This article was medically reviewed by Sarah Gehrke, RN, MS. Sarah Gehrke is a Registered Nurse and Licensed Massage Therapist in Texas. Sarah has over 10 years of experience teaching and practicing phlebotomy and intravenous (IV) therapy using physical, psychological, and emotional support. She received her Massage Therapist License from the Amarillo Massage Therapy Institute in 2008 and a M.S. in Nursing from the University of Phoenix in 2013.
There are 11 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 117,455 times.
Eliquis is an anticoagulant, so if you're on it, it's likely because you are at an elevated risk for a stroke or blood clots.[1] Therefore, you shouldn't go off the medication without first talking to your healthcare provider. That said, you may need to change to another treatment because of adverse side effects, or you may need to stop Eliquis temporarily before having surgery. No matter the reason, talk to your healthcare provider about stopping or changing the medication before doing so.
Steps
Stopping Eliquis for Surgery
-
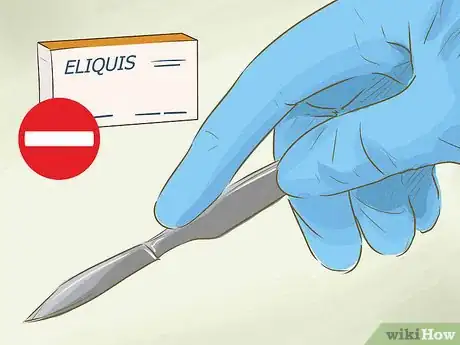
1Stay on Eliquis until your healthcare provider tells you to get off. Suddenly stopping Eliquis can cause serious issues. For instance, you could have a stroke or a blood clot, leading to major damage. Always consult your healthcare provider first.
-
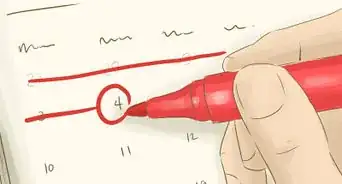
2Stop Eliquis 1- 2 days before medical procedures. Generally, you need to get off this medication a day before most medical procedures, including surgeries and dental work. However, you should call your healthcare provider before you stop taking this medication. Your healthcare provider can advise you on what to do before the procedure. Talk to your surgeon first, but it's also a good idea to talk to your regular doctor, as well.[2]
- If the procedure has a higher risk of bleeding, you may need to stop it 2 days before.[3]
- Examples of surgeries with a higher risk of bleeding include kidney biopsies and coronary artery bypass surgery. Also, any surgery that's expected to be over 45 minutes falls into this category.
- Examples of lower risk surgeries include carpal tunnel repair, abdominal hysterectomy, and cholecystectomy.[4]
Advertisement -
3Stop Eliquis earlier if you have higher serum creatinine levels. If your serum creatinine levels are higher than 1.5 milligrams/dL, you'll need to stop 2 days ahead for a procedure with standard risk for bleeding. You'll need to stop 3 days ahead for procedures that are high risk for bleeding.[5]
- Your serum creatinine levels can be determined by a blood test, which your healthcare provider can perform. Generally, you'll only need this test if you are having kidney problems, too, who will likely be monitoring these levels regularly, anyway.
-
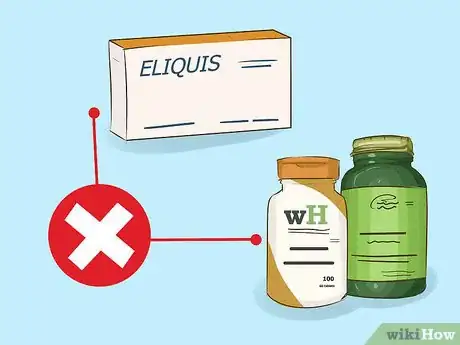
4Don't bridge with an alternative medication. You generally shouldn't need another medication or device to help with anti-coagulation between when you stop Eliquis and when you have your procedure. However, talk to your healthcare provider to determine if that's correct for you.[6]
-
5Start Eliquis again after the procedure. Once the procedure is done, you can start taking Eliquis again. However, you must wait until any bleeding has stopped and your blood is clotting properly before beginning the medication again. Your surgeon or healthcare provider should give you the go ahead.[7]
Changing to an Alternative
-
1Switch to an alternative medication or device as needed. If you can't be on Eliquis for some reason, you'll likely need to be on an alternative. Alternatives like the drug warfarin or a device known as the Watchman may be solutions.[8]
-
2Try the Watchman if blood thinners aren't working for you. This medical device fits into your left atrial appendage, where blood clots tend to form. It stops blood clots from escaping this area by closing it off. However, because medical procedures can be risky, you should stay on blood thinners like Eliquis if they are currently working for you instead of switching.[9]
- The Watchman is a catheter threaded through a vein in the leg. It goes all the way to your heart. It's been proven to be as effective as warfarin at preventing blood clots.
- Typically, you'll stop your blood thinner just for the procedure, and then you'll be on it again for a month and a half after the Watchman is inserted. That's how long it takes for the procedure to fully close off the area that has the potential to release blood clots.
-
3Consider warfarin. Warfarin is an older drug than Eliquis, but it does work well for some people. When switching to warfarin, you'll start taking warfarin, and then on the third day after you begin taking warfarin, you'll stop taking Eliquis.[10]
- Warfarin can have similar side effects to Eliquis, including severe bleeding, bloody urine or stools, bruising, dizziness, weakness, joint pain, and bloody vomit.[11]
Watching for Side Effects that May Require Stopping Eliquis
-
1Look for signs of internal bleeding. Because Eliquis is a blood thinner, 1 of the side effects can be internal bleeding. For instance, you may notice red or especially dark urine, vomit, or feces, all of which indicate blood. Similarly, if you get a cut and can't stop bleeding within 10 minutes, that's also a noteworthy side effect.
- Visit the emergency room if you have one of these symptoms.
- Heavier periods and unexplained bruising can also be side effects, though they aren't quite as serious. They don't warrant a visit to the ER, but you should call your healthcare provider.
-
2Pay attention to signs of an allergic reaction. Eliquis can also cause what appears to be an allergic reaction. You may have chest pain, dizziness, swelling in your face or tongue, or trouble breathing.[12]
- Call emergency services if you experience these symptoms.
-
3Check for signs of a stroke. Eliquis can put you at higher risk of a stroke, particularly if you stop it suddenly. Signs of a stroke include difficulty speaking, drooping in your face, weakness in a limb, dizziness, loss of vision, and headaches.[13]
- Dial emergency services for these symptoms.
-
4Watch for falls that cause a bump to the head. Serious falls, particularly ones where you hit your head, are more of a problem when you're on Eliquis. You are more likely to bleed internally when you have a fall on Eliquis. Always pay attention to more serious falls, and visit the emergency room just in case.
-
5Pay attention to unexpected pain or swelling. Another serious side effect of this drug can be sudden pain anywhere in your body or swelling. Particularly notice sudden pain in your joints. These symptoms also warrant an emergency room visit.[14]
- This side effect could be caused by internal bleeding.
-
6Talk to your healthcare provider about quitting Eliquis. If you have any of these symptoms, you're probably going to need to go off Eliquis. However, you'll need to do it under your healthcare provider’s supervision, as quitting suddenly can increase your chances of a stroke or blood clot.
References
- ↑ https://www.accessdata.fda.gov/drugsatfda_docs/label/2012/202155s000lbl.pdf
- ↑ https://healthonline.washington.edu/document/health_online/pdf/Treatment-Apixaban.pdf
- ↑ https://packageinserts.bms.com/pi/pi_eliquis.pdf
- ↑ https://www.uptodate.com/contents/perioperative-management-of-patients-receiving-anticoagulants#H7
- ↑ https://packageinserts.bms.com/pi/pi_eliquis.pdf
- ↑ https://packageinserts.bms.com/pi/pi_eliquis.pdf
- ↑ https://packageinserts.bms.com/pi/pi_eliquis.pdf
- ↑ https://www.health.harvard.edu/heart-health/afib-stroke-prevention-go-set-a-watchman
- ↑ https://www.watchman.com/en-us/how-watchman-device-works.html
- ↑ https://depts.washington.edu/anticoag/home/content/suggestions-conversion-tofrom-apixaban
- ↑ https://www.mayoclinic.org/diseases-conditions/deep-vein-thrombosis/in-depth/warfarin-side-effects/art-20047592
- ↑ http://www.med.umich.edu/1libr/AntiCoag/Apixaban.pdf
- ↑ http://www.med.umich.edu/1libr/AntiCoag/Apixaban.pdf
- ↑ https://www.fda.gov/downloads/Drugs/DrugSafety/UCM333961.pdf
About This Article
If you need to stop taking Eliquis, ask your doctor first, since changing your medication could be dangerous. If you experience side effects like bloody urine or feces, chest pain, dizziness, swelling in your face, or if you have a stroke, stop taking Eliquis and go to the hospital immediately. Then, consult your doctor. If you’re allergic to the drug or it’s causing you other issues, your doctor may change you to a different medication, like warfarin or a device called the Watchman, which limits blood clots. If you need to stop taking Eliquis before surgery, stop 1 or 2 days before the operation and resume taking it right after. You shouldn't need to take alternative medication before surgery, but your doctor should advise you about this. For more tips from our Medical co-author, including how to stop taking Eliquis if you have high serum creatinine levels, read on.