Actinomycosis
Actinomycosis is a rare infectious bacterial disease caused by Actinomyces species.[1] The name refers to ray-like appearance of the organisms in the granules. About 70% of infections are due to either Actinomyces israelii or A. gerencseriae.[1] Infection can also be caused by Streptomyces somaliensis and Propionibacterium propionicus. The condition is likely to be a polymicrobial anaerobic infection.[2]
| Actinomycosis | |
|---|---|
 | |
| A man with actinomycosis on the right side of his face | |
| Specialty | Infectious disease |
Signs and symptoms
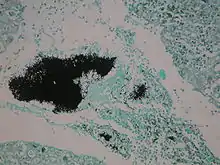
The disease is characterised by the formation of painful abscesses in the mouth, lungs,[3][4] breast,[5] or gastrointestinal tract.[2] Actinomycosis abscesses grow larger as the disease progresses, often over months. In severe cases, they may penetrate the surrounding bone and muscle to the skin, where they break open and leak large amounts of pus, which often contains characteristic granules filled with progeny bacteria. These granules are often called "sulfur granules" due to their yellow appearance, although they may also be white, gray or brown.[6]
Causes

Actinomycosis is primarily caused by any of several members of the bacterial genus Actinomyces. These bacteria are generally anaerobes.[7] In animals, they normally live in the small spaces between the teeth and gums, causing infection only when they can multiply freely in anoxic environments. An affected human often has recently had dental work, poor oral hygiene, periodontal disease, radiation therapy, or trauma (broken jaw) causing local tissue damage to the oral mucosa, all of which predispose the person to developing actinomycosis. A. israelii is a normal commensal species part of the microbiota species of the lower reproductive tract of women.[8] They are also normal commensals among the gut flora of the caecum; thus, abdominal actinomycosis can occur following removal of the appendix. The three most common sites of infection are decayed teeth, the lungs, and the intestines. Actinomycosis infections are typically polymicrobial, containing additional bacterial species; as Actinomyces itself has little invasive ability, these other species often aid in the infection process.[9]
Diagnosis
The diagnosis of actinomycosis can be a difficult one to make. In addition to microbiological examinations, magnetic resonance imaging and immunoassays may be helpful.[10]
Treatment
Actinomyces bacteria are generally sensitive to penicillin, which is frequently used to treat actinomycosis. In cases of penicillin allergy, doxycycline is used. Sulfonamides such as sulfamethoxazole may be used as an alternative regimen at a total daily dosage of 2–4 grams. Response to therapy is slow and may take months. Hyperbaric oxygen therapy may also be used as an adjunct to conventional therapy when the disease process is refractory to antibiotics and surgical treatment.[11][12]
Epidemiology
Disease incidence is greater in males between the ages of 20 and 60 years than in females.[13] Before antibiotic treatments became available, the incidence in the Netherlands and Germany was one per 100,000 people/year. Incidence in the U.S. in the 1970s was one per 300,000 people/year, while in Germany in 1984, it was estimated to be one per 40,000 people/year.[13] The use of intrauterine devices (IUDs) has increased incidence of genitourinary actinomycosis in females. Incidence of oral actinomycosis, which is harder to diagnose, has increased.[13]
History
In 1877, pathologist Otto Bollinger described the presence of A. bovis in cattle, and shortly afterwards, James Israel discovered A. israelii in humans. In 1890, Eugen Bostroem isolated the causative organism from a culture of grain, grasses, and soil. After Bostroem's discovery, a general misconception existed that actinomycosis was a mycosis that affected individuals who chewed grass or straw. The pathogen is still known as the “great masquerader".[14] Bergey's Manual of Systematic Bacteriology classified the organism as bacterial in 1939,[15] but the disease remained classified as a fungus in the 1955 edition of the Control of Communicable Diseases in Man.[16]
Violinist Joseph Joachim died of actinomycosis on 15 August 1907. The Norwegian painter Halfdan Egedius died from actinomycosis on 2 February 1899.
Other animals
Actinomycosis occurs rarely in humans, but rather frequently in cattle as a disease called "lumpy jaw". This name refers to the large abscesses that grow on the head and neck of the infected animal. It can also affect swine, horses, and dogs, and less often wild animals and sheep.
References
- Valour F, Sénéchal A, Dupieux C, Karsenty J, Lustig S, Breton P, Gleizal A, Boussel L, Laurent F, Braun E, Chidiac C, Ader F, Ferry T (2014). "Actinomycosis: etiology, clinical features, diagnosis, treatment, and management". Infect Drug Resist. 7: 183–97. doi:10.2147/IDR.S39601. PMC 4094581. PMID 25045274.
- Bowden GHW (1996). Baron S; et al. (eds.). Actinomycosis in: Baron's Medical Microbiology (4th ed.). Univ of Texas Medical Branch. ISBN 978-0-9631172-1-2. (via NCBI Bookshelf).
- Brook, I (Oct 2008). "Actinomycosis: diagnosis and management". Southern Medical Journal. 101 (10): 1019–23. doi:10.1097/SMJ.0b013e3181864c1f. PMID 18791528. S2CID 19554893.
- Mabeza, GF; Macfarlane J (March 2003). "Pulmonary actinomycosis". European Respiratory Journal. 21 (3): 545–551. doi:10.1183/09031936.03.00089103. PMID 12662015.
- Abdulrahman, Ganiy Opeyemi; Gateley, Christopher Alan (1 January 2015). "Primary actinomycosis of the breast caused by Actinomyces turicensis with associated Peptoniphilus harei". Breast Disease. 35 (1): 45–47. doi:10.3233/BD-140381. PMID 25095985.
- Kliegman, Robert M.; St. Geme, Joseph W., III (2019). Nelson Textbook of Pediatrics. Elsevier Health Sciences. p. 1466. ISBN 9780323568883.
- Ryan KJ; Ray CG, eds. (2004). Sherris Medical Microbiology (4th ed.). McGraw Hill. ISBN 978-0-8385-8529-0.
- Hoffman, Barbara (2012). Williams gynecology (2nd ed.). New York: McGraw-Hill Medical. p. 42. ISBN 978-0071716727.
- Schaal, Klaus P.; Yassin, Atteyet F.; Stackebrandt, E. R. K. O. (2006). "The Family Actinomycetaceae: The Genera Actinomyces, Actinobaculum, Arcanobacterium, Varibaculum, and Mobiluncus". Prokaryotes. Vol. 3. p. 485. doi:10.1007/0-387-30743-5_21. ISBN 9780387254937.
- Böhm, Ingrid; Willinek, Winfried; Schild, Hans H. (October 2006). "Magnetic Resonance Imaging Meets Immunology: An Unusual Combination of Diagnostic Tools Leads to the Diagnosis Actinomycosis". The American Journal of Gastroenterology. 101 (10): 2439–2440. PMID 17032212.
- "Bone Infections". MedlinePlus. US National Library of Medicine. Retrieved 16 August 2015.
- "Osteomyelitis (Refractory)". Undersea and Hyperbaric Medical Society. Retrieved 16 August 2015.
- Wolff K, Goldsmith LA, Katz S, Gilchrist BA, Paller A, Leffell DJ (2007). Fitzpatrick's Dermatology in General Medicine (7th ed.). McGraw Hill.
- Sullivan, D. C.; Chapman, S. W. (12 May 2010). "Bacteria That Masquerade as Fungi: Actinomycosis/Nocardia". Proceedings of the American Thoracic Society. 7 (3): 216–221. doi:10.1513/pats.200907-077AL. PMID 20463251.
- Strong, Richard (1944). Stitt's Diagnosis, Prevention and Treatment of Tropical Diseases (7th ed.). p. 1182.
- Control of Communicable Diseases in Man (8th ed.). American Public Health Association. 1955.
Further reading
- Anderson, Clifton W.; Jenkins, Ralph H. (December 15, 1938). "Actinomycosis of the Scrotum". New England Journal of Medicine. 219 (24): 953–954. doi:10.1056/NEJM193812152192403.
- Codman, E. A. (August 11, 1898). "A Case of Actinomycosis". The Boston Medical and Surgical Journal. 139 (6): 134–135. doi:10.1056/NEJM189808111390606.
- Randolph HL Wong; Alan DL Sihoe; KH Thung; Innes YP Wan; Margaret BY Ip; Anthony PC Yim (June 2004). "Actinomycosis: an often forgotten diagnosis". Asian Cardiovasc Thorac Ann. 12 (2): 165–7. doi:10.1177/021849230401200218. PMID 15213087. S2CID 9930882. Review
- Munro, John C. (September 13, 1900). "Four Cases of Actinomycosis". The Boston Medical and Surgical Journal. 143 (11): 255–256. doi:10.1056/NEJM190009131431103.
- Whitney, W. F. (June 5, 1884). "A Case of Actinomycosis in a Heifer". The Boston Medical and Surgical Journal. 110 (23): 532. doi:10.1056/NEJM188406051102302.
.jpg.webp)
.jpg.webp)
.jpg.webp)
.jpg.webp)
.jpg.webp)