Autism spectrum
The autism spectrum is a range of neurodevelopmental conditions generally characterized by difficulties in social interactions and communication, repetitive behaviors, intense interests, and unusual responses to sensory stimuli. It is commonly referred to as autism or, in the context of a professional diagnosis, autism spectrum disorder (ASD).
| Autism spectrum | |
|---|---|
| Other names | Autism, Autism spectrum condition (ASC), Autism spectrum disorder (ASD) |
 | |
| Repetitively stacking or lining up objects is a common trait associated with autism. | |
| Specialty | Psychiatry, Clinical psychology, pediatrics, occupational medicine |
| Symptoms | Difficulties in social interaction, verbal and nonverbal communication, and the presence of intense interests and repetitive behavior |
| Complications | Social isolation, educational and employment problems,[1] anxiety,[1] stress,[1] bullying,[1] self-harm |
| Onset | Early childhood |
| Duration | Lifelong |
| Causes | Multi-factorial, with many uncertain factors |
| Risk factors | Family history, certain genetic conditions, having older parents, certain prescribed drugs, perinatal and neonatal health issues |
| Diagnostic method | Based on combination of clinical observation of behavior and development and comprehensive diagnostic testing completed by a team of qualified professionals (including clinical psychologists, neuropsychologists, pediatricians, and speech-language pathologists) |
| Differential diagnosis | Intellectual disability, anxiety, depression, Rett syndrome, attention deficit hyperactivity disorder, schizoid personality disorder, selective mutism, schizophrenia, obsessive compulsive disorder, social phobia, Einstein syndrome, learning disorders (mainly speech disorders), social anxiety |
| Management | Speech therapy, Occupational therapy, Behavioral therapy, psychotropic medication |
| Frequency |
|
A spectrum disorder is one that can manifest very differently from person to person: any given person with the disorder is likely to show some but not all of the characteristics associated with it, and may show them to very different degrees. Different autistic people might show strikingly different characteristics, and the same person might also present differently at different times.[2] Historically, the autism spectrum was divided into sub-categories, but questions persisted over the validity of these divisions.[2][3] The most recent editions of the major English-language diagnostic manuals, Diagnostic and Statistical Manual of Mental Disorders (DSM-5-TR, published in 2022) and International Classification of Diseases (ICD-11, released in 2021) both list ASD as a single disorder.[4][5]
While psychiatry traditionally classifies autism as a neurodevelopmental disorder, many autistic people, most autistic advocates and a rapidly increasing number of researchers see autism as part of neurodiversity, the natural diversity in human thinking, and experience, with strengths, differences, and weaknesses.[6] On this view, promoted by the autism rights movement, autism is not pathological, but this does not preclude autistic individuals from being disabled and potentially having high support needs due to co-occurring conditions and lack of person-environment fit.[7] This relatively positive and holistic view of autism has led to a certain degree of friction between autistic individuals, advocates, charities, researchers and practitioners.[8][9][10]
Other controversies in autism are scientific, sociological, political, or philosophical, and some have aspects of all four. First, it is controversial and uncertain if social-communication difficulties of autistic people are inherent core deficits (see empathizing-systemizing theory developed by Simon Baron-Cohen),[11] or due to mismatch in social communication styles, cognition, and experiences resulting in bidirectional misunderstanding between autistic people and non-autistic people (see double empathy problem theory developed by autistic researcher Damien Milton and recent growing evidence that found that autistic people empathize, communicate and socialize well with autistic people),[12][13] or a combination of both factors. A 2018 study has shown that autistic people are more prone to object personification,[14] suggesting that autistic empathy may be not only more complex but also more all-encompassing, contrary to the popular belief that autistic people lack empathy. However, most studies have found no evidence of impairment in autistic individuals' ability to understand other people's basic intentions or goals; instead, data suggests that impairments are found in understanding more complex social emotions or in considering others' viewpoints.[15]
Scientists are still trying to determine what causes autism; it is highly heritable and believed to be mainly genetic, but there are many genes involved, and environmental factors may also be relevant.[16] There is also no cure for autism, so interventions focus on, for example, finding and learning other modes of communication in a non-verbal autistic person, or applied behavior analysis interventions. It is unclear why autism commonly co-occurs with ADHD, epilepsy and a range of other conditions. There are ongoing disagreements about what should be included as part of the autism spectrum, whether meaningful sub-types of autism exist,[3] and the significance of autism-associated traits in the wider population.[17][18] The combination of broader criteria and increased awareness has led to a trend of steadily increasing estimates of autism prevalence, causing a common misconception that there is an autism epidemic[19] and perpetuating the myth that it is caused by vaccines.[20]
Classification
Spectrum model
Autism is a highly variable neurodevelopmental disorder[21] and has long been thought to cover a wide spectrum, ranging from individuals with high support needs (who may be non-speaking, experience developmental delay, and be more likely to present with other co-existing diagnoses including intellectual disability) to individuals with low support needs (who may have more typical speech-language and intellectual skills but atypical social/conversation skills, narrowly focused interests, and wordy, pedantic communication).[22] Because the behavior spectrum is continuous, boundaries between diagnostic categories are somewhat arbitrary.[23]
ICD
The World Health Organization's International Classification of Diseases (11th Revision) ICD-11, regarded as the global standard, was released in June 2018 and came into full effect as of January 2022.[24][25] It describes ASD as follows:[26]
Autism spectrum disorder is characterised by persistent deficits in the ability to initiate and to sustain reciprocal social interaction and social communication, and by a range of restricted, repetitive, and inflexible patterns of behaviour, interests or activities that are clearly atypical or excessive for the individual's age and sociocultural context. The onset of the disorder occurs during the developmental period, typically in early childhood, but symptoms may not become fully manifest until later, when social demands exceed limited capacities. Deficits are sufficiently severe to cause impairment in personal, family, social, educational, occupational or other important areas of functioning and are usually a pervasive feature of the individual's functioning observable in all settings, although they may vary according to social, educational, or other context. Individuals along the spectrum exhibit a full range of intellectual functioning and language abilities.
— ICD-11, chapter 6, section A02
ICD-11 was produced by professionals from 55 countries out of the 90 countries involved and is the most widely used reference worldwide. Clinicians use the ICD as a reference for diagnosis and reporting but researchers, particularly in the US, continue to use the Diagnostic and Statistical Manual of Mental Disorders (DSM-5-TR from 2022, DSM-5 from 2013, or their predecessors) as some material is not included in the ICD (the ICD is broader in scope, covering general as well as mental health). There remain differences, for example Rett disorder was included in ASD in the DSM-5 but in the ICD-11 it was excluded and placed in the chapter for Developmental Anomalies. Both the ICD and the DSM have been under revision and there has been collaborative work towards a convergence of the two since 1980 (when DSM-3 was published and ICD-9 was current), including more rigorous biological assessment - in place of historical experience - and a simplification of the system of classification.[25][27][28][29]
DSM
The American Psychiatric Association's Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR), released in 2022, is the current version of the DSM. The fifth edition, DSM-5, released in May 2013, was the first to define ASD as a single diagnosis,[30] which is continued in DSM-5-TR.[4] ASD encompasses previous diagnoses which included Asperger disorder, childhood disintegrative disorder, PDD-NOS, and the range of diagnoses which included the word autism.[31] Rather than distinguishing between these diagnoses, the DSM-5 and DSM-5-TR adopt a dimensional approach to diagnosing disorders that fall underneath the autistic spectrum umbrella in one diagnostic category. Within this category, the DSM-5 and the DSM includes a framework that differentiates each individual by dimensions of symptom severity, as well as by associated features (i.e., the presence of other disorders or factors which likely contribute to the symptoms, other neurodevelopmental or mental disorders, intellectual disability, or language impairment).[4] The symptom domains are social communication and restricted, repetitive behaviors, with the option of a separate severity - the negative impact of the symptoms on the individual - being specified for each domain, rather than an overall severity.[32] Prior to the DSM-5, the DSM separated social deficits and communication deficits into two domains.[33] Further, the DSM-5 changed to an onset age in the early developmental period, with a note that symptoms may manifest later when social demands exceed capabilities, rather than the previous, more restricted 3 years of age.[34] These changes continue in the DSM-5-TR.[4]
Features and characteristics
For many autistic individuals, characteristics first appear during infancy or childhood and generally follow a steady course without remission (different developmental timelines described in more detail below).[35] Autistic people may be severely impaired in some respects but average, or even superior, in others.[36][37][38]
Clinicians consider assessment for ASD when a patient shows:
- regular difficulties in social interaction or communication
- restricted or repetitive behaviors (often called "stimming")
- resistance to changes or restricted interests
These features are typically assessed with the following, when appropriate:
- problems in obtaining or sustaining employment or education
- difficulties in initiating or sustaining social relationships
- connections with mental health or learning disability services
- a history of neurodevelopmental conditions (including learning disabilities and ADHD) or mental health conditions.[39][40]
There are many signs associated with ASD; the presentation varies widely:[41][42]
Common signs for autistic spectrum disorder - avoidance of eye-contact
- little or no babbling as an infant
- not showing interest in indicated objects
- delayed language skills (e.g. having a smaller vocabulary than peers or difficulty expressing themselves in words)
- reduced interest in other children or caretakers, possibly with more interest in objects
- difficulty playing reciprocal games (e.g. peek-a-boo)
- increased sensitivity or unusual response to the smell, texture, sound, taste, or appearance of things
- resistance to changes in routine
- repetitive, limited, or otherwise unusual usage of toys
- repetition of words or phrases (echolalia)
- repetitive motions or movements, including stimming
- self-harming
Atypical eating is also common, but it does not need to be present to make a diagnosis.[43]
In addition, a small percentage of autistic people can exhibit notable ability, for example in mathematics, music or artistic reproduction, which in exceptional cases is referred to as savant syndrome.[44][45]
Developmental course
There are two possible developmental courses of ASD. One course of development is more gradual in nature, with symptoms appearing fairly early in life and persisting.[46] A second course of development is characterized by normal or near-normal development before onset of regression or loss of skills, which is known as regressive autism.[47]
Gradual autism development
Most parents report that the onset of autism features appear within the first year of life.[48][49] This course of development is fairly gradual, in that parents typically report concerns in development over the first two years of life and diagnosis can be made around 3–4 years of age.[46] Overt features gradually begin after the age of six months, become established by age two or three years,[50] and tend to continue through adulthood, although often in more muted form.[51] Some of the early signs of ASDs in this course include decreased attention at faces, failure to obviously respond when name is called, failure to show interests by showing or pointing, and delayed imaginative play.[52]
Regressive autism development
Regressive autism occurs when a child appears to develop typically but then starts to lose speech and social skills and is subsequently diagnosed with ASD.[53] Other terms used to describe regression in children with autism are autism with regression, autistic regression, setback-type autism, and acquired autistic syndrome.[54]
Within the regressive autism developmental course, there are two patterns. The first pattern is when developmental losses occur in the first 15 months to 3 years.[55][56] The second pattern, childhood disintegrative disorder (a diagnosis now included under ASD), is characterized by regression after normal development in the first 3 to 4, or even up to 9 years of life.[57]
After the regression, the child follows the standard pattern of autistic neurological development. The term regressive autism refers to the appearance that neurological development has reversed; it is actually only the affected developmental skills, rather than the neurology as a whole, that regresses.
The apparent onset of regressive autism can be surprising and distressing to parents, who often initially suspect severe hearing loss.[58] Attribution of regression to environmental stress factors may result in a delay in diagnosis.[59]
There is no standard definition for regression.[54] Some children show a mixture of features, with some early delays and some later losses; and there is evidence of a continuous spectrum of behaviors, rather than, or in addition to, a black-and-white distinction, between autism with and without regression.[60] There are several intermediate types of development, which do not neatly fit into either the traditional early onset or the regressive categories, including mixtures of early deficits, failures to progress, subtle diminishment, and obvious losses.
Regression may occur in a variety of domains, including communication, social, cognitive, and self-help skills; however, the most common regression is loss of language.[61][55][56] Some children lose social development instead of language; some lose both.[60] Skill loss may be quite rapid, or may be slow and preceded by a lengthy period of no skill progression; the loss may be accompanied by reduced social play or increased irritability.[54] The temporarily acquired skills typically amount to a few words of spoken language, and may include some rudimentary social perception.[60]
The prevalence of regression varies depending on the definition used.[60] If regression is defined strictly to require loss of language, it is less common; if defined more broadly, to include cases where language is preserved but social interaction is diminished, it is more common.[60] Though regressive autism is often thought to be a less common (compared with gradual course of autism onset described above), this is an area of ongoing debate;[62] some evidence suggests that a pattern of regressive autism may be more common than previously thought.[63] There are some who believe that regressive autism is simply early-onset autism which was recognized at a later date. Researchers have conducted studies to determine whether regressive autism is a distinct subset of ASD, but the results of these studies have contradicted one another.[53]
Differential outcomes
There continues to be a debate over the differential outcomes based on these two developmental courses. Some studies suggest that regression is associated with poorer outcomes and others report no differences between those with early gradual onset and those who experience a regression period.[64] While there is conflicting evidence surrounding language outcomes in autism, some studies have shown that cognitive and language abilities at age 2+1⁄2 may help predict language proficiency and production after age 5.[65] Overall, the literature stresses the importance of early intervention in achieving positive longitudinal outcomes.[66]
Social and communication skills
In social contexts, autistic people may respond and behave differently than individuals without ASD.[67]
Impairments in social skills present many challenges for autistic individuals. Deficits in social skills may lead to problems with friendships, romantic relationships, daily living, and vocational success.[68] One study that examined the outcomes of autistic adults found that, compared to the general population, autistic people were less likely to be married, but it is unclear whether this outcome was due to deficits in social skills or intellectual impairment, or some other reason.[69] A factor to this is likely discrimination against autistic people which is perpetuated by myths; for example: the myth that autistic people have no empathy.
Prior to 2013, deficits in social function and communication were considered two separate symptom domains of autism.[70] The current social communication domain criteria for autism diagnosis require individuals to have deficits across three social skills: social-emotional reciprocity, nonverbal communication, and developing and sustaining relationships.[4] Communication deficits are due to problems with social-emotional skills like joint attention and social reciprocity.
A range of social-emotional reciprocity difficulties (an individual's ability to naturally engage in social interactions) may be present. Autistic individuals may lack mutual sharing of interests, for example many autistic children prefer not to play or interact with others. They may lack awareness or understanding of other people's thoughts or feelings – a child may get too close to peers (entering their personal space) without noticing that this makes them uncomfortable. They may also engage in atypical behaviors to gain attention, for example a child may push a peer to gain attention before starting a conversation.[71]
Older children and adults with ASD perform worse on tests of face and emotion recognition than non-autistic individuals, although this may be partly due to a lower ability to define a person's own emotions.[72]
Autistic people experience deficits in their ability to develop, maintain, and understand relationships, as well as difficulties adjusting behavior to fit social contexts.[73] ASD presents with impairments in pragmatic communication skills, such as difficulty initiating a conversation or failure to consider the interests of the listener to sustain a conversation.[71] The ability to be focused exclusively on one topic in communication is known as monotropism, and can be compared to "tunnel vision". It is common for autistic individuals to communicate strong interest in a specific topic, speaking in lesson-like monologues about their passion instead of enabling reciprocal communication with whomever they are speaking to.[74] What may look like self-involvement or indifference toward others stems from a struggle to recognize or remember that other people have their own personalities, perspectives, and interests.[75][76] Another difference in pragmatic communication skills is that autistic people may not recognize the need to control the volume of their voice in different social settings – for example, they may speak loudly in libraries or movie theaters.[77]
Autistic people display atypical nonverbal behaviors or have difficulties with nonverbal communication. They may make infrequent eye contact – an autistic child may not make eye contact when called by name, or they may avoid making eye contact with an observer. Aversion of gaze can also be seen in anxiety disorders, however poor eye contact in autistic children is not due to shyness or anxiety; rather, it is overall diminished in quantity. Autistic individuals may struggle with both production and understanding of facial expressions. They often do not know how to recognize emotions from others' facial expressions, or they may not respond with the appropriate facial expressions. They may have trouble recognizing subtle expressions of emotion and identifying what various emotions mean for the conversation.[78][74] A defining feature is that autistic people have social impairments and often lack the intuition about others that many people take for granted. Temple Grandin, an autistic woman involved in autism activism, described her inability to understand the social communication of neurotypicals, or people with typical neural development, as leaving her feeling "like an anthropologist on Mars".[79] They may also not pick up on body language or social cues such as eye contact and facial expressions if they provide more information than the person can process at that time. They struggle with understanding the context and subtext of conversational or printed situations, and have trouble forming resulting conclusions about the content. This also results in a lack of social awareness and atypical language expression.[75] How facial expressions differ between those on the autism spectrum and neurotypical individuals is not clear.[80] Further, at least half of autistic children have unusual prosody.[77]
Autistic people may also experience difficulties with verbal communication. Differences in communication may be present from the first year of life, and may include delayed onset of babbling, unusual gestures, diminished responsiveness, and vocal patterns that are not synchronized with the caregiver. In the second and third years, autistic children have less frequent and less diverse babbling, consonants, words, and word combinations; their gestures are less often integrated with words. Autistic children are less likely to make requests or share experiences, and are more likely to simply repeat others' words (echolalia).[81] Joint attention seems to be necessary for functional speech, and deficits in joint attention seem to distinguish infants with ASD.[59] For example, they may look at a pointing hand instead of the object to which the hand is pointing,[82][81] and they consistently fail to point at objects in order to comment on or share an experience.[59] Autistic children may have difficulty with imaginative play and with developing symbols into language.[81] Some autistic linguistic behaviors include repetitive or rigid language, and restricted interests in conversation. For example, a child might repeat words or insist on always talking about the same subject.[71] Echolalia may also be present in autistic individuals, for example by responding to a question by repeating the inquiry instead of answering.[74] Language impairment is also common in autistic children, but is not part of a diagnosis.[71] Many autistic children develop language skills at an uneven pace where they easily acquire some aspects of communication, while never fully developing others,[74] such as in some cases of hyperlexia. In some cases, individuals remain completely nonverbal throughout their lives. The CDC estimated that around 40% of autistic children don't speak at all, although the accompanying levels of literacy and nonverbal communication skills vary.[83]
Restricted and repetitive behaviors

ASD includes a wide variety of characteristics. Some of these include behavioral characteristics which widely range from slow development of social and learning skills to difficulties creating connections with other people. Autistic individuals may experience these challenges with forming connections due to anxiety or depression, which they are more likely to experience, and as a result isolate themselves.[84]
Other behavioral characteristics include abnormal responses to sensations (such as sights, sounds, touch, taste and smell) and problems keeping a consistent speech rhythm. The latter problem influences an individual's social skills, leading to potential problems in how they are understood by communication partners. Behavioral characteristics displayed by autistic people typically influence development, language, and social competence. Behavioral characteristics of autistic people can be observed as perceptual disturbances, disturbances of development rate, relating, speech and language, and motility.[85]
The second core symptom of autism spectrum is a pattern of restricted and repetitive behaviors, activities, and interests. In order to be diagnosed with ASD under DSM-5 or DSM-5-TR, a person must have at least two of the following behaviors:[4][86]
- Repetitive behaviors – Repetitive behaviors such as rocking, hand flapping, finger flicking, head banging, or repeating phrases or sounds.[71] These behaviors may occur constantly or only when the person gets stressed, anxious or upset.
- Resistance to change – A strict adherence to routines such as eating certain foods in a specific order, or taking the same path to school every day.[71] The child may have a meltdown if there is any change or disruption to their routine.
- Restricted interests – An excessive interest in a particular activity, topic, or hobby, and devoting all their attention to it. For example, young children might completely focus on things that spin and ignore everything else. Older children might try to learn everything about a single topic, such as the weather or sports, and perseverate or talk about it constantly.[71]
- Sensory reactivity– An unusual reaction to certain sensory inputs such as having a negative reaction to specific sounds or textures, being fascinated by lights or movements or having an apparent indifference to pain or heat.[87]
Autistic individuals can display many forms of repetitive or restricted behavior, which the Repetitive Behavior Scale-Revised (RBS-R) categorizes as follows.[88]
- Stereotyped behaviors: Repetitive movements, such as hand flapping, head rolling, or body rocking.
- Compulsive behaviors: Time-consuming behaviors intended to reduce anxiety, that an individual feels compelled to perform repeatedly or according to rigid rules, such as placing objects in a specific order, checking things, or handwashing.
- Sameness: Resistance to change; for example, insisting that the furniture not be moved or refusing to be interrupted.
- Ritualistic behavior: Unvarying pattern of daily activities, such as an unchanging menu or a dressing ritual. This is closely associated with sameness and an independent validation has suggested combining the two factors.[88]
- Restricted interests: Interests or fixations that are abnormal in theme or intensity of focus, such as preoccupation with a single television program, toy, or game.
- Self-injury: Behaviors such as eye-poking, skin-picking, hand-biting and head-banging.[59]
Self-injury
Self-injurious behaviors (SIB) are relatively common in autistic people, and can include head-banging, self-cutting, self-biting, and hair-pulling.[89] Some of these behaviors can result in serious injury or death.[89] Following are theories about the cause of self-injurious behavior in children with developmental delay, including autistic individuals:[90]
- Frequency and/or continuation of self-injurious behavior can be influenced by environmental factors (e.g. reward in return for halting self-injurious behavior). However this theory is not applicable to younger children with autism. There is some evidence that frequency of self-injurious behavior can be reduced by removing or modifying environmental factors that reinforce this behavior.[90]: 10–12
- Higher rates of self-injury are also noted in socially isolated individuals with autism. Studies have shown that socialization skills are related factors to self injurious behavior for individuals with autism.[91]
- Self-injury could be a response to modulate pain perception when chronic pain or other health problems that cause pain are present.[90]: 12–13
- An abnormal basal ganglia connectivity may predispose to self-injurious behavior.[90]: 13
Other features
Autistic individuals may have symptoms that do not contribute to the official diagnosis, but that can affect the individual or the family.[43] Some individuals with ASD show unusual abilities, ranging from splinter skills (such as the memorization of trivia) to the rare talents of autistic savants.[92] One study describes how some individuals with ASD show superior skills in perception and attention, relative to the general population.[93] Sensory abnormalities are found in over 90% of autistic people, and are considered core features by some.[23] Differences between the previously recognized disorders under the autism spectrum are greater for under-responsivity (for example, walking into things) than for over-responsivity (for example, distress from loud noises) or for sensation seeking (for example, rhythmic movements).[94] An estimated 60–80% of autistic people have motor signs that include poor muscle tone, poor motor planning, and toe walking;[23][95] deficits in motor coordination are pervasive across ASD and are greater in autism proper.[96] Unusual eating behavior occurs in about three-quarters of children with ASD, to the extent that it was formerly a diagnostic indicator. Selectivity is the most common problem, although eating rituals and food refusal also occur.[97]
There is tentative evidence that gender dysphoria occurs more frequently in autistic people (see Autism and LGBT identities).[98][99] As well as that, a 2021 anonymized online survey of 16–90 year-olds revealed that autistic males are more likely to identify as bisexual, while autistic females are more likely to identify as homosexual.[100]
Gastrointestinal problems are one of the most commonly co-occurring medical conditions in autistic people.[101] These are linked to greater social impairment, irritability, language impairments, mood changes, and behavior and sleep problems.[101][102]
Parents of children with ASD have higher levels of stress.[82] Siblings of children with ASD report greater admiration and less conflict with the affected sibling than siblings of unaffected children and were similar to siblings of children with Down syndrome in these aspects of the sibling relationship. However, they reported lower levels of closeness and intimacy than siblings of children with Down syndrome; siblings of individuals with ASD have greater risk of negative well-being and poorer sibling relationships as adults.[103]
Causes
It had long been presumed that there is a common cause at the genetic, cognitive, and neural levels for the social and non-social components of autism's symptoms, described as a triad in the classic autism criteria.[104] However, there is increasing suspicion that autism is instead a complex disorder whose core aspects have distinct causes that often co-occur.[104][105] While it is unlikely that a single cause for ASD exists,[105] many risk factors identified in the research literature may contribute to ASD development. These risk factors include genetics, prenatal and perinatal factors (meaning factors during pregnancy or very early infancy), neuroanatomical abnormalities, and environmental factors. It is possible to identify general factors, but much more difficult to pinpoint specific factors. Given the current state of knowledge, prediction can only be of a global nature and therefore requires the use of general markers.[106]
Biological subgroups
Research into causes has been hampered by the inability to identify biologically meaningful subgroups within the autistic population[107] and by the traditional boundaries between the disciplines of psychiatry, psychology, neurology and pediatrics.[108] Newer technologies such as fMRI and diffusion tensor imaging can help identify biologically relevant phenotypes (observable traits) that can be viewed on brain scans, to help further neurogenetic studies of autism;[109] one example is lowered activity in the fusiform face area of the brain, which is associated with impaired perception of people versus objects.[110] It has been proposed to classify autism using genetics as well as behavior.[111] (For more, see Brett Abrahams)
Genetics

Autism has a strong genetic basis, although the genetics of autism are complex and it is unclear whether ASD is explained more by rare mutations with major effects, or by rare multi-gene interactions of common genetic variants.[113][114] Complexity arises due to interactions among multiple genes, the environment, and epigenetic factors which do not change DNA sequencing but are heritable and influence gene expression.[51] Many genes have been associated with autism through sequencing the genomes of affected individuals and their parents.[115] However, most of the mutations that increase autism risk have not been identified. Typically, autism cannot be traced to a Mendelian (single-gene) mutation or to a single chromosome abnormality, and none of the genetic syndromes associated with ASD have been shown to selectively cause ASD.[113] Numerous candidate genes have been located, with only small effects attributable to any particular gene.[113] Most loci individually explain less than 1% of cases of autism.[116] As of 2018, it appeared that between 74% and 93% of ASD risk is heritable.[86] After an older child is diagnosed with ASD, 7–20% of subsequent children are likely to be as well.[86] If parents have one autistic child, they have a 2% to 8% chance of having a second child who is also autistic. If the autistic child is an identical twin the other will be affected 36 to 95 percent of the time. If they are fraternal twins the other will only be affected up to 31 percent of the time. The large number of autistic individuals with unaffected family members may result from spontaneous structural variation, such as deletions, duplications or inversions in genetic material during meiosis.[117][118] Hence, a substantial fraction of autism cases may be traceable to genetic causes that are highly heritable but not inherited: that is, the mutation that causes the autism is not present in the parental genome.[119]
As of 2018, understanding of genetic risk factors had shifted from a focus on a few alleles to an understanding that genetic involvement in ASD is probably diffuse, depending on a large number of variants, some of which are common and have a small effect, and some of which are rare and have a large effect. The most common gene disrupted with large effect rare variants appeared to be CHD8, but less than 0.5% of autistic people have such a mutation. The gene CHD8 encodes the protein chromodomain helicase DNA binding protein 8, which is a chromatin regulator enzyme that is essential during fetal development, CHD8 is an ATP dependent enzyme.[120][121][122] The protein contains an Snf2 helicase domain that is responsible for the hydrolysis of ATP to ADP.[122] CHD8 encodes for a DNA helicase that function as a transcription repressor by remodeling chromatin structure by altering the position of nucleosomes. CHD8 negatively regulates Wnt signaling. Wnt signaling is important in the vertebrate early development and morphogenesis. It is believed that CHD8 also recruits the linker histone H1 and causes the repression of β-catenin and p53 target genes.[120] The importance of CHD8 can be observed in studies where CHD8-knockout mice died after 5.5 embryonic days because of widespread p53 induced apoptosis. Some studies have determined the role of CHD8 in autism spectrum disorder (ASD). CHD8 expression significantly increases during human mid-fetal development.[120] The chromatin remodeling activity and its interaction with transcriptional regulators have shown to play an important role in ASD aetiology.[121] The developing mammalian brain has a conserved CHD8 target regions that are associated with ASD risk genes.[123] The knockdown of CHD8 in human neural stem cells results in dysregulation of ASD risk genes that are targeted by CHD8.[124] Recently CD8 has been associated to the regulation of long non-coding RNAs (lncRNAs),[125] and the regulation of X chromosome inactivation (XCI) initiation, via regulation of Xist long non-coding RNA, the master regulator of XCI, though competitive binding to Xist regulatory regions.[126]
Some ASD is associated with clearly genetic conditions, like fragile X syndrome; however, only around 2% of autistic people have fragile X.[86] Hypotheses from evolutionary psychiatry suggest that these genes persist because they are linked to human inventiveness, intelligence or systemising.[127][128]
Current research suggests that genes that increase susceptibility to ASD are ones that control protein synthesis in neuronal cells in response to cell needs, activity and adhesion of neuronal cells, synapse formation and remodeling, and excitatory to inhibitory neurotransmitter balance. Therefore, despite up to 1000 different genes thought to contribute to increased risk of ASD, all of them eventually affect normal neural development and connectivity between different functional areas of the brain in a similar manner that is characteristic of an ASD brain. Some of these genes are known to modulate production of the GABA neurotransmitter which is the main inhibitory neurotransmitter in the nervous system. These GABA-related genes are under-expressed in an ASD brain. On the other hand, genes controlling expression of glial and immune cells in the brain e.g. astrocytes and microglia, respectively, are over-expressed which correlates with increased number of glial and immune cells found in postmortem ASD brains. Some genes under investigation in ASD pathophysiology are those that affect the mTOR signaling pathway which supports cell growth and survival.[129]
All these genetic variants contribute to the development of the autistic spectrum; however, it cannot be guaranteed that they are determinants for the development.[130]
Autism may be under-diagnosed in women and girls due to an assumption that it is primarily a male condition,[131] but genetic phenomena such as imprinting and X linkage have the ability to raise the frequency and severity of conditions in males, and theories have been put forward for a genetic reason why males are diagnosed more often, such as the imprinted brain hypothesis and the extreme male brain theory.[132][133][134]
Early life
Several prenatal and perinatal complications have been reported as possible risk factors for autism. These risk factors include maternal gestational diabetes, maternal and paternal age over 30, bleeding during pregnancy after the first trimester, use of certain prescription medication (e.g. valproate) during pregnancy, and meconium in the amniotic fluid. While research is not conclusive on the relation of these factors to autism, each of these factors has been identified more frequently in children with autism, compared to their siblings who do not have autism, and other typically developing youth.[135] While it is unclear if any single factors during the prenatal phase affect the risk of autism,[136] complications during pregnancy may be a risk.[136]
Low vitamin D levels in early development have been hypothesized as a risk factor for autism.[137]
There are also studies being done to test if certain types of regressive autism have an autoimmune basis.[53]
Maternal nutrition and inflammation during preconception and pregnancy influences fetal neurodevelopment. Intrauterine growth restriction is associated with ASD, in both term and preterm infants.[138] Maternal inflammatory and autoimmune diseases may damage fetal tissues, aggravating a genetic problem or damaging the nervous system.[139]
Exposure to air pollution during pregnancy, especially heavy metals and particulates, may increase the risk of autism.[140][141] Environmental factors that have been claimed without evidence to contribute to or exacerbate autism include certain foods, infectious diseases, solvents, PCBs, phthalates and phenols used in plastic products, pesticides, brominated flame retardants, alcohol, smoking, illicit drugs, vaccines,[142] and prenatal stress. Some, such as the MMR vaccine, have been completely disproven.[143][144][145][146]
Disproven vaccine hypothesis
Parents may first become aware of autistic symptoms in their child around the time of a routine vaccination. This has led to unsupported theories blaming vaccine "overload", a vaccine preservative, or the MMR vaccine for causing autism.[147] In 1998 Andrew Wakefield led a fraudulent, litigation-funded study that suggested that the MMR vaccine may cause autism.[148][149][150][151][152] This conjecture suggested that autism results from brain damage caused either by the MMR vaccine itself, or by thimerosal, a vaccine preservative.[153] No convincing scientific evidence supports these claims,[20] they are biologically implausible,[147] and further evidence continues to refute them, including the observation that the rate of autism continues to climb despite elimination of thimerosal from routine childhood vaccines.[154] A 2014 meta-analysis examined ten major studies on autism and vaccines involving 1.25 million children worldwide; it concluded that neither the MMR vaccine, which has never contained thimerosal,[155] nor the vaccine components thimerosal or mercury, lead to the development of ASDs.[156] Despite this, misplaced parental concern has led to lower rates of childhood immunizations, outbreaks of previously controlled childhood diseases in some countries, and the preventable deaths of several children.[157][158]
Etiological hypotheses
Several hypotheses have been presented that try to explain how and why autism develops by integrating known causes (genetic and environmental effects) and findings (neurobiological and somatic). Some are more comprehensive, such as the Pathogenetic Triad,[159] which proposes and operationalizes three core features (an autistic personality, cognitive compensation, neuropathological burden) that interact to cause autism, and the Intense World Theory,[160] which explains autism through a hyper-active neurobiology that leads to an increased perception, attention, memory, and emotionality. There are also simpler hypotheses that explain only individual parts of the neurobiology or phenotype of autism, such as mind-blindness (a decreased ability for Theory of Mind), the weak central coherence theory, or the extreme male brain and empathising-systemising theory.
Evolutionary hypotheses
Research exploring the evolutionary benefits of autism and associated genes has suggested that autistic people may have played a "unique role in technological spheres and understanding of natural systems" in the course of human development.[161][162] It has been suggested that it may have arisen as "a slight trade off for other traits that are seen as highly advantageous", providing "advantages in tool making and mechanical thinking", with speculation that the condition may "reveal itself to be the result of a balanced polymorphism, like sickle cell anemia, that is advantageous in a certain mixture of genes and disadvantageous in specific combinations".[163]
In 2011, a paper in Evolutionary Psychology proposed that autistic traits, including increased abilities for spatial intelligence, concentration and memory, could have been naturally selected to enable self-sufficient foraging in a more (although not completely) solitary environment, referred to as the "Solitary Forager Hypothesis".[164][165][166] A 2016 paper examines Asperger syndrome as "an alternative pro-social adaptive strategy" which may have developed as a result of the emergence of "collaborative morality" in the context of small-scale hunter-gathering, i.e. where "a positive social reputation for making a contribution to group wellbeing and survival" becomes more important than complex social understanding.[167]
Conversely, some multidisciplinary research suggests that recent human evolution may be a driving force in the rise of a number of medical conditions in recent human populations, including autism. Studies in evolutionary medicine indicate that as biological evolution becomes outpaced by cultural evolution, disorders linked to bodily dysfunction increase in prevalence due to a lack of contact with pathogens and negative environmental conditions that once widely affected ancestral populations. Because natural selection primarily favors reproduction over health and longevity, the lack of this impetus to adapt to certain harmful circumstances creates a tendency for genes in descendant populations to over-express themselves, which may cause a wide array of maladies, ranging from mental illnesses to autoimmune disorders.[168]
Pathophysiology
Autism's symptoms result from maturation-related changes in various systems of the brain.[169] How autism occurs is not well understood. Its mechanism can be divided into two areas: the pathophysiology of brain structures and processes associated with autism, and the neuropsychological linkages between brain structures and behaviors.[169] The behaviors appear to have multiple pathophysiologies.[170]
There is evidence that gut–brain axis abnormalities may be involved.[101][102][171] A 2015 review proposed that immune, gastrointestinal inflammation, malfunction of the autonomic nervous system, gut flora alterations, and food metabolites may cause brain neuroinflammation and dysfunction.[102] A 2016 review concludes that enteric nervous system abnormalities might play a role in neurological disorders such as autism. Neural connections and the immune system are a pathway that may allow diseases originated in the intestine spread to the brain.[171]
Several lines of evidence point to synaptic dysfunction as a cause of autism.[110] Some rare mutations may lead to autism by disrupting some synaptic pathways, such as those involved with cell adhesion.[172] All known teratogens (agents that cause birth defects) related to the risk of autism appear to act during the first eight weeks from conception, and though this does not exclude the possibility that autism can be initiated or affected later, there is strong evidence that autism arises very early in development.[173]
In general, neuroanatomical studies support the concept that autism may involve a combination of brain enlargement in some areas and reduction in others.[174] These studies suggest that autism may be caused by abnormal neuronal growth and pruning during the early stages of prenatal and postnatal brain development, leaving some areas of the brain with too many neurons and other areas with too few neurons.[175] Some research has reported an overall brain enlargement in autism, while others suggest abnormalities in several areas of the brain, including the frontal lobe, the mirror neuron system, the limbic system, the temporal lobe, and the corpus callosum.[176][177]
In functional neuroimaging studies, when performing theory of mind and facial emotion response tasks, the median person on the autism spectrum exhibits less activation in the primary and secondary somatosensory cortices of the brain than the median member of a properly sampled control population. This finding coincides with reports demonstrating abnormal patterns of cortical thickness and grey matter volume in those regions of autistic peoples' brains.[178]
Brain connectivity
Brains of autistic individuals have been observed to have abnormal connectivity and the degree of these abnormalities directly correlates with the severity of autism. Following are some observed abnormal connectivity patterns in autistic individuals:[179][129]
- Decreased connectivity between different specialized regions of the brain (e.g. lower neuron density in corpus callosum) and relative over-connectivity within specialized regions of the brain by adulthood. Connectivity between different regions of the brain ('long-range' connectivity) is important for integration and global processing of information and comparing incoming sensory information with the existing model of the world within the brain. Connections within each specialized regions ('short-range' connections) are important for processing individual details and modifying the existing model of the world within the brain to more closely reflect incoming sensory information. In infancy, children at high risk for autism that were later diagnosed with autism were observed to have abnormally high long-range connectivity which then decreased through childhood to eventual long-range under-connectivity by adulthood.[179]
- Abnormal preferential processing of information by the left hemisphere of the brain vs. preferential processing of information by right hemisphere in neurotypical individuals. The left hemisphere is associated with processing information related to details whereas the right hemisphere is associated with processing information in a more global and integrated sense that is essential for pattern recognition. For example, visual information like face recognition is normally processed by the right hemisphere which tends to integrate all information from an incoming sensory signal, whereas an ASD brain preferentially processes visual information in the left hemisphere where information tends to be processed for local details of the face rather than the overall configuration of the face. This left lateralization negatively impacts both facial recognition and spatial skills.[179]
- Increased functional connectivity within the left hemisphere which directly correlates with severity of autism. This observation also supports preferential processing of details of individual components of sensory information over global processing of sensory information in an ASD brain.[179]
- Prominent abnormal connectivity in the frontal and occipital regions. In autistic individuals low connectivity in the frontal cortex was observed from infancy through adulthood. This is in contrast to long-range connectivity which is high in infancy and low in adulthood in ASD.[179] Abnormal neural organization is also observed in the Broca's area which is important for speech production.[129]
Neuropathology
Listed below are some characteristic findings in ASD brains on molecular and cellular levels regardless of the specific genetic variation or mutation contributing to autism in a particular individual:
- Limbic system with smaller neurons that are more densely packed together. Given that the limbic system is the main center of emotions and memory in the human brain, this observation may explain social impairment in ASD.[129]
- Fewer and smaller Purkinje neurons in the cerebellum. New research suggest a role of the cerebellum in emotional processing and language.[129]
- Increased number of astrocytes and microglia in the cerebral cortex. These cells provide metabolic and functional support to neurons and act as immune cells in the nervous system, respectively.[129]
- Increased brain size in early childhood causing macrocephaly in 15–20% of ASD individuals. The brain size however normalizes by mid-childhood. This variation in brain size in not uniform in the ASD brain with some parts like the frontal and temporal lobes being larger, some like the parietal and occipital lobes being normal sized, and some like cerebellar vermis, corpus callosum, and basal ganglia being smaller than neurotypical individuals.[129]
- Cell adhesion molecules that are essential to formation and maintenance of connections between neurons, neuroligins found on postsynaptic neurons that bind presynaptic cell adhesion molecules, and proteins that anchor cell adhesion molecules to neurons are all found to be mutated in ASD.[129]
Gut-immune-brain axis
46% to 84% of autistic individuals have GI-related problems like reflux, diarrhea, constipation, inflammatory bowel disease, and food allergies.[180] It has been observed that the makeup of gut bacteria in autistic people is different than that of neurotypical individuals which has raised the question of influence of gut bacteria on ASD development via inducing an inflammatory state.[181] Listed below are some research findings on the influence of gut bacteria and abnormal immune responses on brain development:[181]
- Some studies on rodents have shown gut bacteria influencing emotional functions and neurotransmitter balance in the brain, both of which are impacted in ASD.[129]
- The immune system is thought to be the intermediary that modulates the influence of gut bacteria on the brain. Some ASD individuals have a dysfunctional immune system with higher numbers of some types of immune cells, biochemical messengers and modulators, and autoimmune antibodies. Increased inflammatory biomarkers correlate with increased severity of ASD symptoms and there is some evidence to support a state of chronic brain inflammation in ASD.[181]
- More pronounced inflammatory responses to bacteria were found in ASD individuals with an abnormal gut microbiota. Additionally, immunoglobulin A antibodies that are central to gut immunity were also found in elevated levels in ASD populations. Some of these antibodies may attack proteins that support myelination of the brain, a process that is important for robust transmission of neural signal in many nerves.[181]
- Activation of the maternal immune system during pregnancy (by gut bacteria, bacterial toxins, an infection, or non-infectious causes) and gut bacteria in the mother that induce increased levels of Th17, a pro-inflammatory immune cell, have been associated with an increased risk of autism. Some maternal IgG antibodies that cross the placenta to provide passive immunity to the fetus can also attack the fetal brain.[181]
- It is proposed that inflammation within the brain promoted by inflammatory responses to harmful gut microbiome impacts brain development.[181]
- Pro-inflammatory cytokines IFN-γ, IFN-α, TNF-α, IL-6 and IL-17 have been shown to promote autistic behaviors in animal models. Giving anti-IL-6 and anti-IL-17 along with IL-6 and IL-17, respectively, have been shown to negate this effect in the same animal models.[181]
- Some gut proteins and microbial products can cross the blood–brain barrier and activate mast cells in the brain. Mast cells release pro-inflammatory factors and histamine which further increase blood–brain barrier permeability and help set up a cycle of chronic inflammation.[181]
Mirror neuron system
The mirror neuron system consists of a network of brain areas that have been associated with empathy processes in humans.[182] In humans, the mirror neuron system has been identified in the inferior frontal gyrus and the inferior parietal lobule and is thought to be activated during imitation or observation of behaviors.[183] The connection between mirror neuron dysfunction and autism is tentative, and it remains to be seen how mirror neurons may be related to many of the important characteristics of autism.[184][185]
Social brain interconnectivity
A number of discrete brain regions and networks among regions that are involved in dealing with other people have been discussed together under the rubric of the social brain. As of 2012, there is a consensus that autism spectrum is likely related to problems with interconnectivity among these regions and networks, rather than problems with any specific region or network.[186]
Temporal lobe
Functions of the temporal lobe are related to many of the deficits observed in individuals with ASDs, such as receptive language, social cognition, joint attention, action observation, and empathy. The temporal lobe also contains the superior temporal sulcus and the fusiform face area, which may mediate facial processing. It has been argued that dysfunction in the superior temporal sulcus underlies the social deficits that characterize autism. Compared to typically developing individuals, one study found that individuals with so-called high-functioning autism had reduced activity in the fusiform face area when viewing pictures of faces.[187]
Mitochondria
ASD could be linked to mitochondrial disease, a basic cellular abnormality with the potential to cause disturbances in a wide range of body systems.[188] A 2012 meta-analysis study, as well as other population studies show that approximately 5% of autistic children meet the criteria for classical mitochondrial dysfunction.[189] It is unclear why this mitochondrial disease occurs, considering that only 23% of children with both ASD and mitochondrial disease present with mitochondrial DNA abnormalities.[189]
Serotonin
Serotonin is a major neurotransmitter in the nervous system and contributes to formation of new neurons (neurogenesis), formation of new connections between neurons (synaptogenesis), remodeling of synapses, and survival and migration of neurons, processes that are necessary for a developing brain and some also necessary for learning in the adult brain. 45% of ASD individuals have been found to have increased blood serotonin levels.[129] It has been hypothesized that increased activity of serotonin in the developing brain may facilitate the onset of ASD, with an association found in six out of eight studies between the use of selective serotonin reuptake inhibitors (SSRIs) by the pregnant mother and the development of ASD in the child exposed to SSRI in the antenatal environment. The study could not definitively conclude SSRIs caused the increased risk for ASD due to the biases found in those studies, and the authors called for more definitive, better conducted studies.[190] Confounding by indication has since then been shown to be likely.[191] However, it is also hypothesized that SSRIs may help reduce symptoms of ASD and even positively affect brain development in some ASD patients.[129]
Diagnosis
Autism spectrum disorder is a clinical diagnosis that is typically made by a physician based off reported and directly observed behavior in the affected individual.[192] According to the updated diagnostic criteria in the DSM-5-TR, in order to receive a diagnosis of autism spectrum disorder, one must present with “persistent deficits in social communication and social interaction” and “restricted, repetitive patterns of behavior, interests, or activities.”[193] These behaviors must begin in early childhood and affect one's ability to perform everyday tasks. Furthermore, the symptoms must not be fully explainable by intellectual developmental disorder or global developmental delay.
There are several factors that make autism spectrum disorder difficult to diagnose. First off, there are no standardized imaging, molecular or genetic tests that can be used to diagnose ASD.[194] Additionally, there is a lot of variety in how ASD affects individuals. The behavioral manifestations of ASD depend on one's developmental stage, age of presentation, current support, and individual variability.[195][193] Lastly, there are multiple conditions that may present similarly to autism spectrum disorder, including intellectual disability, hearing impairment, a specific language impairment[196] such as Landau–Kleffner syndrome.[197] ADHD, anxiety disorder, and psychotic disorders.[198] Furthermore, the presence of autism can make it harder to diagnose coexisting psychiatric disorders such as depression.[199]
Ideally the diagnosis of ASD should be given by a team of clinicians (e.g. pediatricians, child psychiatrists, child neurologists) based on information provided from the affected individual, caregivers, other medical professionals and from direct observation.[200] Evaluation of a child or adult for autism spectrum disorder typically starts with a pediatrician or primary care physician taking a developmental history and performing a physical exam. If warranted, the physician may refer the individual to an ASD specialist who will observe and assess cognitive, communication, family, and other factors using standardized tools, and taking into account any associated medical conditions.[196] A pediatric neuropsychologist is often asked to assess behavior and cognitive skills, both to aid diagnosis and to help recommend educational interventions.[201] Further workup may be performed after someone is diagnosed with ASD. This may include a clinical genetics evaluation particularly when other symptoms already suggest a genetic cause.[202] Although up to 40% of ASD cases may be linked to genetic causes,[203] it is not currently recommended to perform complete genetic testing on every individual who is diagnosed with ASD. Consensus guidelines for genetic testing in patients with ASD in the US and UK are limited to high-resolution chromosome and fragile X testing.[202] Metabolic and neuroimaging tests are also not routinely performed for diagnosis of ASD.[202]
The age at which ASD is diagnosed varies. Sometimes ASD can be diagnosed as early as 14 months, however, a reliable diagnosis of ASD is usually made at the age of two years.[194] Diagnosis becomes increasingly stable over the first three years of life. For example, a one-year-old who meets diagnostic criteria for ASD is less likely than a three-year-old to continue to do so a few years later.[204] Additionally, age of diagnosis may depend on the severity of ASD, with more severe forms of ASD more likely to be diagnosed at an earlier age.[205] Issues with access to healthcare such as cost of appointments or delays in making appointments often lead to delays in the diagnosis of ASD.[206] In the UK the National Autism Plan for Children recommends at most 30 weeks from first concern to completed diagnosis and assessment, though few cases are handled that quickly in practice.[196] Lack of access to appropriate medical care, broadening diagnostic criteria and increased awareness surrounding ASD in recent years has resulted in an increased number of individuals receiving a diagnosis of ASD as adults. Diagnosis of ASD in adults poses unique challenges because it still relies on an accurate developmental history and because autistic adults sometimes learn coping strategies (known as 'camouflaging') which may make it more difficult to obtain a diagnosis.[207]
The presentation and diagnosis of autism spectrum disorder may vary based on sex and gender identity. Most studies that have investigated the impact of gender on presentation and diagnosis of autism spectrum disorder have not differentiated between the impact of sex versus gender.[208] There is some evidence that autistic women and girls tend to show less repetitive behavior and may engage in more camouflaging than autistic males.[209] Camouflaging may include making oneself perform normative facial expressions and eye contact.[210] Differences in behavioral presentation and gender-stereotypes may make it more challenging to diagnose autism spectrum disorder in a timely manner in females.[208][209] A notable percentage of autistic females may be misdiagnosed, diagnosed after a considerable delay, or not diagnosed at all.[209]
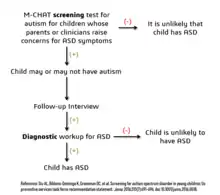
Considering the unique challenges in diagnosing ASD using behavioral and observational assessment, specific US practice parameters for its assessment were published by the American Academy of Neurology in the year 2000,[211] the American Academy of Child and Adolescent Psychiatry in 1999,[195] and a consensus panel with representation from various professional societies in 1999.[43] The practice parameters outlined by these societies include an initial screening of children by general practitioners (i.e., "Level 1 screening") and for children who fail the initial screening, a comprehensive diagnostic assessment by experienced clinicians (i.e. "Level 2 evaluation"). Furthermore, it has been suggested that assessments of children with suspected ASD be evaluated within a developmental framework, include multiple informants (e.g., parents and teachers) from diverse contexts (e.g., home and school), and employ a multidisciplinary team of professionals (e.g., clinical psychologists, neuropsychologists, and psychiatrists).[212]
As of 2019, psychologists wait until a child showed initial evidence of ASD tendencies, then administer various psychological assessment tools to assess for ASD.[212] Among these measurements, the Autism Diagnostic Interview-Revised (ADI-R) and the Autism Diagnostic Observation Schedule (ADOS) are considered the "gold standards" for assessing autistic children.[213][214] The ADI-R is a semi-structured parent interview that probes for symptoms of autism by evaluating a child's current behavior and developmental history. The ADOS is a semi-structured interactive evaluation of ASD symptoms that is used to measure social and communication abilities by eliciting several opportunities for spontaneous behaviors (e.g., eye contact) in standardized context. Various other questionnaires (e.g., The Childhood Autism Rating Scale, Autism Treatment Evaluation Checklist) and tests of cognitive functioning (e.g., The Peabody Picture Vocabulary Test) are typically included in an ASD assessment battery. The diagnostic interview for social and communication disorders (DISCO) may also be used.[215]
Screening
About half of parents of children with ASD notice their child's atypical behaviors by age 18 months, and about four-fifths notice by age 24 months.[204] If a child does not meet any of the following milestones, it "is an absolute indication to proceed with further evaluations. Delay in referral for such testing may delay early diagnosis and treatment and affect the [child's] long-term outcome."[43]
- No response to name (or gazing with direct eye contact) by 6 months.[216]
- No babbling by 12 months.
- No gesturing (pointing, waving, etc.) by 12 months.
- No single words by 16 months.
- No two-word (spontaneous, not just echolalic) phrases by 24 months.
- Loss of any language or social skills, at any age.
The Japanese practice is to screen all children for ASD at 18 and 24 months, using autism-specific formal screening tests. In contrast, in the UK, children whose families or doctors recognize possible signs of autism are screened. It is not known which approach is more effective.[110] The UK National Screening Committee does not recommend universal ASD screening in young children. Their main concerns includes higher chances of misdiagnosis at younger ages and lack of evidence of effectiveness of early interventions.[217] There is no consensus between professional and expert bodies in the US on screening for autism in children younger than 3 years.[219]
Screening tools include the Modified Checklist for Autism in Toddlers (M-CHAT), the Early Screening of Autistic Traits Questionnaire, and the First Year Inventory; initial data on M-CHAT and its predecessor, the Checklist for Autism in Toddlers (CHAT), on children aged 18–30 months suggests that it is best used in a clinical setting and that it has low sensitivity (many false-negatives) but good specificity (few false-positives).[204] It may be more accurate to precede these tests with a broadband screener that does not distinguish ASD from other developmental disorders.[220] Screening tools designed for one culture's norms for behaviors like eye contact may be inappropriate for a different culture.[221] Although genetic screening for autism is generally still impractical, it can be considered in some cases, such as children with neurological symptoms and dysmorphic features.[222]
Misdiagnosis
There is a significant level of misdiagnosis of autism in neurodevelopmentally typical children; 18–37% of children diagnosed with ASD eventually lose their diagnosis. This high rate of lost diagnosis cannot be accounted for by successful ASD treatment alone. The most common reason parents reported as the cause of lost ASD diagnosis was new information about the child (73.5%), such as a replacement diagnosis. Other reasons included a diagnosis given so the child could receive ASD treatment (24.2%), ASD treatment success or maturation (21%), and parents disagreeing with the initial diagnosis (1.9%).[218]
Many of the children who were later found not to meet ASD diagnosis criteria then received diagnosis for another developmental disorder. Most common was ADHD, but other diagnoses included sensory disorders, anxiety, personality disorder, or learning disability.[218] Neurodevelopment and psychiatric disorders that are commonly misdiagnosed as ASD include specific language impairment, social communication disorder, anxiety disorder, reactive attachment disorder, cognitive impairment, visual impairment, hearing loss and normal behavioral variation.[223] Some behavioral variations that resemble autistic traits are repetitive behaviors, sensitivity to change in daily routines, focused interests, and toe-walking. These are considered normal behavioral variations when they do not cause impaired function. Boys are more likely to exhibit repetitive behaviors especially when excited, tired, bored, or stressed. Some ways of distinguishing typical behavioral variations from autistic behaviors are the ability of the child to suppress these behaviors and the absence of these behaviors during sleep.[200]
Comorbidity
ASDs tend to be highly comorbid with other disorders.[110] Comorbidity may increase with age and may worsen the course of youth with ASDs and make intervention and treatment more difficult. Distinguishing between ASDs and other diagnoses can be challenging because the traits of ASDs often overlap with symptoms of other disorders, and the characteristics of ASDs make traditional diagnostic procedures difficult.[224][225]
- The most common medical condition occurring in individuals with ASDs is seizure disorder or epilepsy, which occurs in 11–39% of autistic individuals.[226] The risk varies with age, cognitive level, and type of language disorder.[227]
- Tuberous sclerosis, an autosomal dominant genetic condition in which non-malignant tumors grow in the brain and on other vital organs, is present in 1–4% of individuals with ASDs.[228]
- Intellectual disabilities are some of the most common comorbid disorders with ASDs. Recent estimates suggest that 40–69% of autistic individuals have some degree of an intellectual disability,[64] more likely to be severe for females. A number of genetic syndromes causing intellectual disability may also be comorbid with ASD, including fragile X, Down, Prader-Willi, Angelman, Williams syndrome[229] and SYNGAP1-related intellectual disability.[230][231]
- Learning disabilities are also highly comorbid in individuals with an ASD. Approximately 25–75% of individuals with an ASD also have some degree of a learning disability.[232]
- Various anxiety disorders tend to co-occur with ASDs, with overall comorbidity rates of 7–84%.[64] They are common among children with ASD; there are no firm data, but studies have reported prevalences ranging from 11% to 84%. Many anxiety disorders have symptoms that are better explained by ASD itself, or are hard to distinguish from ASD's symptoms.[233]
- Rates of comorbid depression in individuals with an ASD range from 4–58%.[234]
- The relationship between ASD and schizophrenia remains a controversial subject under continued investigation, and recent meta-analyses have examined genetic, environmental, infectious, and immune risk factors that may be shared between the two conditions.[235][236][237] Oxidative stress, DNA damage and DNA repair have been postulated to play a role in the aetiopathology of both ASD and schizophrenia.[238]
- Deficits in ASD are often linked to behavior problems, such as difficulties following directions, being cooperative, and doing things on other people's terms.[239] Symptoms similar to those of attention deficit hyperactivity disorder (ADHD) can be part of an ASD diagnosis.[240]
- Sensory processing disorder is also comorbid with ASD, with comorbidity rates of 42–88%.[241]
- Starting in adolescence, some people with Asperger syndrome (26% in one sample)[242] fall under the criteria for the similar condition schizoid personality disorder, which is characterized by a lack of interest in social relationships, a tendency towards a solitary or sheltered lifestyle, secretiveness, emotional coldness, detachment and apathy.[242][243][244] Asperger syndrome was traditionally called "schizoid disorder of childhood."
- Genetic disorders - about 10–15% of autism cases have an identifiable Mendelian (single-gene) condition, chromosome abnormality, or other genetic syndromes.[245]
- Several metabolic defects, such as phenylketonuria, are associated with autistic symptoms.[246]
- Sleep problems affect about two-thirds of individuals with ASD at some point in childhood. These most commonly include symptoms of insomnia such as difficulty in falling asleep, frequent nocturnal awakenings, and early morning awakenings. Sleep problems are associated with difficult behaviors and family stress, and are often a focus of clinical attention over and above the primary ASD diagnosis.[247]
Management
There is no treatment as such for autism,[248] and many sources advise that this is not an appropriate goal,[249][250] although treatment of co-occurring conditions remains an important goal.[251] There is no known cure for autism, nor can any known treatments significantly reduce brain mutations caused by autism, although those who require little-to-no support are more likely to experience a lessening of symptoms over time.[252][253][254] Several interventions can help children with autism,[255] and no single treatment is best, with treatment typically tailored to the child's needs.[256] Studies of interventions have methodological problems that prevent definitive conclusions about efficacy;[257] however, the development of evidence-based interventions has advanced.[258]
The main goals of treatment are to lessen associated deficits and family distress, and to increase quality of life and functional independence. In general, higher IQs are correlated with greater responsiveness to treatment and improved treatment outcomes.[259][260] Behavioral, psychological, education, and/or skill-building interventions may be used to assist autistic people to learn life skills necessary for living independently,[261] as well as other social, communication, and language skills. Therapy also aims to reduce challenging behaviors and build upon strengths.[262]
Intensive, sustained special education programs and behavior therapy early in life can help children acquire self-care, communication, and job skills.[256] Although evidence-based interventions for autistic children vary in their methods, many adopt a psychoeducational approach to enhancing cognitive, communication, and social skills while minimizing problem behaviors. While medications have not been found to help with core symptoms, they may be used for associated symptoms, such as irritability, inattention, or repetitive behavior patterns.[263]
Non-pharmacological interventions
Intensive, sustained special education or remedial education programs and behavior therapy early in life can help children acquire self-care, social, and job skills. Available approaches include applied behavior analysis, developmental models, structured teaching, speech and language therapy, social skills therapy, and occupational therapy.[264] Among these approaches, interventions either treat autistic features comprehensively, or focus treatment on a specific area of deficit.[260] Generally, when educating those with autism, specific tactics may be used to effectively relay information to these individuals. Using as much social interaction as possible is key in targeting the inhibition autistic individuals experience concerning person-to-person contact. Additionally, research has shown that employing semantic groupings, which involves assigning words to typical conceptual categories, can be beneficial in fostering learning.[265]
There has been increasing attention to the development of evidence-based interventions for autistic young children. Two theoretical frameworks outlined for early childhood intervention include applied behavioral analysis (ABA) and the developmental social-pragmatic model (DSP).[260] Although ABA therapy has a strong evidence base, particularly in regard to early intensive home-based therapy, ABA's effectiveness may be limited by diagnostic severity and IQ of the person affected by ASD.[266] The Journal of Clinical Child and Adolescent Psychology has deemed two early childhood interventions as "well-established":[267] individual comprehensive ABA, and focused teacher-implemented ABA combined with DSP.[260]
Another evidence-based intervention that has demonstrated efficacy is a parent training model, which teaches parents how to implement various ABA and DSP techniques themselves.[260] Various DSP programs have been developed to explicitly deliver intervention systems through at-home parent implementation.
In October 2015, the American Academy of Pediatrics (AAP) proposed new evidence-based recommendations for early interventions in ASD for children under 3.[268] These recommendations emphasize early involvement with both developmental and behavioral methods, support by and for parents and caregivers, and a focus on both the core and associated symptoms of ASD.[268] However, a Cochrane review found no evidence that early intensive behavioral intervention (EIBI) is effective in reducing behavioral problems associated with autism in most autistic children but did help improve IQ and language skills. The Cochrane review did acknowledge that this may be due to the low quality of studies currently available on EIBI and therefore providers should recommend EIBI based on their clinical judgement and the family's preferences. No adverse effects of EIBI treatment were found.[269] Studies on pet therapy have shown positive effects.[270]
Generally speaking, treatment of ASD focuses on behavioral and educational interventions to target its two core symptoms: social communication deficits and restricted, repetitive behaviors.[271] If symptoms continue after behavioral strategies have been implemented, some medications can be recommended to target specific symptoms or co-existing problems such as restricted and repetitive behaviors (RRBs), anxiety, depression, hyperactivity/inattention and sleep disturbance.[271] Melatonin for example can be used for sleep problems.[272]
While there are a number of parent-mediated behavioral therapies to target social communication deficits in children with autism, there is uncertainty regarding the efficacy of interventions to treat RRBs.[273]
Education

Educational interventions often used include applied behavior analysis (ABA), developmental models, structured teaching, speech and language therapy and social skills therapy.[256] Among these approaches, interventions either treat autistic features comprehensively, or focalize treatment on a specific area of deficit.[258] The quality of research for early intensive behavioral intervention (EIBI)—a treatment procedure incorporating over thirty hours per week of the structured type of ABA that is carried out with very young children—is currently low, and more vigorous research designs with larger sample sizes are needed.[269] Two theoretical frameworks outlined for early childhood intervention include structured and naturalistic ABA interventions, and developmental social pragmatic models (DSP).[258] One interventional strategy utilizes a parent training model, which teaches parents how to implement various ABA and DSP techniques, allowing for parents to disseminate interventions themselves.[258] Various DSP programs have been developed to explicitly deliver intervention systems through at-home parent implementation. Despite the recent development of parent training models, these interventions have demonstrated effectiveness in numerous studies, being evaluated as a probable efficacious mode of treatment.[258] Early, intensive ABA therapy has demonstrated effectiveness in enhancing communication and adaptive functioning in preschool children;[256] it is also well-established for improving the intellectual performance of that age group.[256]
Similarly, a teacher-implemented intervention that utilizes a more naturalistic form of ABA combined with a developmental social pragmatic approach has been found to be beneficial in improving social-communication skills in young children, although there is less evidence in its treatment of global symptoms.[258] Neuropsychological reports are often poorly communicated to educators, resulting in a gap between what a report recommends and what education is provided.[201] The appropriateness of including children with varying severity of autism spectrum disorders in the general education population is a subject of current debate among educators and researchers.[275]
Pharmacological interventions
Medications may be used to treat ASD symptoms that interfere with integrating a child into home or school when behavioral treatment fails.[276] They may also be used for associated health problems, such as ADHD or anxiety.[276] However, their routine prescription for the core features of ASD is not recommended.[277] More than half of US children diagnosed with ASD are prescribed psychoactive drugs or anticonvulsants, with the most common drug classes being antidepressants, stimulants, and antipsychotics.[278][279] The atypical antipsychotic drugs risperidone and aripiprazole are FDA-approved for treating associated aggressive and self-injurious behaviors.[263][280] However, their side effects must be weighed against their potential benefits, and autistic people may respond atypically.[263] Side effects may include weight gain, tiredness, drooling, and aggression.[263] There is some emerging data that show positive effects of aripiprazole and risperidone on restricted and repetitive behaviors (i.e., stimming; e.g., flapping, twisting, complex whole-body movements),[277] but due to the small sample size and different focus of these studies and the concerns about its side effects, antipsychotics are not recommended as primary treatment of RRBs.[281] SSRI antidepressants, such as fluoxetine and fluvoxamine, have been shown to be effective in reducing repetitive and ritualistic behaviors, while the stimulant medication methylphenidate is beneficial for some children with co-morbid inattentiveness or hyperactivity.[256] There is scant reliable research about the effectiveness or safety of drug treatments for adolescents and adults with ASD. No known medication relieves autism's core symptoms of social and communication impairments.[263]
Alternative medicine
A multitude of researched alternative therapies have also been implemented. Many have resulted in harm to autistic people.[264] A 2020 systematic review on adults with autism has provided emerging evidence for decreasing stress, anxiety, ruminating thoughts, anger, and aggression through mindfulness-based interventions for improving mental health.[282]
Although popularly used as an alternative treatment for autistic people, as of 2018 there is no good evidence to recommend a gluten- and casein-free diet as a standard treatment.[283][284][285] A 2018 review concluded that it may be a therapeutic option for specific groups of children with autism, such as those with known food intolerances or allergies, or with food intolerance markers. The authors analyzed the prospective trials conducted to date that studied the efficacy of the gluten- and casein-free diet in children with ASD (4 in total). All of them compared gluten- and casein-free diet versus normal diet with a control group (2 double-blind randomized controlled trials, 1 double-blind crossover trial, 1 single-blind trial). In two of the studies, whose duration was 12 and 24 months, a significant improvement in ASD symptoms (efficacy rate 50%) was identified. In the other two studies, whose duration was 3 months, no significant effect was observed.[283] The authors concluded that a longer duration of the diet may be necessary to achieve the improvement of the ASD symptoms.[283] Other problems documented in the trials carried out include transgressions of the diet, small sample size, the heterogeneity of the participants and the possibility of a placebo effect.[285][286][287] In the subset of people who have gluten sensitivity there is limited evidence that suggests that a gluten-free diet may improve some autistic behaviors.[288][289][290]
The preference that autistic children have for unconventional foods can lead to reduction in bone cortical thickness with this risk being greater in those on casein-free diets, as a consequence of the low intake of calcium and vitamin D; however, suboptimal bone development in ASD has also been associated with lack of exercise and gastrointestinal disorders.[291] In 2005, botched chelation therapy killed a five-year-old child with autism.[292][293] Chelation is not recommended for autistic people since the associated risks outweigh any potential benefits.[294] Another alternative medicine practice with no evidence is CEASE therapy, a pseudoscientific mixture of homeopathy, supplements, and 'vaccine detoxing'.[295]
Results of a systematic review on interventions to address health outcomes among autistic adults found emerging evidence to support mindfulness-based interventions for improving mental health. This includes decreasing stress, anxiety, ruminating thoughts, anger, and aggression.[296] An updated Cochrane review (2022) found evidence that music therapy likely improves social interactions, verbal communication, and non-verbal communication skills.[297] There has been early research looking at hyperbaric treatments in children with autism.[298] Studies on pet therapy have shown positive effects.[299]
Prevention
While infection with rubella during pregnancy causes fewer than 1% of cases of autism,[300] vaccination against rubella can prevent many of those cases.[301]
Outcomes
There is no known cure for autism.[256][110] The degree of symptoms can decrease, occasionally to the extent that people lose their diagnosis of ASD;[302] this occurs sometimes after intensive treatment and sometimes not. It is not known how often this outcome happens,[303] with reported rates in unselected samples ranging from 3% to 25%.[302] Although core difficulties tend to persist, symptoms often become less severe with age.[51] Acquiring language before age six, having an IQ above 50, and having a marketable skill all predict better outcomes; independent living is unlikely with severe autism.[304]
Many autistic people face significant obstacles in transitioning to adulthood.[305] Compared to the general population, autistic people are more likely to be unemployed and to have never had a job. About half of people in their 20s with autism are not employed.[306] Some autistic adults are unable to live independently.[307]
Academic performance
The number of students identified and served as eligible for autism services in the United States has increased from 5,413 children in 1991–1992 to 370,011 children in the 2010–2011 academic school year.[308] The United States Department of Health and Human Services reported approximately 1 in 68 children are diagnosed with ASD at age 8 although onset is typically between ages 2 and 4.[308]
The increasing number of students diagnosed with ASD in the schools presents significant challenges to teachers, school psychologists, and other school professionals.[308] These challenges include developing a consistent practice that best support the social and cognitive development of the increasing number of autistic students.[308] Although there is considerable research addressing assessment, identification, and support services for autistic children, there is a need for further research focused on these topics within the school context.[308] Further research on appropriate support services for students with ASD will provide school psychologists and other education professionals with specific directions for advocacy and service delivery that aim to enhance school outcomes for students with ASD.[308]
Attempts to identify and use best intervention practices for students with autism also pose a challenge due to over dependence on popular or well-known interventions and curricula.[308] Some evidence suggests that although these interventions work for some students, there remains a lack of specificity for which type of student, under what environmental conditions (one-on-one, specialized instruction or general education) and for which targeted deficits they work best.[308] More research is needed to identify what assessment methods are most effective for identifying the level of educational needs for students with ASD. Additionally, children living in higher resources settings in the United States tend to experience earlier ASD interventions than children in lower resource settings (e.g. rural areas).[309]
A difficulty for academic performance in students with ASD is the tendency to generalize learning.[76] Learning is different for each student, which is the same for students with ASD. To assist in learning, accommodations are commonly put into place for students with differing abilities. The existing schema of these students works in different ways and can be adjusted to best support the educational development for each student.[310]
The cost of educating a student with ASD in the US is about $8,600 a year more than the cost of educating an average student, which is about $12,000.[311]
Though much of the focus on early childhood intervention for ASD has centered on high-income countries like the United States, some of the most significant unmet needs for autistic individuals are in low- and middle-income countries.[309] In these contexts, research has been more limited but there is evidence to suggest that some comprehensive care plans can be successfully delivered by non-specialists in schools and in the community.[309]
Employment
In the United States, about half of people in their 20s with autism are unemployed, and one third of those with graduate degrees may be unemployed.[312] While employers state hiring concerns about productivity and supervision, experienced employers of autistics give positive reports of above average memory and detail orientation as well as a high regard for rules and procedure in autistic employees.[312] The majority of the economic burden of autism is caused by lost productivity in the job market.[313] From the perspective of the social model of disability, social model of disability, much of this unemployment is caused by the lack of understanding from employers and coworkers.[314][315] Adding content related to autism in existing diversity training can clarify misconceptions, support employees, and help provide new opportunities for autistic people.[316] As of 2021, the potential for new autism employment initiatives by major employers in the United States continue to grow. The most high-profile autism initiative in the United States, "Autism at Work" grew to 20 of the largest companies in the United States.[317] However, special hiring programs remain largely limited to entry-level technology positions, such as software testing, and exclude those who have talents outside of technology. An alternative approach is systemic neurodiversity inclusion. Developing organizational systems with enough flexibility and fairness to include autistic employees improves the work experience of all employees.[318][319]
Epidemiology
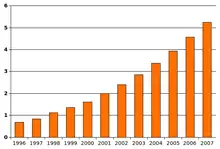
The World Health Organization (WHO) estimates that about 1 in 100 children have autism.[320] The number of people diagnosed has increased considerably since the 1990s, which may be partly due to increased recognition of the condition.[321]
While rates of ASD are consistent across cultures, they vary greatly by gender, with boys diagnosed far more frequently than girls: 1 in 70 boys, but only 1 in 315 girls at eight years of age.[322] Girls, however, are more likely to have associated cognitive impairment, suggesting that less severe forms of ASD are likely being missed in girls and women.[323] Prevalence differences may be a result of gender differences in expression of clinical symptoms, with women and girls with autism showing less atypical behaviors and, therefore, less likely to receive an ASD diagnosis.[324]
Using DSM-5 criteria, 92% of the children diagnosed per DSM-IV with one of the disorders which is now considered part of ASD will still meet the diagnostic criteria of ASD. However, if both ASD and the social (pragmatic) communication disorder categories of DSM-5 are combined, the prevalence of autism is mostly unchanged from the prevalence per the DSM-IV criteria. The best estimate for prevalence of ASD is 0.7% or 1 child in 143 children.[325] Relatively mild forms of autism, such as Aspergers as well as other developmental disorders, are included in the DSM-5 diagnostic criteria.[326] ASD rates were constant between 2014 and 2016 but twice the rate compared to the time period between 2011 and 2014 (1.25 vs 2.47%). A Canadian meta-analysis from 2019 confirmed these effects as the profiles of people diagnosed with autism became less and less different from the profiles of the general population.[327] In the US, the rates for diagnosed ASD have been steadily increasing since 2000 when records began being kept.[328] While it remains unclear whether this trend represents a true rise in incidence, it likely reflects changes in ASD diagnostic criteria, improved detection, and increased public awareness of autism.[329] In 2012, the NHS estimated that the overall prevalence of autism among adults aged 18 years and over in the UK was 1.1%.[330] A 2016 survey in the United States reported a rate of 25 per 1,000 children for ASD.[331] It is important to note that rates of autism are poorly understood in many low- and middle-income countries, which affects the accuracy of global ASD prevalence estimates,[332] but it is thought that most autistic individuals live in low- and middle-income countries.[309]
In the UK, from 1998 to 2018, the autism diagnoses increased by 787%.[321] This increase is largely attributable to changes in diagnostic practices, referral patterns, availability of services, age at diagnosis, and public awareness[333][334][335] (particularly among women),[321] though unidentified environmental risk factors cannot be ruled out.[336] The available evidence does not rule out the possibility that autism's true prevalence has increased;[333] a real increase would suggest directing more attention and funding toward psychosocial factors and changing environmental factors instead of continuing to focus on genetics.[337] It has been established that vaccination is not a risk factor for autism and is not a cause of any increase in autism prevalence rates, if any change in the rate of autism exists at all.[156]
Males have higher likelihood of being diagnosed with ASD than females. The sex ratio averages 4.3:1 and is greatly modified by cognitive impairment: it may be close to 2:1 with intellectual disability and more than 5.5:1 without.[142] Several theories about the higher prevalence in males have been investigated, but the cause of the difference is unconfirmed;[338] one theory is that females are underdiagnosed.[339]
The risk of developing autism is greater with older fathers than with older mothers; two potential explanations are the known increase in mutation burden in older sperm, and the hypothesis that men marry later if they carry genetic liability and show some signs of autism.[21] Most professionals believe that race, ethnicity, and socioeconomic background do not affect the occurrence of autism.[340]
United States
In the United States it is estimated to affect more than 2% of children (about 1.5 million) as of 2016.[341] According to the latest CDC prevalence reports, 1 in 44 children (2.3%) in the United States had a diagnosis of ASD in 2018.[342] Prevalence is estimated at 6 per 1,000 for ASDs as a whole.[142]
History
A few examples of autistic symptoms and treatments were described long before autism was named. The Table Talk of Martin Luther, compiled by his notetaker, Mathesius, contains the story of a 12-year-old boy who may have been severely autistic.[344] The earliest well-documented case of autism is that of Hugh Blair of Borgue, as detailed in a 1747 court case in which his brother successfully petitioned to annul Blair's marriage to gain Blair's inheritance.[345]
The Wild Boy of Aveyron, a feral child found in 1798, showed several signs of autism. He was non-verbal during his teenage years, and his case was widely popular among society for its time. Such cases brought awareness to autism, and more research was conducted on the natural dimensions of human behavior. The medical student Jean Itard treated him with a behavioral program designed to help him form social attachments and to induce speech via imitation.[343]
The New Latin word autismus (English translation autism) was coined by the Swiss psychiatrist Eugen Bleuler in 1910 as he was defining symptoms of schizophrenia. He derived it from the Greek word: αὐτός, romanized: autós, lit. 'self' and used it to mean morbid self-admiration, referring to "autistic withdrawal of the patient to his fantasies, against which any influence from outside becomes an intolerable disturbance".[346] A Soviet child psychiatrist, Grunya Sukhareva, described a similar syndrome in Russian in 1925, and in German in 1926.[347]
Clinical development and diagnoses

Autism spectrum disorder, as it is known today, can be traced back to the late 1930s, when two separate psychiatrists – Leo Kanner of Johns Hopkins Hospital and Hans Asperger of the Vienna University Hospital – used the word autism to describe the patients they were studying in their own clinical research and practice. The word autism first took its modern sense in German, when Asperger adopted Bleuler's terminology autistic psychopaths in a 1938 lecture in German about child psychology.[348] Asperger was investigating an ASD which was later known as Asperger syndrome, although it did not become widely recognized as a separate diagnosis until 1981; it has since been eliminated from the lexicon.[343] In English, Kanner first used autism in its modern sense when he introduced the label early infantile autism in a 1943 report of 11 children with striking behavioral similarities; his publication was named Autistic Disturbances of Affective Contact.[349] Almost all the characteristics described in Kanner's first paper on the subject, notably "autistic aloneness" and "insistence on sameness", are still regarded as typical of autistic spectrum disorder.[105] It is not known whether Kanner derived the term independently of Hans Asperger.[350]
Kanner's reuse of autism led to decades of confused terminology like infantile schizophrenia, and child psychiatry's focus on maternal deprivation led to misconceptions of autism as an infant's response to "refrigerator mothers". Starting in the late 1960s, autism was established as a separate syndrome from schizophrenia.[351] Leo Kanner was the first person to describe autism as a neurodevelopmental disorder in 1943 by calling it infantile autism and therefore rejected the refrigerator mother theory.[352]
The discussion of autism prior to the twentieth century brought about much controversy. Without researchers being able to meet a consensus on the varying forms of condition, there was a lack of research being conducted on the disorder. Discussing the syndrome and its complexity frustrated researchers at the time. Controversies have surrounded various claims regarding the etiology of autism. In the 1950s, the refrigerator mother theory emerged as an explanation for autism despite no scientific evidence behind it. The hypothesis was based on the idea that autistic behaviors stem from the emotional "frigidity," lack of warmth, and cold, distant, rejecting demeanor of a child's mother.[353] Parents of children with an ASD experienced blame, guilt and self-doubt, especially as the theory was embraced by the medical establishment and went largely unchallenged into the mid-1960s.[354] The "refrigerator mother" theory has since been refuted in the scientific literature, including a 2015 systematic review which showed absolutely no association between caregiver interaction and language outcomes in ASD patients.[355] Another controversial claim suggested that watching extensive amounts of television may cause autism. This hypothesis was largely based on research suggesting that the increasing rates of autism in the 1970s and 1980s were linked to the growth of cable television at the time.[154]
Terminology and distinction from schizophrenia
As late as the mid-1970s there was little evidence of a genetic role in autism, however by 2007 it was recognised as one of the most heritable psychiatric conditions.[356] Although the rise of parent organizations and the destigmatization of childhood ASD have affected how ASD is viewed,[343] parents continue to feel social stigma in situations where their child's autistic behavior is perceived negatively,[357] and many primary care physicians and medical specialists express beliefs consistent with outdated autism research.[358]
It took until 1980 for the DSM-III to differentiate autism from childhood schizophrenia. In 1987, the DSM-III-R provided a checklist for diagnosing autism. In May 2013, the DSM-5 was released, updating the classification for pervasive developmental disorders. The grouping of disorders, including PDD-NOS, autism, Asperger syndrome, Rett syndrome, and CDD, has been removed and replaced with the general term of Autism Spectrum Disorders. The two categories that exist are impaired social communication and/or interaction, and restricted and/or repetitive behaviors.[359]
The Internet has helped autistic individuals bypass nonverbal cues and emotional sharing that they find difficult to deal with, and has given them a way to form online communities and work remotely.[360] Societal and cultural aspects of autism have developed: some in the community seek a cure, while others believe that autism is simply another way of being.[361][362]
Society and culture

An autistic culture has emerged, accompanied by the autistic rights and neurodiversity movements who argue autism should be accepted as a difference to be accommodated instead of cured,[363][364][365][366][361] although a minority of autistic individuals do continue seeking a cure.[367] Worldwide, events related to autism include World Autism Awareness Day, Autism Sunday, Autistic Pride Day, Autreat, and others.[368][369][370][371] Social-science scholars study those with autism in hopes to learn more about "autism as a culture, transcultural comparisons ... and research on social movements."[372] Many autistic individuals have been successful in their fields.[373]
Neurodiversity movement

Some autistic people, as well as a number of researchers, have advocated a shift in attitudes toward the view that autism spectrum disorder is a difference, rather than a disease that must be treated or cured.[374][375][376] Critics have bemoaned the entrenchment of some of these groups' opinions.[377][378][379][380]
The neurodiversity movement and the autism rights movement are social movements within the context of disability rights, emphasizing the concept of neurodiversity, which describes the autism spectrum as a result of natural variations in the human brain rather than a disorder to be cured.[365] The autism rights movement advocates for including greater acceptance of autistic behaviors; therapies that focus on coping skills rather than imitating the behaviors of those without autism;[381] and the recognition of the autistic community as a minority group.[381][382] Autism rights or neurodiversity advocates believe that the autism spectrum is genetic and should be accepted as a natural expression of the human genome.[365] However, these movements are not without criticism; for example, a common argument made against neurodiversity activists is that the majority of them are high-functioning, have Asperger syndrome, or are self-diagnosed, and do not represent the views of low-functioning autistic people.[382][383][384]
The concept of neurodiversity is contentious within various autism advocacy and research groups and has led to infighting.[378][379]
Caregivers
Families who care for an autistic child face added stress from a number of different causes.[385] Parents may struggle to understand the diagnosis and to find appropriate care options. Parents often take a negative view of the diagnosis, and may struggle emotionally.[386] More than half of parents over the age of 50 are still living with their child, as about 85% of autistic people have difficulties living independently.[387] Some studies also find decreased earning among parents who care for autistic children.[388][389]
Broader autism phenotype
The broader autism phenotype (BAP) describes individuals who may not have ASD but do have autistic traits, such as avoiding eye contact and stimming.[390]
See also
- Autism spectrum disorders in the media
- Extraordinary Attorney Woo
- List of films about autism
- Social narrative
References
- Bonati M, Cartabia M, Clavenna A (January 2022). "Still too much delay in recognition of autism spectrum disorder". Epidemiology and Psychiatric Sciences. Cambridge University Press. 31 (e1): e1. doi:10.1017/S2045796021000822. LCCN 2011243374. OCLC 727338545. PMC 8786613. PMID 35012703. S2CID 245851335.
- Wing L, Gould J, Gillberg C (1 March 2011). "Autism spectrum disorders in the DSM-V: better or worse than the DSM-IV?". Research in Developmental Disabilities. Elsevier. 32 (2): 768–773. doi:10.1016/j.ridd.2010.11.003. eISSN 1873-3379. ISSN 0891-4222. PMID 21208775.
- Rosen NE, Lord C, Volkmar FR (December 2021). "The Diagnosis of Autism: From Kanner to DSM-III to DSM-5 and Beyond". Journal of Autism and Developmental Disorders. 51 (12): 4253–4270. doi:10.1007/s10803-021-04904-1. PMC 8531066. PMID 33624215.
- DSM-5-TR.
- Reed GM, First MB, Kogan CS, Hyman SE, Gureje O, Gaebel W, et al. (February 2019). "Innovations and changes in the ICD-11 classification of mental, behavioural and neurodevelopmental disorders". World Psychiatry. 18 (1): 3–19. doi:10.1002/wps.20611. PMC 6313247. PMID 30600616.
- Pellicano E, den Houting J (April 2022). "Annual Research Review: Shifting from 'normal science' to neurodiversity in autism science". Journal of Child Psychology and Psychiatry, and Allied Disciplines. 63 (4): 381–396. doi:10.1111/jcpp.13534. eISSN 1469-7610. ISSN 0021-9630. OCLC 01307942. PMC 9298391. PMID 34730840. S2CID 241118562.
- Bailin A (6 June 2019). "Clearing Up Some Misconceptions about Neurodiversity". Scientific American Blog Network. Nature America, Inc. Archived from the original on 29 June 2019. Retrieved 17 March 2022.
- Robison JE (2020). "My Time with Autism Speaks". In Kapp SK (ed.). Autistic Community and the Neurodiversity Movement. Autistic Community and the Neurodiversity Movement: Stories from the Frontline. Singapore: Springer. pp. 221–232. doi:10.1007/978-981-13-8437-0_16. ISBN 978-981-13-8437-0. S2CID 210496353. Retrieved 23 April 2022.
- Opar, Alisa (24 April 2019). "In search of truce in the autism wars". Spectrum. Simons Foundation. Archived from the original on 3 May 2019. Retrieved 9 July 2022.
- Opar, Alisa (6 May 2019). "A medical condition or just a difference? The question roils autism community". The Washington Post. spectrumnews.org. ISSN 0190-8286. Archived from the original on 7 May 2019. Retrieved 23 April 2022.
- "Autism: A New Introduction to Psychological Theory and Current Debate".
- Davis, Rachael; Crompton, Catherine J. (2021). "What do New Findings About Social Interaction in Autistic Adults Mean for Neurodevelopmental Research?". Perspectives on Psychological Science. 16 (3): 649–653. doi:10.1177/1745691620958010. PMC 8114326. PMID 33560175.
- Mitchell, Peter; Sheppard, Elizabeth; Cassidy, Sarah (2021). "Autism and the double empathy problem: Implications for development and mental health". British Journal of Developmental Psychology. 39 (1): 1–18. doi:10.1111/bjdp.12350. PMID 33393101. S2CID 230489027.
- White, Rebekah; Remington, Anna (2018). "Object personification in autism: This paper will be very sad if you don't read it". Autism. 23 (4): 1042–1045. doi:10.1177/1362361318793408. ISSN 1362-3613. PMID 30101594. S2CID 51969215.
- Hamilton AF (2009). "Goals, intentions and mental states: challenges for theories of autism". J Child Psychol Psychiatry. 50 (8): 881–92. CiteSeerX 10.1.1.621.6275. doi:10.1111/j.1469-7610.2009.02098.x. PMID 19508497.
- Mandy W, Lai MC (March 2016). "Annual Research Review: The role of the environment in the developmental psychopathology of autism spectrum condition". Journal of Child Psychology and Psychiatry, and Allied Disciplines. 57 (3): 271–292. doi:10.1111/jcpp.12501. eISSN 1469-7610. ISSN 0021-9630. OCLC 01307942. PMID 26782158.
- Losh M, Adolphs R, Piven J (2011). "The Broad Autism Phenotype". Autism Spectrum Disorders. Oxford University Press. pp. 457–476. doi:10.1093/med/9780195371826.003.0031. ISBN 978-0-19-996521-2.
- Chapman R, Veit W (November 2021). "Correction to: The essence of autism: fact or artefact?". Molecular Psychiatry. 26 (11): 7069. doi:10.1038/s41380-021-01057-6. PMID 34697454. S2CID 239771302.
- Wazana A, Bresnahan M, Kline J (June 2007). "The autism epidemic: fact or artifact?". Journal of the American Academy of Child and Adolescent Psychiatry. 46 (6): 721–730. doi:10.1097/chi.0b013e31804a7f3b. PMID 17513984.
- DeStefano, Frank; Shimabukuro, Tom T. (29 September 2019). "The MMR Vaccine and Autism". Annual Review of Virology. 6 (1): 585–600. doi:10.1146/annurev-virology-092818-015515. ISSN 2327-0578. PMC 6768751. PMID 30986133.
- Geschwind DH (October 2008). "Autism: many genes, common pathways?". Cell. 135 (3): 391–395. doi:10.1016/j.cell.2008.10.016. PMC 2756410. PMID 18984147.
- Happé F (1999). "Understanding assets and deficits in autism: why success is more interesting than failure" (PDF). Psychologist. 12 (11): 540–547. Archived from the original (PDF) on 17 May 2012.
- Geschwind DH (2009). "Advances in autism". Annual Review of Medicine. 60: 367–380. doi:10.1146/annurev.med.60.053107.121225. PMC 3645857. PMID 19630577.
- "WHO releases new International Classification of Diseases (ICD 11)". World Health Organisation (Press Release). Retrieved 29 October 2021.
- Pickett D, Anderson RN (18 July 2018). Status on ICD-11: The WHO Launch (PDF) (Report). CDC/NCHS.
- ICD-11.
- "ICD vs. DSM". APA Monitor. Vol. 40, no. 9. American Psychological Association. 2009. p. 63.
- Mezzich JE (2002). "International surveys on the use of ICD-10 and related diagnostic systems". Psychopathology. 35 (2–3): 72–75. doi:10.1159/000065122. PMID 12145487. S2CID 35857872.
- Goldberg D (January 2010). "The classification of mental disorder: a simpler system for DSM–V and ICD–11". Advances in Psychiatric Treatment. 16 (1): 14–19. doi:10.1192/apt.bp.109.007120.
- American Psychiatric Association (18 May 2013). DSM-5. Diagnostic and Statistical Manual of Mental Disorders. Arlington County. doi:10.1176/APPI.BOOKS.9780890425596. ISBN 978-0-89042-554-1. OCLC 830807378. OL 27587204M. Wikidata Q3064664.
- DSM-5-TR, "Autism spectrum disorder encompasses disorders previously referred to as early infantile autism, childhood autism, Kanner's autism, high-functioning autism, atypical autism, pervasive developmental disorder not otherwise specified, childhood disintegrative disorder, and Asperger's disorder".
- Kulage KM, Smaldone AM, Cohn EG (August 2014). "How will DSM-5 affect autism diagnosis? A systematic literature review and meta-analysis". Journal of Autism and Developmental Disorders. 44 (8): 1918–32. doi:10.1007/s10803-014-2065-2. PMID 24531932. S2CID 18865395.
- "DSM-5 Diagnostic Criteria". U.S. Department of Health & Human Services Interagency Autism Coordinating Committee. Retrieved 17 May 2017.
- "F84. Pervasive developmental disorders". ICD-10: International Statistical Classification of Diseases and Related Health Problems: Tenth Revision. World Health Organization. 2007. Archived from the original on 21 April 2013. Retrieved 10 October 2009.
- Loukusa, Soile (2021). "Autism Spectrum Disorder". In Cummings, Louise (ed.). Handbook of pragmatic language disorders : complex and underserved populations. Cham, Switzerland: Springer. pp. 45–78. doi:10.1007/978-3-030-74985-9_3. ISBN 978-3-030-74984-2. OCLC 1269056169. S2CID 239160368.
- Pinel JP (2011). Biopsychology (8th ed.). Boston, Massachusetts: Pearson. p. 235. ISBN 978-0-205-03099-6. OCLC 1085798897.
- Hollander, Eric; Hagerman, Randi; Fein, Deborah, eds. (2018). Autism Spectrum Disorders. eBooks. Chapter 6: Cognitive Assessment. doi:10.1176/appi.books.9781615371921. ISBN 978-1-61537-192-1. Retrieved 12 September 2022.
- Autism spectrum disorder in adults: diagnosis and management, NICE, 14 June 2021, CG142, retrieved 24 October 2021
- "About autism spectrum disorder (ASD)". Government of Canada. 18 January 2016. Retrieved 4 November 2021.
- "What are the signs and symptoms of ASD?". Government of Canada. 18 January 2016. Retrieved 4 November 2021.
- National Center on Birth Defects and Developmental Disabilities (25 March 2020). "What is Autism Spectrum Disorder?". Centers for Disease Control and Prevention. Retrieved 24 October 2021.
- Filipek PA, Accardo PJ, Baranek GT, Cook EH, Dawson G, Gordon B, et al. (December 1999). "The screening and diagnosis of autistic spectrum disorders". Journal of Autism and Developmental Disorders. 29 (6): 439–484. doi:10.1023/A:1021943802493. PMID 10638459. S2CID 145113684. This paper represents a consensus of representatives from nine professional and four parent organizations in the US.
- Zhang Y, Han VZ (April 2018). "孤独症患者的偏才和获得性偏才现象及其神经生物学机理" [Neurobiological mechanisms of autistic savant and acquired savant]. 生理学报; Sheng Li Xue Bao; 'Acta Physiologica Sinica' (in Chinese). 70 (2): 201–210. PMID 29691585.
- Hughes JE, Ward J, Gruffydd E, Baron-Cohen S, Smith P, Allison C, Simner J (October 2018). "Savant syndrome has a distinct psychological profile in autism". Molecular Autism. 9: 53. doi:10.1186/s13229-018-0237-1. PMC 6186137. PMID 30344992.
- Tracy A Becerra-Culqui; Frances L Lynch; Ashli A Owen-Smith; Joseph Spitzer; Lisa A Croen (1 October 2018). "Parental First Concerns and Timing of Autism Spectrum Disorder Diagnosis". Journal of Autism and Developmental Disorders. 48 (10): 3367–3376. doi:10.1007/S10803-018-3598-6. ISSN 0162-3257. PMID 29754290. Wikidata Q88651632.
- Dwyer, Patrick; Ryan, Jacalyn G; Williams, Zachary J; Gassner, Dena L (1 April 2022). "First Do No Harm: Suggestions Regarding Respectful Autism Language". Pediatrics. American Academy of Pediatrics (AAP). 149 (Supplement 4). doi:10.1542/peds.2020-049437n. ISSN 0031-4005. PMC 9066426. PMID 35363298.
- Zwaigenbaum L, Bryson S, Lord C, Rogers S, Carter A, Carver L, et al. (May 2009). "Clinical assessment and management of toddlers with suspected autism spectrum disorder: insights from studies of high-risk infants". Pediatrics. 123 (5): 1383–91. doi:10.1542/peds.2008-1606. PMC 2833286. PMID 19403506.
- Lord C (November 1995). "Follow-up of two-year-olds referred for possible autism". Journal of Child Psychology and Psychiatry, and Allied Disciplines. 36 (8): 1365–82. doi:10.1111/j.1469-7610.1995.tb01669.x. eISSN 1469-7610. ISSN 0021-9630. OCLC 01307942. PMID 8988272.
- Rogers SJ (June 2009). "What are infant siblings teaching us about autism in infancy?". Autism Research. 2 (3): 125–137. doi:10.1002/aur.81. PMC 2791538. PMID 19582867.
- Rapin I, Tuchman RF (October 2008). "Autism: definition, neurobiology, screening, diagnosis". Pediatric Clinics of North America. 55 (5): 1129–46, viii. doi:10.1016/j.pcl.2008.07.005. PMID 18929056.
- Zwaigenbaum L (October 2001). "Autistic spectrum disorders in preschool children". Canadian Family Physician. 47 (10): 2037–42. PMC 2018435. PMID 11723598.
- Stefanatos GA (December 2008). "Regression in autistic spectrum disorders". Neuropsychology Review. 18 (4): 305–319. doi:10.1007/s11065-008-9073-y. PMID 18956241. S2CID 34658024.
- Halsey NA, Hyman SL (May 2001). "Measles-mumps-rubella vaccine and autistic spectrum disorder: report from the New Challenges in Childhood Immunizations Conference convened in Oak Brook, Illinois, June 12-13, 2000". Pediatrics. 107 (5): E84. doi:10.1542/peds.107.5.e84. PMID 11331734.
- Martínez-Pedraza F, Carter AS (July 2009). "Autism spectrum disorders in young children". Child and Adolescent Psychiatric Clinics of North America. 18 (3): 645–63. doi:10.1016/j.chc.2009.02.002. PMC 3166636. PMID 19486843.
- Werner E, Dawson G, Munson J, Osterling J (June 2005). "Variation in early developmental course in autism and its relation with behavioral outcome at 3-4 years of age". Journal of Autism and Developmental Disorders. 35 (3): 337–50. doi:10.1007/s10803-005-3301-6. PMID 16119475. S2CID 22485657.
- "Autism spectrum disorder – childhood disintegrative disorder: MedlinePlus Medical Encyclopedia". medlineplus.gov. Retrieved 8 May 2020.
- Annio Posar; Paola Visconti (23 September 2020). "Is it autism? Some suggestions for pediatricians". Türk pediatri arsivi Turkish Pediatrics Archive. 55 (3): 229–235. doi:10.14744/TURKPEDIATRIARS.2020.59862. ISSN 1306-0015. PMC 7536466. PMID 33061749. Wikidata Q100648906.
- Johnson CP, Myers SM (November 2007). "Identification and evaluation of children with autism spectrum disorders". Pediatrics. 120 (5): 1183–1215. doi:10.1542/peds.2007-2361. PMID 17967920. Archived from the original on 8 February 2009.
- Ozonoff S, Heung K, Byrd R, Hansen R, Hertz-Picciotto I (December 2008). "The onset of autism: patterns of symptom emergence in the first years of life". Autism Research. 1 (6): 320–328. doi:10.1002/aur.53. PMC 2857525. PMID 19360687.
- CDC (18 August 2016). "Part II: A Closer Look". Centers for Disease Control and Prevention. Retrieved 15 September 2022.
- CDC (18 August 2016). "Part II: A Closer Look". Centers for Disease Control and Prevention. Retrieved 15 September 2022.
- Ozonoff, Sally; Iosif, Ana-Maria (1 May 2019). "Changing conceptualizations of regression: What prospective studies reveal about the onset of autism spectrum disorder". Neuroscience & Biobehavioral Reviews. 100: 296–304. doi:10.1016/j.neubiorev.2019.03.012. ISSN 0149-7634. PMC 6451681. PMID 30885812.
- Mash EJ, Barkley RA (2003). Child Psychopathology. New York: The Guilford Press. pp. 409–454. ISBN 9781572306097.
- Ellis Weismer S, Kover ST (December 2015). "Preschool language variation, growth, and predictors in children on the autism spectrum". Journal of Child Psychology and Psychiatry, and Allied Disciplines. 56 (12): 1327–37. doi:10.1111/jcpp.12406. eISSN 1469-7610. ISSN 0021-9630. OCLC 01307942. PMC 4565784. PMID 25753577.
- Dawson G, Osterling J (1997). "Early Intervention in Autism". In Guralnick MJ (ed.). The effectiveness of early intervention. Baltimore: Brookes. pp. 307–326. ISBN 1-55766-255-X. OCLC 34411043. ERIC ED414694.
- CDC (31 March 2022). "Basics About Autism Spectrum Disorder (ASD) | NCBDDD | CDC". Centers for Disease Control and Prevention. Retrieved 15 September 2022.
- Barnhill GP (2007). "Outcomes in adults with Asperger syndrome". Focus on Autism and Other Developmental Disabilities. 22 (2): 116–126. doi:10.1177/10883576070220020301. S2CID 1355689.
- Howlin P, Moss P (May 2012). "Adults with autism spectrum disorders". Canadian Journal of Psychiatry. 57 (5): 275–83. doi:10.1177/070674371205700502. PMID 22546059. S2CID 44544407.
- Frye RE (August 2018). "Social Skills Deficits in Autism Spectrum Disorder: Potential Biological Origins and Progress in Developing Therapeutic Agents". CNS Drugs. 32 (8): 713–734. doi:10.1007/s40263-018-0556-y. PMC 6105175. PMID 30105528.
- Augustyn M. "Autism spectrum disorder: Clinical features". UpToDate. Retrieved 22 March 2020.
- Bird G, Cook R (July 2013). "Mixed emotions: the contribution of alexithymia to the emotional symptoms of autism". Translational Psychiatry. 3 (7): e285. doi:10.1038/tp.2013.61. PMC 3731793. PMID 23880881.
- National Center on Birth Defects and Developmental Disabilities (29 June 2020). "Diagnostic Criteria: Autism Spectrum Disorder (ASD)". Centers for Disease Control and Prevention. Retrieved 21 February 2021.
- "Autism Spectrum Disorder: Communication Problems in Children". NIDCD. 18 August 2015. Retrieved 17 December 2017.
- Vicker B. "Social communication and language characteristics associated with high-functioning, verbal children and adults with autism spectrum disorder". Indiana Resource Center for Autism. Retrieved 17 December 2017.
- Lawson W (2001). Understanding and Working With the Spectrum of Autism: An Insider's View. London UK, & Philadelphia PA: Jessica Kingsley Publishers. pp. 33. ISBN 978-1853029714.
- Fusaroli R, Lambrechts A, Bang D, Bowler DM, Gaigg SB (March 2017). "Is voice a marker for Autism spectrum disorder? A systematic review and meta-analysis" (PDF). Autism Research. 10 (3): 384–407. doi:10.1002/aur.1678. PMID 27501063. S2CID 13772771.
- "Autism: Overview". American Speech-Language-Hearing Association. Retrieved 17 December 2017.
- Cohen, David; Grandin, Temple (25 October 2005). "Temple Grandin: 'I'm an anthropologist from Mars'". The Guardian. Kings Place, London: Scott Trust. eISSN 1756-3224. ISSN 0261-3077. OCLC 60623878. Archived from the original on 9 November 2013. Retrieved 6 July 2022.
- Keating CT, Cook JL (July 2020). "Facial expression production and recognition in autism spectrum disorders: a shifting landscape". Child Adolesc Psychiatr Clin N Am (Review). 29 (3): 557–571. doi:10.1016/j.chc.2020.02.006. PMID 32471602.
- Tager-Flusberg H, Caronna E (June 2007). "Language disorders: autism and other pervasive developmental disorders". Pediatric Clinics of North America. 54 (3): 469–81, vi. doi:10.1016/j.pcl.2007.02.011. PMID 17543905.
- Volkmar FR, Paul R, Pelphrey KA, Rogers SJ, eds. (2014). Handbook of Autism and Pervasive Developmental Disorders: Volume Two: Assessment, Interventions, and Policy. Vol. 2 (4th ed.). Hoboken, New Jersey: John Wiley & Sons. p. 301. ISBN 978-1-118-28220-5. LCCN 2013034363. OCLC 946133861. Retrieved 1 March 2019.
- National Center on Birth Defects and Developmental Disabilities (26 February 2015). "Signs & Symptoms: Autism Spectrum Disorder". Centers for Disease Control and Prevention. Archived from the original on 10 March 2015. (Also available in Spanish.)
- "Engaging people on the autism spectrum". Autism Spectrum Australia. 7 October 2013. Archived from the original on 19 March 2020.
- Hinerman PS (1983). Teaching Autistic Children to Communicate. Rockville, Maryland: Aspens System Corporation. p. 180. ISBN 978-0-89443-884-4.
- Lord C, Elsabbagh M, Baird G, Veenstra-Vanderweele J (August 2018). "Autism spectrum disorder". Lancet. 392 (10146): 508–520. doi:10.1016/S0140-6736(18)31129-2. PMC 7398158. PMID 30078460. S2CID 51922565.
- DSM-5-TR, "Hyper- or hyporeactivity to sensory input or unusual interest in sensory aspects of the environment (e.g., apparent indifference to pain/temperature, adverse response to specific sounds or textures, excessive smelling or touching of objects, visual fascination with lights or movement)".
- Lam KS, Aman MG (May 2007). "The Repetitive Behavior Scale-Revised: independent validation in individuals with autism spectrum disorders". Journal of Autism and Developmental Disorders. 37 (5): 855–866. doi:10.1007/s10803-006-0213-z. PMID 17048092. S2CID 41034513.
- Minshawi NF, Hurwitz S, Fodstad JC, Biebl S, Morriss DH, McDougle CJ (April 2014). "The association between self-injurious behaviors and autism spectrum disorders". Psychology Research and Behavior Management. 7: 125–36. doi:10.2147/PRBM.S44635. PMC 3990505. PMID 24748827.
- Oliver C, Richards C (October 2015). "Practitioner Review: Self-injurious behaviour in children with developmental delay" (PDF). J Child Psychol Psychiatry (Review). 56 (10): 1042–54. doi:10.1111/jcpp.12425. PMID 25916173.
- Flowers, Jacqueline; Lantz, Johanna; Hamlin, Terry; Simeonsson, Rune J. (1 August 2020). "Associated Factors of Self-injury Among Adolescents with Autism Spectrum Disorder in a Community and Residential Treatment Setting". Journal of Autism and Developmental Disorders. 50 (8): 2987–3004. doi:10.1007/s10803-020-04389-4. ISSN 1573-3432. PMID 32056114. S2CID 211111895.
- Treffert DA (May 2009). "The savant syndrome: an extraordinary condition. A synopsis: past, present, future". Philosophical Transactions of the Royal Society of London. Series B, Biological Sciences. 364 (1522): 1351–1357. doi:10.1098/rstb.2008.0326. PMC 2677584. PMID 19528017.
- Plaisted Grant K, Davis G (May 2009). "Perception and apperception in autism: rejecting the inverse assumption". Philosophical Transactions of the Royal Society of London. Series B, Biological Sciences. 364 (1522): 1393–1398. doi:10.1098/rstb.2009.0001. PMC 2677593. PMID 19528022.
- Ben-Sasson A, Hen L, Fluss R, Cermak SA, Engel-Yeger B, Gal E (January 2009). "A meta-analysis of sensory modulation symptoms in individuals with autism spectrum disorders". Journal of Autism and Developmental Disorders. 39 (1): 1–11. doi:10.1007/s10803-008-0593-3. PMID 18512135. S2CID 5208889.
- Gargot T, Archambault D, Chetouani M, Cohen D, Johal W, Anzalone SM (10 January 2022). "Automatic Assessment of Motor Impairments in Autism Spectrum Disorders: A Systematic Review" (PDF). Cognitive Computation. 14 (2): 624–659. doi:10.1007/s12559-021-09940-8. ISSN 1866-9964. S2CID 248326222.
- Fournier KA, Hass CJ, Naik SK, Lodha N, Cauraugh JH (October 2010). "Motor coordination in autism spectrum disorders: a synthesis and meta-analysis". Journal of Autism and Developmental Disorders. 40 (10): 1227–1240. doi:10.1007/s10803-010-0981-3. PMID 20195737. S2CID 3469612.
- Dominick KC, Davis NO, Lainhart J, Tager-Flusberg H, Folstein S (2007). "Atypical behaviors in children with autism and children with a history of language impairment". Research in Developmental Disabilities. Elsevier. 28 (2): 145–162. doi:10.1016/j.ridd.2006.02.003. eISSN 1873-3379. ISSN 0891-4222. PMID 16581226.
- Van Der Miesen AI, Hurley H, De Vries AL (2016). "Gender dysphoria and autism spectrum disorder: A narrative review". International Review of Psychiatry. 28 (1): 70–80. doi:10.3109/09540261.2015.1111199. PMID 26753812. S2CID 20918937.
- Glidden D, Bouman WP, Jones BA, Arcelus J (January 2016). "Gender Dysphoria and Autism Spectrum Disorder: A Systematic Review of the Literature". Sexual Medicine Reviews. 4 (1): 3–14. doi:10.1016/j.sxmr.2015.10.003. PMID 27872002. S2CID 3454600.
- Weir E, Allison C, Baron-Cohen S (November 2021). "The sexual health, orientation, and activity of autistic adolescents and adults". Autism Research. 14 (11): 2342–2354. doi:10.17863/CAM.74771. PMID 34536071.
- Israelyan N, Margolis KG (June 2018). "Serotonin as a link between the gut-brain-microbiome axis in autism spectrum disorders". Pharmacological Research (Review). 132: 1–6. doi:10.1016/j.phrs.2018.03.020. PMC 6368356. PMID 29614380.
- Wasilewska J, Klukowski M (2015). "Gastrointestinal symptoms and autism spectrum disorder: links and risks - a possible new overlap syndrome". Pediatric Health, Medicine and Therapeutics (Review). 6: 153–166. doi:10.2147/PHMT.S85717. PMC 5683266. PMID 29388597.
- Orsmond GI, Seltzer MM (2007). "Siblings of individuals with autism spectrum disorders across the life course" (PDF). Developmental Disabilities Research Reviews. 13 (4): 313–320. CiteSeerX 10.1.1.359.7273. doi:10.1002/mrdd.20171. PMID 17979200. Archived from the original (PDF) on 30 May 2013.
- Happé F, Ronald A (December 2008). "The 'fractionable autism triad': a review of evidence from behavioural, genetic, cognitive and neural research". Neuropsychology Review. 18 (4): 287–304. doi:10.1007/s11065-008-9076-8. PMID 18956240. S2CID 13928876.
- Happé F, Ronald A, Plomin R (October 2006). "Time to give up on a single explanation for autism". Nature Neuroscience. 9 (10): 1218–1220. doi:10.1038/nn1770. PMID 17001340.
- Tager-Flusberg H (2010). "The origins of social impairments in autism spectrum disorder: studies of infants at risk". Neural Networks. 23 (8–9): 1072–6. doi:10.1016/j.neunet.2010.07.008. PMC 2956843. PMID 20800990.
- Altevogt BM, Hanson SL, Leshner AI (June 2008). "Autism and the environment: challenges and opportunities for research". Pediatrics. 121 (6): 1225–1229. doi:10.1542/peds.2007-3000. PMID 18519493. S2CID 24595814. Archived from the original on 15 January 2010.
- Reiss AL (January 2009). "Childhood developmental disorders: an academic and clinical convergence point for psychiatry, neurology, psychology and pediatrics". Journal of Child Psychology and Psychiatry, and Allied Disciplines. 50 (1–2): 87–98. doi:10.1111/j.1469-7610.2008.02046.x. eISSN 1469-7610. ISSN 0021-9630. OCLC 01307942. PMC 5756732. PMID 19220592.
- Piggot J, Shirinyan D, Shemmassian S, Vazirian S, Alarcón M (November 2009). "Neural systems approaches to the neurogenetics of autism spectrum disorders". Neuroscience. 164 (1): 247–256. doi:10.1016/j.neuroscience.2009.05.054. PMID 19482063. S2CID 207246176.
- Levy SE, Mandell DS, Schultz RT (November 2009). "Autism". Lancet. 374 (9701): 1627–1638. doi:10.1016/S0140-6736(09)61376-3. PMC 2863325. PMID 19819542. (Erratum: doi:10.1016/S0140-6736(11)61666-8, )
- Stephan DA (January 2008). "Unraveling autism". American Journal of Human Genetics. 82 (1): 7–9. doi:10.1016/j.ajhg.2007.12.003. PMC 2253980. PMID 18179879.
- Brown EA, Lautz JD, Davis TR, Gniffke EP, VanSchoiack AA, Neier SC, et al. (2018). "Clustering the autisms using glutamate synapse protein interaction networks from cortical and hippocampal tissue of seven mouse models". Molecular Autism. 9 (48): 48. doi:10.1186/s13229-018-0229-1. PMC 6139139. PMID 30237867.
- Abrahams BS, Geschwind DH (May 2008). "Advances in autism genetics: on the threshold of a new neurobiology". Nature Reviews. Genetics. 9 (5): 341–355. doi:10.1038/nrg2346. PMC 2756414. PMID 18414403.
- Buxbaum JD (2009). "Multiple rare variants in the etiology of autism spectrum disorders". Dialogues in Clinical Neuroscience. 11 (1): 35–43. doi:10.31887/DCNS.2009.11.1/jdbuxbaum. PMC 3181906. PMID 19432386.
- Sanders SJ, He X, Willsey AJ, Ercan-Sencicek AG, Samocha KE, Cicek AE, et al. (September 2015). "Insights into Autism Spectrum Disorder Genomic Architecture and Biology from 71 Risk Loci". Neuron. 87 (6): 1215–1233. doi:10.1016/j.neuron.2015.09.016. PMC 4624267. PMID 26402605.
- Persico AM, Napolioni V (August 2013). "Autism genetics". Behavioural Brain Research. 251: 95–112. doi:10.1016/j.bbr.2013.06.012. PMID 23769996. S2CID 15721666.
- Cook EH, Scherer SW (October 2008). "Copy-number variations associated with neuropsychiatric conditions". Nature. 455 (7215): 919–923. Bibcode:2008Natur.455..919C. doi:10.1038/nature07458. PMID 18923514. S2CID 4377899.
- Brandler WM, Antaki D, Gujral M, Noor A, Rosanio G, Chapman TR, et al. (April 2016). "Frequency and Complexity of De Novo Structural Mutation in Autism". American Journal of Human Genetics. 98 (4): 667–679. doi:10.1016/j.ajhg.2016.02.018. PMC 4833290. PMID 27018473.
- Beaudet AL (May 2007). "Autism: highly heritable but not inherited". Nature Medicine. 13 (5): 534–536. doi:10.1038/nm0507-534. PMID 17479094. S2CID 11673879.
- Nishiyama M, Oshikawa K, Tsukada Y, Nakagawa T, Iemura S, Natsume T, Fan Y, Kikuchi A, Skoultchi AI, Nakayama KI (18 January 2009). "CHD8 suppresses p53-mediated apoptosis through histone H1 recruitment during early embryogenesis". Nature Cell Biology. 11 (2): 172–182. doi:10.1038/ncb1831. ISSN 1465-7392. PMC 3132516. PMID 19151705.
- Ronan JL, Wu W, Crabtree GR (9 April 2013). "From neural development to cognition: unexpected roles for chromatin". Nature Reviews Genetics. 14 (5): 347–359. doi:10.1038/nrg3413. ISSN 1471-0056. PMC 4010428. PMID 23568486.
- Thompson BA, Tremblay V, Lin G, Bochar DA (15 June 2008). "CHD8 Is an ATP-Dependent Chromatin Remodeling Factor That Regulates β-Catenin Target Genes". Molecular and Cellular Biology. 28 (12): 3894–3904. doi:10.1128/mcb.00322-08. ISSN 0270-7306. PMC 2423111. PMID 18378692.
- Sugathan A, Biagioli M, Golzio C, Erdin S, Blumenthal I, Manavalan P, Ragavendran A, Brand H, Lucente D, Miles J, Sheridan SD (7 October 2014). "CHD8 regulates neurodevelopmental pathways associated with autism spectrum disorder in neural progenitors". Proceedings of the National Academy of Sciences. 111 (42): E4468-77. Bibcode:2014PNAS..111E4468S. doi:10.1073/pnas.1405266111. ISSN 0027-8424. PMC 4210312. PMID 25294932.
- Cotney J, Muhle RA, Sanders SJ, Liu L, Willsey AJ, Niu W, Liu W, Klei L, Lei J, Yin J, Reilly SK (10 March 2015). "The autism-associated chromatin modifier CHD8 regulates other autism risk genes during human neurodevelopment". Nature Communications. 6 (1): 6404. Bibcode:2015NatCo...6.6404C. doi:10.1038/ncomms7404. ISSN 2041-1723. PMC 4355952. PMID 25752243.
- Wilkinson B, Grepo N, Thompson BL, Kim J, Wang K, Evgrafov OV, Lu W, Knowles JA, Campbell DB (May 2015). "The autism-associated gene chromodomain helicase DNA-binding protein 8 (CHD8) regulates noncoding RNAs and autism-related genes". Translational Psychiatry. 5 (5): e568. doi:10.1038/tp.2015.62. ISSN 2158-3188. PMC 4471293. PMID 25989142.
- Cerase A, Young AN, Ruiz NB, Buness A, Sant GM, Arnold M, Di Giacomo M, Ascolani M, Kumar M, Hierholzer A, Trigiante G (15 April 2021). "Chd8 regulates X chromosome inactivation in mouse through fine-tuning control of Xist expression". Communications Biology. 4 (1): 485. doi:10.1038/s42003-021-01945-1. ISSN 2399-3642. PMC 8050208. PMID 33859315.
- Crespi BJ (30 June 2016). "Autism As a Disorder of High Intelligence". Frontiers in Neuroscience. 10: 300. doi:10.3389/fnins.2016.00300. PMC 4927579. PMID 27445671.
- Baron-Cohen S (10 November 2020). The pattern seekers: how autism drives human invention. ISBN 978-1-5416-4713-8. OCLC 1204602315.
- Chen JA, Peñagarikano O, Belgard TG, Swarup V, Geschwind DH (2015). "The emerging picture of autism spectrum disorder: genetics and pathology". Annu Rev Pathol (Review). 10: 111–44. doi:10.1146/annurev-pathol-012414-040405. PMID 25621659.
- Werling DM, Brand H, An JY, Stone MR, Zhu L, Glessner JT, et al. (April 2018). "An analytical framework for whole-genome sequence association studies and its implications for autism spectrum disorder". Nature Genetics. 50 (5): 727–736. doi:10.1038/s41588-018-0107-y. PMC 5961723. PMID 29700473.
- Devlin H (14 September 2018). "Thousands of autistic girls and women 'going undiagnosed' due to gender bias". The Guardian.
- Crespi B, Badcock C (June 2008). "Psychosis and autism as diametrical disorders of the social brain" (PDF). The Behavioral and Brain Sciences. 31 (3): 241–61, discussion 261–320. doi:10.1017/S0140525X08004214. PMID 18578904.
- Crespi B, Stead P, Elliot M (January 2010). "Evolution in health and medicine Sackler colloquium: Comparative genomics of autism and schizophrenia". Proceedings of the National Academy of Sciences of the United States of America. 107 (Suppl 1): 1736–1741. Bibcode:2010PNAS..107.1736C. doi:10.1073/pnas.0906080106. PMC 2868282. PMID 19955444.
- Baron-Cohen S, Knickmeyer RC, Belmonte MK (November 2005). "Sex differences in the brain: implications for explaining autism" (PDF). Science. 310 (5749): 819–823. Bibcode:2005Sci...310..819B. doi:10.1126/science.1115455. PMID 16272115. S2CID 44330420.
- Gardener H, Spiegelman D, Buka SL (August 2011). "Perinatal and neonatal risk factors for autism: a comprehensive meta-analysis". Pediatrics. 128 (2): 344–55. doi:10.1542/peds.2010-1036. PMC 3387855. PMID 21746727.
- Gardener H, Spiegelman D, Buka SL (July 2009). "Prenatal risk factors for autism: comprehensive meta-analysis". The British Journal of Psychiatry. 195 (1): 7–14. doi:10.1192/bjp.bp.108.051672. PMC 3712619. PMID 19567888.
- Mazahery H, Camargo CA, Conlon C, Beck KL, Kruger MC, von Hurst PR (April 2016). "Vitamin D and Autism Spectrum Disorder: A Literature Review". Nutrients. 8 (4): 236. doi:10.3390/nu8040236. PMC 4848704. PMID 27110819.
- Vohr BR, Poggi Davis E, Wanke CA, Krebs NF (April 2017). "Neurodevelopment: The Impact of Nutrition and Inflammation During Preconception and Pregnancy in Low-Resource Settings". Pediatrics (Review). 139 (Suppl 1): S38–S49. doi:10.1542/peds.2016-2828F. PMID 28562247. S2CID 28637473.
- Samsam M, Ahangari R, Naser SA (August 2014). "Pathophysiology of autism spectrum disorders: revisiting gastrointestinal involvement and immune imbalance". World Journal of Gastroenterology (Review). 20 (29): 9942–9951. doi:10.3748/wjg.v20.i29.9942. PMC 4123375. PMID 25110424.
- Lyall K, Schmidt RJ, Hertz-Picciotto I (April 2014). "Maternal lifestyle and environmental risk factors for autism spectrum disorders". International Journal of Epidemiology. 43 (2): 443–464. doi:10.1093/ije/dyt282. PMC 3997376. PMID 24518932.
- Lam J, Sutton P, Kalkbrenner A, Windham G, Halladay A, Koustas E, et al. (2016). "A Systematic Review and Meta-Analysis of Multiple Airborne Pollutants and Autism Spectrum Disorder". PLOS ONE. 11 (9): e0161851. Bibcode:2016PLoSO..1161851L. doi:10.1371/journal.pone.0161851. PMC 5031428. PMID 27653281.
- Newschaffer CJ, Croen LA, Daniels J, Giarelli E, Grether JK, Levy SE, et al. (2007). "The epidemiology of autism spectrum disorders". Annual Review of Public Health. 28: 235–58. doi:10.1146/annurev.publhealth.28.021406.144007. PMID 17367287.
- Kinney DK, Munir KM, Crowley DJ, Miller AM (October 2008). "Prenatal stress and risk for autism". Neuroscience and Biobehavioral Reviews. 32 (8): 1519–1532. doi:10.1016/j.neubiorev.2008.06.004. PMC 2632594. PMID 18598714.
- Hussain A, Ali S, Ahmed M, Hussain S (July 2018). "The Anti-vaccination Movement: A Regression in Modern Medicine". Cureus. 10 (7): e2919. doi:10.7759/cureus.2919. PMC 6122668. PMID 30186724.
- Spencer JP, Trondsen Pawlowski RH, Thomas S (June 2017). "Vaccine Adverse Events: Separating Myth from Reality". American Family Physician. 95 (12): 786–794. PMID 28671426.
- Di Pietrantonj C, Rivetti A, Marchione P, Debalini MG, Demicheli V (November 2021). "Vaccines for measles, mumps, rubella, and varicella in children". The Cochrane Database of Systematic Reviews. 2021 (11): CD004407. doi:10.1002/14651858.CD004407.pub5. PMC 8607336. PMID 34806766.
- Gerber JS, Offit PA (February 2009). "Vaccines and autism: a tale of shifting hypotheses". Clinical Infectious Diseases. 48 (4): 456–461. doi:10.1086/596476. PMC 2908388. PMID 19128068.
- Deer B (8 February 2009). "MMR doctor Andrew Wakefield fixed data on autism". The Sunday Times.
- Boseley S (2 February 2010). "Lancet retracts 'utterly false' MMR paper". The Guardian.
- Stratton K, Ford A, Rusch E, Clayton EW, eds. (August 2011). "Influenza Vaccine". Adverse Effects of Vaccines: Evidence and Causality. Committee to Review Adverse Effects of Vaccines, Board on Population Health and Public Health Practice. Washington, D.C.: Institute of Medicine/National Academies Press. doi:10.17226/13164. ISBN 978-0-309-21435-3. PMID 24624471.
- Flaherty DK (October 2011). "The vaccine-autism connection: a public health crisis caused by unethical medical practices and fraudulent science". The Annals of Pharmacotherapy. 45 (10): 1302–1304. doi:10.1345/aph.1Q318. PMID 21917556. S2CID 39479569.
- Godlee F, Smith J, Marcovitch H (January 2011). "Wakefield's article linking MMR vaccine and autism was fraudulent". BMJ. 342: c7452. doi:10.1136/bmj.c7452. PMID 21209060. S2CID 43640126.
- Tan M, Parkin JE (November 2000). "Route of decomposition of thiomersal (thimerosal)". International Journal of Pharmaceutics. 208 (1–2): 23–34. doi:10.1016/S0378-5173(00)00514-7. PMID 11064208.
- Waterhouse L (December 2008). "Autism overflows: increasing prevalence and proliferating theories". Neuropsychology Review. 18 (4): 273–286. doi:10.1007/s11065-008-9074-x. PMID 19015994. S2CID 8863638.
- "Frequently Asked Questions about Thimerosal". Centers for Disease Control and Prevention. Retrieved 21 February 2017.
- Taylor LE, Swerdfeger AL, Eslick GD (June 2014). "Vaccines are not associated with autism: an evidence-based meta-analysis of case-control and cohort studies". Vaccine. 32 (29): 3623–3629. doi:10.1016/j.vaccine.2014.04.085. PMID 24814559.
- Vaccines and autism:
- Doja A, Roberts W (November 2006). "Immunizations and autism: a review of the literature". The Canadian Journal of Neurological Sciences. Le Journal Canadien des Sciences Neurologiques. 33 (4): 341–346. doi:10.1017/s031716710000528x. PMID 17168158.
- Gerber JS, Offit PA (February 2009). "Vaccines and autism: a tale of shifting hypotheses". Clinical Infectious Diseases. 48 (4): 456–461. doi:10.1086/596476. PMC 2908388. PMID 19128068.
- Gross L (May 2009). "A broken trust: lessons from the vaccine--autism wars". PLOS Biology. 7 (5): e1000114. doi:10.1371/journal.pbio.1000114. PMC 2682483. PMID 19478850.
- Paul R (June 2009). "Parents ask: Am I risking autism if I vaccinate my children?". Journal of Autism and Developmental Disorders. 39 (6): 962–963. doi:10.1007/s10803-009-0739-y. PMID 19363650. S2CID 34467853.
- Poland GA, Jacobson RM (January 2011). "The age-old struggle against the antivaccinationists". The New England Journal of Medicine. 364 (2): 97–99. doi:10.1056/NEJMp1010594. PMID 21226573.
- McBrien J, Murphy J, Gill D, Cronin M, O'Donovan C, Cafferkey MT (July 2003). "Measles outbreak in Dublin, 2000". The Pediatric Infectious Disease Journal. 22 (7): 580–584. doi:10.1097/00006454-200307000-00002. PMID 12867830.
- Sarovic D (November 2021). "A Unifying Theory for Autism: The Pathogenetic Triad as a Theoretical Framework". Frontiers in Psychiatry (Review). 12: 767075. doi:10.3389/fpsyt.2021.767075. PMC 8637925. PMID 34867553. S2CID 244119594.
- Markram, Kamila; Markram, Henry (21 December 2010). "The Intense World Theory – a unifying theory of the neurobiology of autism". Frontiers in Human Neuroscience (Review). 4: 224. doi:10.3389/fnhum.2010.00224. ISSN 1662-5161. PMC 3010743. PMID 21191475.
The proposed neuropathology is hyper-functioning of local neural microcircuits, best characterized by hyper-reactivity and hyper-plasticity. Such hyper-functional microcircuits are speculated to become autonomous and memory trapped leading to the core cognitive consequences of hyper-perception, hyper-attention, hyper-memory and hyper-emotionality. The theory is centered on the neocortex and the amygdala, but could potentially be applied to all brain regions. (...) This may lead to obsessively detailed information processing of fragments of the world and an involuntarily and systematic decoupling of the autist from what becomes a painfully intense world.
- Spikins, Penny (27 March 2017). "How our autistic ancestors played an important role in human evolution". The Conversation.
- Spikins, Penny (6 March 2013). "The Stone Age Origins of Autism". In Fitzgerald, Michael (ed.). Recent Advances in Autism Spectrum Disorders - Volume II.
- Lomelin, David E. (2010). "An Examination of Autism Spectrum Disorders in Relation to Human Evolution and Life History Theory". Nebraska Anthropologist. 57.
- Reser, Jared Edward (1 April 2011). "Conceptualizing the Autism Spectrum in Terms of Natural Selection and Behavioral Ecology: The Solitary Forager Hypothesis". Evolutionary Psychology. 9 (2): 207–238. doi:10.1177/147470491100900209. ISSN 1474-7049. PMID 22947969. S2CID 25378900.
- "Autism may have had advantages in humans' hunter-gatherer past, researcher believes". ScienceDaily. University of Southern California. 3 June 2011.
- Rudacille, Deborah (8 July 2011). "Lonely hunters". Spectrum.
- Spikins, Penny; Wright, Barry; Hodgson, Derek (1 October 2016). "Are there alternative adaptive strategies to human pro-sociality? The role of collaborative morality in the emergence of personality variation and autistic traits". Time and Mind. 9 (4): 289–313. doi:10.1080/1751696X.2016.1244949. ISSN 1751-696X. S2CID 151820168.
- Harvard University (11 January 2020). "Ongoing human evolution could explain recent rise in certain disorders". ScienceDaily. Retrieved 24 May 2020.
- Penn HE (February 2006). "Neurobiological correlates of autism: a review of recent research". Child Neuropsychology. 12 (1): 57–79. doi:10.1080/09297040500253546. PMID 16484102. S2CID 46119993.
- London E (October 2007). "The role of the neurobiologist in redefining the diagnosis of autism". Brain Pathology. 17 (4): 408–411. doi:10.1111/j.1750-3639.2007.00103.x. PMC 8095627. PMID 17919126. S2CID 24860348.
- Rao M, Gershon MD (September 2016). "The bowel and beyond: the enteric nervous system in neurological disorders". Nature Reviews. Gastroenterology & Hepatology (Review). 13 (9): 517–528. doi:10.1038/nrgastro.2016.107. PMC 5005185. PMID 27435372.
immune dysregulation, GI inflammation, malfunction of the ANS, genetic and metabolic activity of the microbiome, and dietary metabolites may contribute to brain dysfunction and neuroinflammation depending upon individual genetic vulnerability
- Betancur C, Sakurai T, Buxbaum JD (July 2009). "The emerging role of synaptic cell-adhesion pathways in the pathogenesis of autism spectrum disorders" (PDF). Trends in Neurosciences. 32 (7): 402–412. doi:10.1016/j.tins.2009.04.003. PMID 19541375. S2CID 8644511.
- Arndt TL, Stodgell CJ, Rodier PM (2005). "The teratology of autism". International Journal of Developmental Neuroscience. 23 (2–3): 189–199. doi:10.1016/j.ijdevneu.2004.11.001. PMID 15749245. S2CID 17797266.
- Koenig K, Tsatsanis KD, Volkmar FR (2001). "Neurobiology and Genetics of Autism: A Developmental Perspective". In Burack JA, Charman T, Yirmiya N, Zelazo PR (eds.). The development of autism: perspectives from theory and research. Mahwah, N.J.: L. Erlbaum. pp. 73–92. ISBN 9780805832457. OCLC 806185029.
- Minshew NJ (April 1996). "Brief report: brain mechanisms in autism: functional and structural abnormalities". Journal of Autism and Developmental Disorders. 26 (2): 205–9. doi:10.1007/BF02172013. PMID 8744486. S2CID 8134205.
- Stanfield AC, McIntosh AM, Spencer MD, Philip R, Gaur S, Lawrie SM (June 2008). "Towards a neuroanatomy of autism: a systematic review and meta-analysis of structural magnetic resonance imaging studies". European Psychiatry. 23 (4): 289–99. doi:10.1016/j.eurpsy.2007.05.006. PMID 17765485. S2CID 29070618.
- Lefebvre A, Beggiato A, Bourgeron T, Toro R (July 2015). "Neuroanatomical Diversity of Corpus Callosum and Brain Volume in Autism: Meta-analysis, Analysis of the Autism Brain Imaging Data Exchange Project, and Simulation". Biological Psychiatry. 78 (2): 126–34. doi:10.1016/j.biopsych.2015.02.010. PMID 25850620. S2CID 8794474.
- Sugranyes G, Kyriakopoulos M, Corrigall R, Taylor E, Frangou S (2011). "Autism spectrum disorders and schizophrenia: meta-analysis of the neural correlates of social cognition". PLOS ONE. 6 (10): e25322. Bibcode:2011PLoSO...625322S. doi:10.1371/journal.pone.0025322. PMC 3187762. PMID 21998649.
- O'Reilly C, Lewis JD, Elsabbagh M (2017). "Is functional brain connectivity atypical in autism? A systematic review of EEG and MEG studies". PLOS ONE (Review). 12 (5): e0175870. Bibcode:2017PLoSO..1275870O. doi:10.1371/journal.pone.0175870. PMC 5414938. PMID 28467487.
- Al-Beltagi, Mohammed (9 May 2021). "Autism medical comorbidities". World Journal of Clinical Pediatrics. 10 (3): 15–28. doi:10.5409/wjcp.v10.i3.15. PMC 8085719. PMID 33972922.
Gastrointestinal (GI) disorders are significantly more common in children with ASD; they occur in 46% to 84% of them.
- Azhari A, Azizan F, Esposito G (July 2019). "A systematic review of gut-immune-brain mechanisms in Autism Spectrum Disorder". Developmental Psychobiology. 61 (s5): 752–771. doi:10.1002/dev.21803. hdl:10220/49107. PMID 30523646. S2CID 54523742.
- Fadiga L, Craighero L, Olivier E (April 2005). "Human motor cortex excitability during the perception of others' action". Current Opinion in Neurobiology. 15 (2): 213–8. doi:10.1016/j.conb.2005.03.013. PMID 15831405. S2CID 10511430.
- Shamay-Tsoory SG (February 2011). "The neural bases for empathy". The Neuroscientist. 17 (1): 18–24. doi:10.1177/1073858410379268. PMID 21071616. S2CID 2646438.
- Dinstein I, Thomas C, Behrmann M, Heeger DJ (January 2008). "A mirror up to nature". Current Biology. 18 (1): R13-8. doi:10.1016/j.cub.2007.11.004. PMC 2517574. PMID 18177704.
- Kalat J (2009). Biological Psychology (Tenth ed.). pp. 237–8. ISBN 978-0-495-60300-9.
- Kennedy DP, Adolphs R (November 2012). "The social brain in psychiatric and neurological disorders". Trends in Cognitive Sciences. 16 (11): 559–72. doi:10.1016/j.tics.2012.09.006. PMC 3606817. PMID 23047070.
- Schultz RT (2005). "Developmental deficits in social perception in autism: the role of the amygdala and fusiform face area". International Journal of Developmental Neuroscience. 23 (2–3): 125–41. doi:10.1016/j.ijdevneu.2004.12.012. PMID 15749240. S2CID 17078137.
- Haas RH, Parikh S, Falk MJ, Saneto RP, Wolf NI, Darin N, Cohen BH (December 2007). "Mitochondrial disease: a practical approach for primary care physicians". Pediatrics. 120 (6): 1326–1333. doi:10.1542/peds.2007-0391. PMID 18055683. S2CID 4939996.
- Rossignol DA, Frye RE (March 2012). "Mitochondrial dysfunction in autism spectrum disorders: a systematic review and meta-analysis". Molecular Psychiatry. 17 (3): 290–314. doi:10.1038/mp.2010.136. PMC 3285768. PMID 21263444.
- Gentile S (August 2015). "Prenatal antidepressant exposure and the risk of autism spectrum disorders in children. Are we looking at the fall of Gods?". Journal of Affective Disorders. 182: 132–7. doi:10.1016/j.jad.2015.04.048. PMID 25985383.
- Dragioti E, Solmi M, Favaro A, Fusar-Poli P, Dazzan P, Thompson T, et al. (October 2019). "Association of Antidepressant Use With Adverse Health Outcomes: A Systematic Umbrella Review". JAMA Psychiatry. 76 (12): 1241–1255. doi:10.1001/jamapsychiatry.2019.2859. PMC 6777224. PMID 31577342.
- Baird G, Cass H, Slonims V (August 2003). "Diagnosis of autism". BMJ. 327 (7413): 488–493. doi:10.1136/bmj.327.7413.488. PMC 188387. PMID 12946972.
- "Section 2: Neurodevelopmental Disorders". Diagnostic and statistical manual of mental disorders : DSM-5-TR (Print) (Fifth edition, text revision. ed.). Washington, DC: American Psychiatric Association Publishing. 2022. ISBN 978-0-89042-575-6.
- CDC (31 March 2022). "Screening and Diagnosis | Autism Spectrum Disorder (ASD) | NCBDDD". Centers for Disease Control and Prevention. Retrieved 12 September 2022.
- Volkmar F, Cook EH, Pomeroy J, Realmuto G, Tanguay P (December 1999). "Practice parameters for the assessment and treatment of children, adolescents, and adults with autism and other pervasive developmental disorders. American Academy of Child and Adolescent Psychiatry Working Group on Quality Issues". Journal of the American Academy of Child and Adolescent Psychiatry. 38 (12 Suppl): 32S–54S. doi:10.1016/s0890-8567(99)80003-3. PMID 10624084.
- Dover CJ, Le Couteur A (June 2007). "How to diagnose autism". Archives of Disease in Childhood. 92 (6): 540–545. doi:10.1136/adc.2005.086280. PMC 2066173. PMID 17515625.
- Mantovani JF (May 2000). "Autistic regression and Landau-Kleffner syndrome: progress or confusion?". Developmental Medicine and Child Neurology. 42 (5): 349–353. doi:10.1017/S0012162200210621. PMID 10855658.
- Constantino JN, Charman T (March 2016). "Diagnosis of autism spectrum disorder: reconciling the syndrome, its diverse origins, and variation in expression" (PDF). The Lancet. Neurology. 15 (3): 279–91. doi:10.1016/s1474-4422(15)00151-9. PMID 26497771. S2CID 206162618.
- Matson JL, Neal D (2009). "Cormorbidity: diagnosing comorbid psychiatric conditions". Psychiatr Times. 26 (4). Archived from the original on 3 April 2013.
- Simms MD (February 2017). "When Autistic Behavior Suggests a Disease Other than Classic Autism". Pediatric Clinics of North America. 64 (1): 127–138. doi:10.1016/j.pcl.2016.08.009. PMID 27894440.
- Kanne SM, Randolph JK, Farmer JE (December 2008). "Diagnostic and assessment findings: a bridge to academic planning for children with autism spectrum disorders". Neuropsychology Review. 18 (4): 367–384. doi:10.1007/s11065-008-9072-z. PMID 18855144. S2CID 21108225.
- Caronna EB, Milunsky JM, Tager-Flusberg H (June 2008). "Autism spectrum disorders: clinical and research frontiers". Archives of Disease in Childhood. 93 (6): 518–523. doi:10.1136/adc.2006.115337. PMID 18305076. S2CID 18761374.
- Schaefer GB, Mendelsohn NJ (January 2008). "Genetics evaluation for the etiologic diagnosis of autism spectrum disorders". Genetics in Medicine. 10 (1): 4–12. doi:10.1097/GIM.0b013e31815efdd7. PMID 18197051. S2CID 4468548.
- Landa RJ (March 2008). "Diagnosis of autism spectrum disorders in the first 3 years of life". Nature Clinical Practice. Neurology. 4 (3): 138–147. doi:10.1038/ncpneuro0731. PMID 18253102.
- Mandell DS, Novak MM, Zubritsky CD (December 2005). "Factors associated with age of diagnosis among children with autism spectrum disorders". Pediatrics. 116 (6): 1480–1486. doi:10.1542/peds.2005-0185. PMC 2861294. PMID 16322174.
- Shattuck PT, Grosse SD (2007). "Issues related to the diagnosis and treatment of autism spectrum disorders". Developmental Disabilities Research Reviews. 13 (2): 129–135. doi:10.1002/mrdd.20143. PMID 17563895.
- Huang, Yunhe; Arnold, Samuel Rc; Foley, Kitty-Rose; Trollor, Julian N. (August 2020). "Diagnosis of autism in adulthood: A scoping review". Autism: The International Journal of Research and Practice. 24 (6): 1311–1327. doi:10.1177/1362361320903128. ISSN 1461-7005. PMID 32106698. S2CID 211556350.
- Lai, Meng-Chuan; Szatmari, Peter (2020). "Sex and gender impacts on the behavioural presentation and recognition of autism". Current Opinion in Psychiatry. 33 (2): 117–123. doi:10.1097/YCO.0000000000000575. ISSN 1473-6578. PMID 31815760. S2CID 209164138.
- Lockwood Estrin, Georgia; Milner, Victoria; Spain, Debbie; Happé, Francesca; Colvert, Emma (29 October 2020). "Barriers to Autism Spectrum Disorder Diagnosis for Young Women and Girls: a Systematic Review". Review Journal of Autism and Developmental Disorders. Springer Science and Business Media LLC. 8 (4): 454–470. doi:10.1007/s40489-020-00225-8. ISSN 2195-7177. PMC 8604819. PMID 34868805.
- Hull L, Petrides KV, Allison C, Smith P, Baron-Cohen S, Lai MC, Mandy W (August 2017). "'Putting on My Best Normal': Social Camouflaging in Adults with Autism Spectrum Conditions". Journal of Autism and Developmental Disorders. 47 (8): 2519–2534. doi:10.1007/s10803-017-3166-5. PMC 5509825. PMID 28527095.
- Filipek PA, Accardo PJ, Ashwal S, Baranek GT, Cook EH, Dawson G, et al. (August 2000). "Practice parameter: screening and diagnosis of autism: report of the Quality Standards Subcommittee of the American Academy of Neurology and the Child Neurology Society". Neurology. 55 (4): 468–79. doi:10.1212/wnl.55.4.468. PMID 10953176.
- Ozonoff S, Goodlin-Jones BL, Solomon M (September 2005). "Evidence-based assessment of autism spectrum disorders in children and adolescents" (PDF). Journal of Clinical Child and Adolescent Psychology. Taylor & Francis. 34 (3): 523–40. doi:10.1207/s15374424jccp3403_8. ISSN 1537-4416. PMID 16083393. S2CID 14322690. Archived from the original (PDF) on 18 April 2021. Retrieved 3 September 2019.
- Corsello C, Hus V, Pickles A, Risi S, Cook EH, Leventhal BL, Lord C (September 2007). "Between a ROC and a hard place: decision making and making decisions about using the SCQ". Journal of Child Psychology and Psychiatry, and Allied Disciplines. 48 (9): 932–40. doi:10.1111/j.1469-7610.2007.01762.x. eISSN 1469-7610. hdl:2027.42/74877. ISSN 0021-9630. OCLC 01307942. PMID 17714378.
- Huerta M, Lord C (February 2012). "Diagnostic evaluation of autism spectrum disorders". Pediatric Clinics of North America. 59 (1): 103–11, xi. doi:10.1016/j.pcl.2011.10.018. PMC 3269006. PMID 22284796.
- Kan CC, Buitelaar JK, van der Gaag RJ (June 2008). "Autismespectrumstoornissen bij volwassenen" [Autism spectrum disorders in adults]. Nederlands Tijdschrift voor Geneeskunde (in Dutch). 152 (24): 1365–1369. PMID 18664213.
- "Autism case training part 1: A closer look – key developmental milestones". CDC.gov. 18 August 2016. Retrieved 5 August 2019.
- Siu AL, Bibbins-Domingo K, Grossman DC, Baumann LC, Davidson KW, Ebell M, et al. (February 2016). "Screening for Autism Spectrum Disorder in Young Children: US Preventive Services Task Force Recommendation Statement". JAMA. 315 (7): 691–696. doi:10.1001/jama.2016.0018. PMID 26881372.
- Johnson, Chris Plauché; Myers, Scott M. (1 November 2007). "Identification and Evaluation of Children With Autism Spectrum Disorders". Pediatrics. American Academy of Pediatrics. 120 (5): 1183–1215. doi:10.1542/peds.2007-2361. ISSN 0031-4005. PMID 17967920. S2CID 218028., cited in Blumberg SJ, Zablotsky B, Avila RM, Colpe LJ, Pringle BA, Kogan MD (October 2016). "Diagnosis lost: Differences between children who had and who currently have an autism spectrum disorder diagnosis". Autism. 20 (7): 783–795. doi:10.1177/1362361315607724. PMC 4838550. PMID 26489772.
- For example:
- US Preventive Services Task Force does not recommend universal screen of young children for autism due to poor evidence of benefits of this screening when parents and clinicians have no concerns about ASD. The major concern is a false-positive diagnosis that would burden a family with very time-consuming and financially demanding treatment interventions when it is not truly required. The Task Force also did not find any robust studies showing effectiveness of behavioral therapies in reducing ASD symptom severity.[217]
- American Academy of Pediatrics recommends ASD screening of all children between the ages if 18 and 24 months.[217] The AAP also recommends that children who screen positive for ASD be referred to treatment services without waiting for a comprehensive diagnostic workup[218]
- The American Academy of Family Physicians did not find sufficient evidence of benefit of universal early screening for ASD[217]
- The American Academy of Neurology and Child Neurology Society recommends general routine screening for delayed or abnormal development in children followed by screening for ASD only if indicated by the general developmental screening[217]
- The American Academy of Child and Adolescent Psychiatry recommend routinely screening autism symptoms in young children[217]
- Wetherby AM, Brosnan-Maddox S, Peace V, Newton L (September 2008). "Validation of the Infant-Toddler Checklist as a broadband screener for autism spectrum disorders from 9 to 24 months of age". Autism. 12 (5): 487–511. doi:10.1177/1362361308094501. PMC 2663025. PMID 18805944.
- Wallis KE, Pinto-Martin J (May 2008). "The challenge of screening for autism spectrum disorder in a culturally diverse society". Acta Paediatrica. 97 (5): 539–540. doi:10.1111/j.1651-2227.2008.00720.x. PMID 18373717. S2CID 39744269.
- Lintas C, Persico AM (January 2009). "Autistic phenotypes and genetic testing: state-of-the-art for the clinical geneticist". Journal of Medical Genetics. 46 (1): 1–8. doi:10.1136/jmg.2008.060871. PMC 2603481. PMID 18728070.
- "Conditions That May Look Like Autism, but Aren't". WebMD. Retrieved 10 May 2020.
- Helverschou SB, Bakken TL, Martinsen H (2011). "Psychiatric Disorders in People with Autism Spectrum Disorders: Phenomenology and Recognition". In Matson JL, Sturmey P (eds.). International handbook of autism and pervasive developmental disorders. New York: Springer. pp. 53–74. ISBN 9781441980649. OCLC 746203105.
- Underwood L, McCarthy J, Tsakanikos E (September 2010). "Mental health of adults with autism spectrum disorders and intellectual disability". Current Opinion in Psychiatry. 23 (5): 421–6. doi:10.1097/YCO.0b013e32833cfc18. PMID 20613532. S2CID 13735841.
- Ballaban-Gil K, Tuchman R (2000). "Epilepsy and epileptiform EEG: association with autism and language disorders". Developmental Disabilities Research Reviews. 6 (4): 300–8. doi:10.1002/1098-2779(2000)6:4<300::AID-MRDD9>3.0.CO;2-R. PMID 11107195.
- Spence SJ, Schneider MT (June 2009). "The role of epilepsy and epileptiform EEGs in autism spectrum disorders". Pediatric Research. 65 (6): 599–606. doi:10.1203/PDR.0b013e31819e7168. PMC 2692092. PMID 19454962.
- Wiznitzer M (September 2004). "Autism and tuberous sclerosis". Journal of Child Neurology. 19 (9): 675–9. doi:10.1177/08830738040190090701. PMID 15563013. S2CID 38157900.
- Zafeiriou DI, Ververi A, Vargiami E (June 2007). "Childhood autism and associated comorbidities". Brain & Development. 29 (5): 257–272. doi:10.1016/j.braindev.2006.09.003. PMID 17084999. S2CID 16386209.
- Satterstrom FK, Kosmicki JA, Wang J, Breen MS, De Rubeis S, An JY, et al. (February 2020). "Large-Scale Exome Sequencing Study Implicates Both Developmental and Functional Changes in the Neurobiology of Autism". Cell. 180 (3): 568–584.e23. doi:10.1016/j.cell.2019.12.036. PMC 7250485. PMID 31981491.
- Holder, J. L. Jr.; Hamdan, F. F.; Michaud, J. L.; Adam, M. P.; Ardinger, H. H.; Pagon, R. A.; Wallace, S. E.; Bean LJH; Gripp, K. W.; Mirzaa, G. M.; Amemiya, A. (2019). "SYNGAP1-Related Intellectual Disability". Gene Reviews (Review). PMID 30789692.
- O'Brien G, Pearson J (June 2004). "Autism and learning disability". Autism. 8 (2): 125–40. doi:10.1177/1362361304042718. PMID 15165430. S2CID 17372893.
- White SW, Oswald D, Ollendick T, Scahill L (April 2009). "Anxiety in children and adolescents with autism spectrum disorders". Clinical Psychology Review. 29 (3): 216–229. doi:10.1016/j.cpr.2009.01.003. PMC 2692135. PMID 19223098.
- Lainhart J (1999). "Psychiatric problems in individuals with autism, their parents and siblings". International Review of Psychiatry. 11 (4): 278–298. doi:10.1080/09540269974177.
- Chisholm K, Lin A, Abu-Akel A, Wood SJ (August 2015). "The association between autism and schizophrenia spectrum disorders: A review of eight alternate models of co-occurrence" (PDF). Neuroscience and Biobehavioral Reviews. 55: 173–83. doi:10.1016/j.neubiorev.2015.04.012. PMID 25956249. S2CID 21450062.
- Hamlyn J, Duhig M, McGrath J, Scott J (May 2013). "Modifiable risk factors for schizophrenia and autism—shared risk factors impacting on brain development". Neurobiology of Disease. 53: 3–9. doi:10.1016/j.nbd.2012.10.023. PMID 23123588. S2CID 207067275.
- Crespi BJ, Thiselton DL (October 2011). "Comparative immunogenetics of autism and schizophrenia". Genes, Brain and Behavior. 10 (7): 689–701. doi:10.1111/j.1601-183X.2011.00710.x. PMID 21649858. S2CID 851655.
- Markkanen E, Meyer U, Dianov GL (June 2016). "DNA Damage and Repair in Schizophrenia and Autism: Implications for Cancer Comorbidity and Beyond". International Journal of Molecular Sciences. 17 (6): 856. doi:10.3390/ijms17060856. PMC 4926390. PMID 27258260.
- Tsakanikos E, Costello H, Holt G, Sturmey P, Bouras N (July 2007). "Behaviour management problems as predictors of psychotropic medication and use of psychiatric services in adults with autism" (PDF). Journal of Autism and Developmental Disorders. 37 (6): 1080–5. doi:10.1007/s10803-006-0248-1. PMID 17053989. S2CID 14272598.
- Rommelse NN, Franke B, Geurts HM, Hartman CA, Buitelaar JK (March 2010). "Shared heritability of attention-deficit/hyperactivity disorder and autism spectrum disorder". European Child & Adolescent Psychiatry. 19 (3): 281–95. doi:10.1007/s00787-010-0092-x. PMC 2839489. PMID 20148275.
- Baranek GT (October 2002). "Efficacy of sensory and motor interventions for children with autism". Journal of Autism and Developmental Disorders. 32 (5): 397–422. doi:10.1023/A:1020541906063. PMID 12463517. S2CID 16449130.
- Lugnegård T, Hallerbäck MU, Gillberg C (May 2012). "Personality disorders and autism spectrum disorders: what are the connections?". Comprehensive Psychiatry. 53 (4): 333–40. doi:10.1016/j.comppsych.2011.05.014. PMID 21821235.
- Tantam D (December 1988). "Lifelong eccentricity and social isolation. II: Asperger's syndrome or schizoid personality disorder?". The British Journal of Psychiatry. 153: 783–91. doi:10.1192/bjp.153.6.783. PMID 3256377. S2CID 39433805.
- Ekleberry SC (2008). "Cluster A - Schizoid Personality Disorder and Substance Use Disorders". Integrated Treatment for Co-Occurring Disorders: Personality Disorders and Addiction. Routledge. pp. 31–32. ISBN 978-0789036933.
- Folstein SE, Rosen-Sheidley B (December 2001). "Genetics of autism: complex aetiology for a heterogeneous disorder". Nature Reviews. Genetics. 2 (12): 943–955. doi:10.1038/35103559. PMID 11733747. S2CID 9331084.
- Manzi B, Loizzo AL, Giana G, Curatolo P (March 2008). "Autism and metabolic diseases". Journal of Child Neurology. 23 (3): 307–314. doi:10.1177/0883073807308698. PMID 18079313. S2CID 30809774.
- Richdale AL, Schreck KA (December 2009). "Sleep problems in autism spectrum disorders: prevalence, nature, & possible biopsychosocial aetiologies". Sleep Medicine Reviews. 13 (6): 403–411. doi:10.1016/j.smrv.2009.02.003. PMID 19398354.
- "Fake and harmful autism 'treatments'". nhs.uk. 2 May 2019. Retrieved 29 April 2022.
- "Making information and the words we use accessible". NHS England. Retrieved 29 April 2022.
- "How to talk about autism". www.autism.org.uk. Retrieved 29 April 2022.
- "The psychiatric management of autism in adults (CR228)". Royal College of Psychiatrists (UK). Retrieved 29 April 2022.
- McPartland J, Klin A (October 2006). "Asperger's syndrome". Adolescent Medicine Clinics. 17 (3): 771–88, abstract xiii. doi:10.1016/j.admecli.2006.06.010 (inactive 31 July 2022). PMID 17030291.
{{cite journal}}: CS1 maint: DOI inactive as of July 2022 (link) - Woodbury-Smith MR, Volkmar FR (June 2008). "Asperger syndrome". European Child & Adolescent Psychiatry. 18 (1): 2–11. doi:10.1007/s00787-008-0701-0. PMID 18563474. S2CID 12808995.
- Coplan J, Jawad AF (July 2005). "Modeling clinical outcome of children with autistic spectrum disorders". Pediatrics. 116 (1): 117–22. doi:10.1542/peds.2004-1118. PMID 15995041. S2CID 8440775.
- "10 Facts about Autism Spectrum Disorder (ASD)". Early Childhood Development | ACF. Retrieved 6 November 2019.
- Myers SM, Johnson CP (November 2007). "Management of children with autism spectrum disorders". Pediatrics. 120 (5): 1162–1182. doi:10.1542/peds.2007-2362. PMID 17967921.
- Ospina MB, Krebs Seida J, Clark B, Karkhaneh M, Hartling L, Tjosvold L, et al. (2008). "Behavioural and developmental interventions for autism spectrum disorder: a clinical systematic review". PLOS ONE. 3 (11): e3755. Bibcode:2008PLoSO...3.3755O. doi:10.1371/journal.pone.0003755. PMC 2582449. PMID 19015734.
- Smith T, Iadarola S (2 November 2015). "Evidence Base Update for Autism Spectrum Disorder". Journal of Clinical Child and Adolescent Psychology. Taylor & Francis. 44 (6): 897–922. doi:10.1080/15374416.2015.1077448. ISSN 1537-4416. PMID 26430947.
- Eldevik S, Hastings RP, Hughes JC, Jahr E, Eikeseth S, Cross S (May 2009). "Meta-analysis of Early Intensive Behavioral Intervention for children with autism". Journal of Clinical Child and Adolescent Psychology. Taylor & Francis. 38 (3): 439–50. CiteSeerX 10.1.1.607.9620. doi:10.1080/15374410902851739. ISSN 1537-4416. PMID 19437303. S2CID 205873629.
- Smith T, Iadarola S (2015). "Evidence Base Update for Autism Spectrum Disorder". Journal of Clinical Child and Adolescent Psychology. Taylor & Francis. 44 (6): 897–922. doi:10.1080/15374416.2015.1077448. ISSN 1537-4416. PMID 26430947.
- Matson, Johnny L.; Dempsey, Timothy; Fodstad, Jill C. (November 2009). "The effect of Autism Spectrum Disorders on adaptive independent living skills in adults with severe intellectual disability". Research in Developmental Disabilities. Elsevier. 30 (6): 1203–1211. doi:10.1016/j.ridd.2009.04.001. eISSN 1873-3379. ISSN 0891-4222. PMID 19450950.
- "NIMH » Autism Spectrum Disorder". National Institute of Mental Health (US). National Institutes of Health (US). Retrieved 8 April 2021.
- Ji N, Findling RL (March 2015). "An update on pharmacotherapy for autism spectrum disorder in children and adolescents". Current Opinion in Psychiatry. 28 (2): 91–101. doi:10.1097/YCO.0000000000000132. PMID 25602248. S2CID 206141453.
- Myers SM, Johnson CP (November 2007). "Management of children with autism spectrum disorders". Pediatrics. 120 (5): 1162–82. doi:10.1542/peds.2007-2362. PMID 17967921. S2CID 1656920. Archived from the original on 12 June 2009.
- Sigman M, Capps L (2002). Children with Autism: A Developmental Perspective. Cambridge: Harvard University Press. pp. 178–179. ISBN 978-0-674-05313-7.
- Rogers SJ, Vismara LA (January 2008). "Evidence-based comprehensive treatments for early autism". Journal of Clinical Child and Adolescent Psychology. Taylor & Francis. 37 (1): 8–38. doi:10.1080/15374410701817808. ISSN 1537-4416. PMC 2943764. PMID 18444052.
- Journal of Clinical Child and Adolescent Psychology, Taylor & Francis, ISSN 1537-4416, Wikidata Q15767686
- Zwaigenbaum L, Bauman ML, Choueiri R, Kasari C, Carter A, Granpeesheh D, et al. (October 2015). "Early Intervention for Children With Autism Spectrum Disorder Under 3 Years of Age: Recommendations for Practice and Research". Pediatrics. 136 (Supplement 1): S60-81. doi:10.1542/peds.2014-3667E. PMID 26430170.
- Reichow B, Hume K, Barton EE, Boyd BA (May 2018). "Early intensive behavioral intervention (EIBI) for young children with autism spectrum disorders (ASD)". The Cochrane Database of Systematic Reviews. 5 (10): CD009260. doi:10.1002/14651858.CD009260.pub3. PMC 6494600. PMID 29742275.
- Siewertsen CM, French ED, Teramoto M (2015). "Autism spectrum disorder and pet therapy". Advances in Mind-Body Medicine. 29 (2): 22–25. PMID 25831431.
- Weissman L (March 2020). "Autism spectrum disorder in children and adolescents: Pharmacologic interventions". Retrieved 17 March 2020.
- Williams Buckley A, Hirtz D, Oskoui M, et al. (March 2020). "Practice guideline: Treatment for insomnia and disrupted sleep behavior in children and adolescents with autism spectrum disorder: Report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology". Neurology. 94 (9): 392–404. doi:10.1212/WNL.0000000000009033. PMC 7238942. PMID 32051244.
- Harrop C (August 2015). "Evidence-based, parent-mediated interventions for young children with autism spectrum disorder: The case of restricted and repetitive behaviors". Autism. 19 (6): 662–72. doi:10.1177/1362361314545685. PMID 25186943. S2CID 32326472.
- Powell K (August 2004). "Opening a window to the autistic brain". PLOS Biology. 2 (8): E267. doi:10.1371/journal.pbio.0020267. PMC 509312. PMID 15314667.
- Simpson RL, de Boer-Ott SR, Smith-Myles B (2003). "Inclusion of Learners with Autism Spectrum Disorders in General Education Settings". Topics in Language Disorders. 23 (2): 116–133. doi:10.1097/00011363-200304000-00005. S2CID 143733343. Archived from the original on 14 July 2011.
- Sanchack KE, Thomas CA (December 2016). "Autism Spectrum Disorder: Primary Care Principles". American Family Physician. 94 (12): 972–979. PMID 28075089.
- Siafis S, Çıray O, Wu H, Schneider-Thoma J, Bighelli I, Krause M, Rodolico A, Ceraso A, Deste G, Huhn M, Fraguas D, San José Cáceres A, Mavridis D, Charman T, Murphy DG, Parellada M, Arango C, Leucht S (2022). "Pharmacological and dietary-supplement treatments for autism spectrum disorder: a systematic review and network meta-analysis". Molecular Autism. 13 (1): 10. doi:10.1186/s13229-022-00488-4. PMC 8896153. PMID 35246237.
- Oswald DP, Sonenklar NA (June 2007). "Medication use among children with autism spectrum disorders". Journal of Child and Adolescent Psychopharmacology. 17 (3): 348–355. doi:10.1089/cap.2006.17303. PMID 17630868.
- Doyle CA, McDougle CJ (September 2012). "Pharmacologic treatments for the behavioral symptoms associated with autism spectrum disorders across the lifespan". Dialogues in Clinical Neuroscience. 14 (3): 263–279. doi:10.31887/DCNS.2012.14.3/cdoyle. PMC 3513681. PMID 23226952.
- Leskovec TJ, Rowles BM, Findling RL (2008). "Pharmacological treatment options for autism spectrum disorders in children and adolescents". Harvard Review of Psychiatry. 16 (2): 97–112. doi:10.1080/10673220802075852. PMID 18415882. S2CID 26112061.
- Ameis SH, Kassee C, Corbett-Dick P, Cole L, Dadhwal S, Lai MC, et al. (November 2018). "Systematic review and guide to management of core and psychiatric symptoms in youth with autism". Acta Psychiatrica Scandinavica. 138 (5): 379–400. doi:10.1111/acps.12918. PMID 29904907. S2CID 49209337.
- Benevides TW, Shore SM, Andresen ML, Caplan R, Cook B, Gassner DL, et al. (August 2020). "Interventions to address health outcomes among autistic adults: A systematic review". Autism. 24 (6): 1345–1359. doi:10.1177/1362361320913664. PMC 7787674. PMID 32390461.
- Gogou M, Kolios G (June 2018). "Are therapeutic diets an emerging additional choice in autism spectrum disorder management?". World Journal of Pediatrics (Review). 14 (3): 215–223. doi:10.1007/s12519-018-0164-4. PMID 29846886. S2CID 44155118.
Current literature knowledge provides evidence that ketogenic and casein/gluten-free diet may have their own place in our reserve for the therapeutic management of specific subsets of children with autism. ... More clinical studies about the effect of gluten/caseinfree diet in these patients are available. However, available data arise from studies with small sample size and are still controversial. In general, despite encouraging data, no definite proof still exists. Under this view, the use of therapeutic diets in children with autism should be restricted to specific subgroups, such as children with autism and epilepsy or specific inborn errors of metabolism (ketogenic diet), children with known food intolerance/allergy or even children with food intolerance markers (gluten- and casein-free diet). Their implementation should always be guided by health care practitioners.
- Marí-Bauset S, Zazpe I, Mari-Sanchis A, Llopis-González A, Morales-Suárez-Varela M (December 2014). "Evidence of the gluten-free and casein-free diet in autism spectrum disorders: a systematic review". Journal of Child Neurology. 29 (12): 1718–1727. doi:10.1177/0883073814531330. hdl:10171/37087. PMID 24789114. S2CID 19874518.
- Millward C, Ferriter M, Calver S, Connell-Jones G (April 2008). Ferriter M (ed.). "Gluten- and casein-free diets for autistic spectrum disorder". The Cochrane Database of Systematic Reviews (2): CD003498. doi:10.1002/14651858.CD003498.pub3. PMC 4164915. PMID 18425890.
Knivsberg 2002 "monitoring of the compliance with diet was not carried out" ... "several reports of children 'sneaking food' from siblings or classmates"
- Hyman SL, Stewart PA, Foley J, Cain U, Peck R, Morris DD, et al. (January 2016). "The Gluten-Free/Casein-Free Diet: A Double-Blind Challenge Trial in Children with Autism". Journal of Autism and Developmental Disorders. 46 (1): 205–220. doi:10.1007/s10803-015-2564-9. PMID 26343026. S2CID 12884691.
20 natural challenges when parents reported that children by mistake consumed foods containing gluten or casein.
- Siafis S, Çıray O, Schneider-Thoma J, Bighelli I, Krause M, Rodolico A, Ceraso A, Deste G, Huhn M, Fraguas D, Mavridis D, Charman T, Murphy DG, Parellada M, Arango C, Leucht S (2020). "Placebo response in pharmacological and dietary supplement trials of autism spectrum disorder (ASD): systematic review and meta-regression analysis". Molecular Autism. 11 (1): 66. doi:10.1186/s13229-020-00372-z. PMC 7448339. PMID 32847616.
- Buie T (May 2013). "The relationship of autism and gluten". Clinical Therapeutics (Review). 35 (5): 578–583. doi:10.1016/j.clinthera.2013.04.011. PMID 23688532.
At this time, the studies attempting to treat symptoms of autism with diet have not been sufficient to support the general institution of a gluten-free or other diet for all children with autism. There may be a subgroup of patients who might benefit from a gluten-free diet, but the symptom or testing profile of these candidates remains unclear.
- Volta U, Caio G, De Giorgio R, Henriksen C, Skodje G, Lundin KE (June 2015). "Non-celiac gluten sensitivity: a work-in-progress entity in the spectrum of wheat-related disorders". Best Practice & Research. Clinical Gastroenterology. 29 (3): 477–491. doi:10.1016/j.bpg.2015.04.006. PMID 26060112.
autism spectrum disorders (ASD) have been hypothesized to be associated with NCGS [47,48]. Notably, a gluten- and casein-free diet might have a positive effect in improving hyperactivity and mental confusion in some patients with ASD. This very exciting association between NCGS and ASD deserves further study before conclusions can be firmly drawn
- San Mauro Martín I, Garicano Vilar E, Collado Yurrutia L, Ciudad Cabañas MJ (December 2014). "[Is gluten the great etiopathogenic agent of disease in the XXI century?]" [Is gluten the great etiopathogenic agent of disease in the XXI century?]. Nutricion Hospitalaria (in Spanish). 30 (6): 1203–1210. doi:10.3305/nh.2014.30.6.7866. PMID 25433099.
- Tye C, Runicles AK, Whitehouse AJ, Alvares GA (2019). "Characterizing the Interplay Between Autism Spectrum Disorder and Comorbid Medical Conditions: An Integrative Review". Frontiers in Psychiatry (Review). 9: 751. doi:10.3389/fpsyt.2018.00751. PMC 6354568. PMID 30733689.
- Levy SE, Hyman SL (October 2008). "Complementary and alternative medicine treatments for children with autism spectrum disorders". Child and Adolescent Psychiatric Clinics of North America (Review). 17 (4): 803–20, ix. doi:10.1016/j.chc.2008.06.004. PMC 2597185. PMID 18775371.
- Brown MJ, Willis T, Omalu B, Leiker R (August 2006). "Deaths resulting from hypocalcemia after administration of edetate disodium: 2003-2005". Pediatrics. 118 (2): e534–e536. doi:10.1542/peds.2006-0858. PMID 16882789. S2CID 28656831. Archived from the original on 27 July 2009.
- James S, Stevenson SW, Silove N, Williams K (May 2015). James S (ed.). "Chelation for autism spectrum disorder (ASD)". The Cochrane Database of Systematic Reviews (Review) (5): CD010766. doi:10.1002/14651858.CD010766. PMID 26106752.
- Loftus, Yolande (24 November 2021). "CEASE Therapy for Autism: the Controversy of a "Cure"". Autism Parenting Magazine. Autism Parenting Magazine. Archived from the original on 22 September 2022. Retrieved 22 September 2022.
- Benevides TW, Shore SM, Andresen ML, Caplan R, Cook B, Gassner DL, et al. (August 2020). "Interventions to address health outcomes among autistic adults: A systematic review". Autism. 24 (6): 1345–1359. doi:10.1177/1362361320913664. PMC 7787674. PMID 32390461. S2CID 218586379.
- Geretsegger, Monika; Fusar-Poli, Laura; Elefant, Cochavit; Mössler, Karin A.; Vitale, Giovanni; Gold, Christian (9 May 2022). "Music therapy for autistic people". The Cochrane Database of Systematic Reviews. 2022 (5): CD004381. doi:10.1002/14651858.CD004381.pub4. ISSN 1469-493X. PMC 9082683. PMID 35532041.
- Warren Z, Veenstra-VanderWeele J, Stone W, et al. (April 2011). Therapies for Children With Autism Spectrum Disorders (Report No. 11-EHC029-EF). Agency for Healthcare Research and Quality (US). p. 8. PMID 21834171.
Hyperbaric therapy, in which oxygen is administered in special chambers that maintain a higher air pressure, has shown possible effects in other chronic neurologic conditions and has also undergone preliminary exploration in ASDs.
- Rumayor CB, Thrasher AM (November 2017). "Reflections on Recent Research Into Animal-Assisted Interventions in the Military and Beyond". Current Psychiatry Reports. 19 (12): 110. doi:10.1007/s11920-017-0861-z. PMID 29177710. S2CID 207338873.
- Duchan E, Patel DR (February 2012). "Epidemiology of autism spectrum disorders". Pediatric Clinics of North America. 59 (1): 27–43, ix–x. doi:10.1016/j.pcl.2011.10.003. PMID 22284791.
- Lambert N, Strebel P, Orenstein W, Icenogle J, Poland GA (June 2015). "Rubella". Lancet. 385 (9984): 2297–2307. doi:10.1016/S0140-6736(14)60539-0. PMC 4514442. PMID 25576992.
- Helt M, Kelley E, Kinsbourne M, Pandey J, Boorstein H, Herbert M, Fein D (December 2008). "Can children with autism recover? If so, how?". Neuropsychology Review. 18 (4): 339–366. CiteSeerX 10.1.1.695.2995. doi:10.1007/s11065-008-9075-9. PMID 19009353. S2CID 4317267.
- Rogers SJ, Vismara LA (January 2008). "Evidence-based comprehensive treatments for early autism". Journal of Clinical Child and Adolescent Psychology. Taylor & Francis. 37 (1): 8–38. doi:10.1080/15374410701817808. ISSN 1537-4416. PMC 2943764. PMID 18444052.
- Tidmarsh L, Volkmar FR (September 2003). "Diagnosis and epidemiology of autism spectrum disorders". Canadian Journal of Psychiatry. 48 (8): 517–525. doi:10.1177/070674370304800803. PMID 14574827. S2CID 38070709.
- Hendricks DR, Wehman P (24 March 2009). "Transition From School to Adulthood for Youth With Autism Spectrum Disorders: Review and Recommendations". Focus on Autism and Other Developmental Disabilities. 24 (2): 77–88. doi:10.1177/1088357608329827. S2CID 14636906.
- Roux AM, Rast JE, Rava JA, Anderson KA, Shattuck PT (31 August 2015). "Employment Outcomes of Young Adults on the Autism Spectrum". Life Course Outcomes Research Program, A.J. Drexel Autism Institute. Philadelphia, PA: Drexel University.
- Steinhausen HC, Mohr Jensen C, Lauritsen MB (June 2016). "A systematic review and meta-analysis of the long-term overall outcome of autism spectrum disorders in adolescence and adulthood". Acta Psychiatrica Scandinavica. 133 (6): 445–452. doi:10.1111/acps.12559. PMID 26763353. S2CID 12341774.
- Stichter JP, Riley-Tillman TC, Jimerson SR (December 2016). "Assessing, understanding, and supporting students with autism at school: Contemporary science, practice, and policy". School Psychology Quarterly. 31 (4): 443–449. doi:10.1037/spq0000184. PMID 27929316.
- Hahler, Eva-Maria; Elsabbagh, Mayada (1 March 2015). "Autism: A Global Perspective". Current Developmental Disorders Reports. 2 (1): 58–64. doi:10.1007/s40474-014-0033-3. ISSN 2196-2987. S2CID 73214418.
- McLeod, Saul (6 April 2022). "Jean Piaget's Theory of Cognitive Development". Simply Psychology. Archived from the original on 1 June 2022. Retrieved 19 February 2019.
- "Facts and Statistics". Autism Society. Archived from the original on 30 October 2019. Retrieved 6 November 2019.
- Ohl A, Grice Sheff M, Small S, Nguyen J, Paskor K, Zanjirian A (2017). "Predictors of employment status among adults with Autism Spectrum Disorder". Work. 56 (2): 345–355. doi:10.3233/WOR-172492. PMID 28211841.
- Ganz ML (April 2007). "The lifetime distribution of the incremental societal costs of autism". Archives of Pediatrics & Adolescent Medicine. 161 (4): 343–349. doi:10.1001/archpedi.161.4.343. PMID 17404130.
- Praslova, Ludmila N. (2021). Autism Doesn’t Hold People Back at Work. Discrimination Does. Harvard Business Review, 13 December 2021.
- Praslova, Ludmila N. (2022). Your “Autism Awareness Day” Might Be Excluding Autistic People. Harvard Business Review, 1 April 2022
- Johnson KR, Ennis-Cole D, Bohamgregory M (21 February 2020). "Workplace Success Strategies for Employees With Autism Spectrum Disorder: A New Frontier for Human Resource Development". Human Resource Development Review. 19 (2): 122–151. doi:10.1177/1534484320905910. S2CID 213995367.
- Bernick M (12 January 2021). "The State Of Autism Employment In 2021". Forbes. Retrieved 11 February 2022.
- Praslova, Ludmila N. (2022). An Intersectional Approach to Inclusion at Work. Harvard Business Review, 21 June 2022
- Praslova, Ludmila N. (2022). To build a healthy workplace, you need a toxic culture alarm Fast Company, 14 March 2022.
- "Autism". World Health Organization. 30 March 2022. Retrieved 8 May 2022.
- Russell G, Stapley S, Newlove-Delgado T, Salmon A, White R, Warren F, et al. (August 2021). "Time trends in autism diagnosis over 20 years: a UK population-based cohort study". Journal of Child Psychology and Psychiatry, and Allied Disciplines. 63 (6): 674–682. doi:10.1111/jcpp.13505. eISSN 1469-7610. ISSN 0021-9630. OCLC 01307942. PMID 34414570. S2CID 237242123.
The figure starkly illustrates an overall 787% increase in recorded incidence of autism diagnosis over 20 years.
- Maenner MJ, Shaw KA, Baio J, Washington A, Patrick M, DiRienzo M, et al. (March 2020). "Prevalence of Autism Spectrum Disorder Among Children Aged 8 Years - Autism and Developmental Disabilities Monitoring Network, 11 Sites, United States, 2016". Morbidity and Mortality Weekly Report. Surveillance Summaries. 69 (4): 1–12. doi:10.15585/mmwr.ss6904a1. PMC 7119644. PMID 32214087.
- ICD-11, "Females diagnosed with autism spectrum disorder are more frequently diagnosed with co-occurring disorders of intellectual development, suggesting that less severe presentations may go undetected as compared to males".
- Tsakanikos E, Underwood L, Kravariti E, Bouras N, McCarthy J (2011). "Gender differences in co-morbid psychopathology and clinical management in adults with autism spectrum disorders". Research in Autism Spectrum Disorders. 5 (2): 803–808. doi:10.1016/j.rasd.2010.09.009. ISSN 1750-9467.
- Hollander E, Hagerman RJ, Fein D (30 April 2018). Autism spectrum disorders (First ed.). Washington, DC: American Psychiatric Association Publishing. ISBN 978-1-61537-192-1. OCLC 1022084798.
- Baio J, Wiggins L, Christensen DL, et al. (April 2018). "Prevalence of Autism Spectrum Disorder Among Children Aged 8 Years – Autism and Developmental Disabilities Monitoring Network, 11 Sites, United States, 2014". Morbidity and Mortality Weekly Report. Surveillance Summaries. 67 (6): 1–23. doi:10.15585/mmwr.ss6706a1. PMC 5919599. PMID 29701730.
- Rødgaard EM, Jensen K, Vergnes JN, Soulières I, Mottron L (August 2019). "Temporal Changes in Effect Sizes of Studies Comparing Individuals With and Without Autism: A Meta-analysis". JAMA Psychiatry. 76 (11): 1124–1132. doi:10.1001/jamapsychiatry.2019.1956. PMC 6704749. PMID 31433441.
- "CDC estimates 1 in 68 school-aged children have autism; no change from previous estimate". CDC Newsroom. CDC. 31 March 2016. Retrieved 31 December 2019.
- Hill AP (2014). "Epidemiology of autism spectrum disorders". In Volkmar FR (ed.). Handbook of Autism and Pervasive Developmental Disorders. Diagnosis, Development, and Brain Mechanisms. Vol. 1. New York: Wiley. pp. 57–96. doi:10.1002/9781118911389. ISBN 9781118911389.
- Brugha T, Cooper SA, McManus S, Purdon S, Smith J, Scott FJ, et al. (31 January 2012). "Estimating the prevalence of autism spectrum conditions in adults: extending the 2007 Adult Psychiatric Morbidity Survey" (PDF). The Information Centre for Health and Social Care. National Health Service, UK. Archived from the original (PDF) on 30 December 2014. Retrieved 29 December 2014.
- Mozes A (26 November 2018). "Report: Autism Rate Rises to 1 in 40 Children". WebMD. Retrieved 26 September 2019.
- "Autism". www.who.int. Retrieved 15 September 2022.
- Fombonne E (June 2009). "Epidemiology of pervasive developmental disorders". Pediatric Research. 65 (6): 591–598. doi:10.1203/PDR.0b013e31819e7203. PMID 19218885.
- Wing L, Potter D (2002). "The epidemiology of autistic spectrum disorders: is the prevalence rising?". Developmental Disabilities Research Reviews. 8 (3): 151–161. doi:10.1002/mrdd.10029. PMID 12216059.
- Gernsbacher MA, Dawson M, Goldsmith HH (April 2005). "Three Reasons Not to Believe in an Autism Epidemic". Current Directions in Psychological Science. 14 (2): 55–58. doi:10.1111/j.0963-7214.2005.00334.x. PMC 4232964. PMID 25404790.
- Rutter M (January 2005). "Incidence of autism spectrum disorders: changes over time and their meaning". Acta Paediatrica. 94 (1): 2–15. doi:10.1111/j.1651-2227.2005.tb01779.x. PMID 15858952. S2CID 79259285.
- Szpir M (July 2006). "Tracing the origins of autism: a spectrum of new studies". Environmental Health Perspectives. 114 (7): A412–A418. doi:10.1289/ehp.114-a412. PMC 1513312. PMID 16835042.
- Chaste P, Leboyer M (September 2012). "Autism risk factors: genes, environment, and gene-environment interactions". Dialogues in Clinical Neuroscience. 14 (3): 281–292. doi:10.31887/DCNS.2012.14.3/pchaste. PMC 3513682. PMID 23226953.
- Schaafsma SM, Pfaff DW (August 2014). "Etiologies underlying sex differences in Autism Spectrum Disorders". Frontiers in Neuroendocrinology. 35 (3): 255–71. doi:10.1016/j.yfrne.2014.03.006. PMID 24705124. S2CID 7636860.
- Bertoglio K, Hendren RL (March 2009). "New developments in autism". The Psychiatric Clinics of North America. 32 (1): 1–14. doi:10.1016/j.psc.2008.10.004. PMID 19248913.
- "HRSA-led study estimates 1 in 40 U.S. children has diagnosed autism". HRSA News Room. U.S. Department of Health & Human Services, Health Resources and Services Administration. 19 November 2018. Retrieved 17 October 2019.
- National Center on Birth Defects and Developmental Disabilities (31 March 2022). "Autism and Developmental Disabilities Monitoring (ADDM) Network". Centers for Disease Control and Prevention. Retrieved 4 April 2022.
- Wolff S (August 2004). "The history of autism". European Child & Adolescent Psychiatry. 13 (4): 201–208. doi:10.1007/s00787-004-0363-5. PMID 15365889. S2CID 6106042.
- Wing L (1997). "The history of ideas on autism: legends, myths and reality". Autism. 1 (1): 13–23. doi:10.1177/1362361397011004. S2CID 145210370.
- Houston RA, Frith U (2000). Autism in History: The Case of Hugh Blair of Borgue. Oxford: John Wiley & Sons. ISBN 978-0-631-22089-3. LCCN 00036033. OCLC 231866075.
- Kuhn R (September 2004). "Eugen Bleuler's concepts of psychopathology". History of Psychiatry. 15 (59 Pt 3): 361–366. doi:10.1177/0957154X04044603. PMID 15386868. S2CID 5317716. The quote is a translation of Bleuler's 1910 original.
- Manouilenko I, Bejerot S (August 2015). "Sukhareva--Prior to Asperger and Kanner". Nordic Journal of Psychiatry (Report) (published 31 March 2015). 69 (6): 479–482. doi:10.3109/08039488.2015.1005022. PMID 25826582. S2CID 207473133.
- Asperger H (1938). "Das psychisch abnormale Kind" [The psychically abnormal child]. Wien Klin Wochenschr (in German). 51: 1314–1317.
- Kanner L (1943). "Autistic disturbances of affective contact". Acta Paedopsychiatrica. 35 (4): 100–136. PMID 4880460. Reprinted in Kanner L (1968). "Autistic disturbances of affective contact". Acta Paedopsychiatrica. 35 (4): 100–136. PMID 4880460.
- Lyons V, Fitzgerald M (November 2007). "Asperger (1906-1980) and Kanner (1894-1981), the two pioneers of autism". Journal of Autism and Developmental Disorders. 37 (10): 2022–2023. doi:10.1007/s10803-007-0383-3. PMID 17922179. S2CID 38130758.
- Fombonne E (September 2003). "Modern views of autism". Canadian Journal of Psychiatry. 48 (8): 503–505. doi:10.1177/070674370304800801. PMID 14574825. S2CID 8868418.
- Harris J (February 2018). "Leo Kanner and autism: a 75-year perspective". International Review of Psychiatry. 30 (1): 3–17. doi:10.1080/09540261.2018.1455646. PMID 29667863. S2CID 4978549.
- Kanner L (July 1949). "Problems of nosology and psychodynamics of early infantile autism". The American Journal of Orthopsychiatry. 19 (3): 416–26. doi:10.1111/j.1939-0025.1949.tb05441.x. PMID 18146742.
- "Early Infantile Autism and the Refrigerator Mother Theory (1943-1970) | The Embryo Project Encyclopedia". embryo.asu.edu. Retrieved 6 October 2022.
- Tager-Flusberg H (February 2016). "Risk Factors Associated With Language in Autism Spectrum Disorder: Clues to Underlying Mechanisms". Journal of Speech, Language, and Hearing Research. 59 (1): 143–54. doi:10.1044/2015_jslhr-l-15-0146. PMC 4867927. PMID 26502110.
- Szatmari P, Jones MB (2007). "Genetic epidemiology of autism spectrum disorders". In Volkmar FR (ed.). Autism and Pervasive Developmental Disorders (2nd ed.). Cambridge University Press. pp. 157–178. ISBN 978-0-521-54957-8.
- Chambres P, Auxiette C, Vansingle C, Gil S (August 2008). "Adult attitudes toward behaviors of a six-year-old boy with autism". Journal of Autism and Developmental Disorders. 38 (7): 1320–1327. doi:10.1007/s10803-007-0519-5. PMID 18297387. S2CID 19769173.
- Heidgerken AD, Geffken G, Modi A, Frakey L (June 2005). "A survey of autism knowledge in a health care setting". Journal of Autism and Developmental Disorders. 35 (3): 323–330. doi:10.1007/s10803-005-3298-x. PMID 16119473. S2CID 2015723.
- Baker JP (September 2013). "Autism at 70--redrawing the boundaries" (PDF). The New England Journal of Medicine. 369 (12): 1089–1091. doi:10.1056/NEJMp1306380. PMID 24047057. S2CID 44613078. Archived from the original (PDF) on 3 March 2019.
- Biever C (2007). "Web removes social barriers for those with autism". New Scientist. Reed Elsevier (2610): 26–27. ISSN 0262-4079. Archived from the original on 20 October 2012.
- Silverman C (2008). "Fieldwork on another planet: social science perspectives on the autism spectrum". BioSocieties. 3 (3): 325–341. doi:10.1017/S1745855208006236. S2CID 145379758.
- Harmon A (20 December 2004). "How about not 'curing' us, some autistics are pleading". The New York Times. Archived from the original on 11 May 2013.
- Shapiro J (26 June 2006). "Autism Movement Seeks Acceptance, Not Cures". NPR. Retrieved 10 November 2015.
- Trivedi B. "Autistic and proud of it". New Scientist. Reed Elsevier. ISSN 0262-4079. Retrieved 10 November 2015.
- Solomon, Andrew (25 May 2008). "The autism rights movement". New York. ISSN 0028-7369. Archived from the original on 27 May 2008. Retrieved 27 May 2008.
- The Economic World. New York city: Chronicle Publishing Company. 1917. p. 366.
- "Results and Analysis of the Autistic Not Weird 2022 Autism Survey - Autistic Not Weird". 23 March 2022. Retrieved 29 April 2022.
- "World Autism Awareness Day, 2 April". United Nations. Retrieved 17 November 2015.
- Bascom J (18 June 2015). "Autistic Pride Day 2015: A Message to the Autistic Community". Retrieved 18 November 2015.
- "Autism Sunday – Home". Autism Sunday. 2010. Archived from the original on 3 March 2010. Retrieved 17 November 2015.
- "About Autreat". Autreat.com. 2013. Retrieved 17 November 2015.
- Silverman C (2008). "Fieldwork on Another Planet: Social Science Perspectives on the Autism Spectrum". BioSocieties. 3 (3): 325–341. doi:10.1017/S1745855208006236. ISSN 1745-8552. S2CID 145379758.
- Russell G, Kapp SK, Elliott D, Elphick C, Gwernan-Jones R, Owens C (13 April 2019). "Mapping the Autistic Advantage from the Accounts of Adults Diagnosed with Autism: A Qualitative Study". Autism in Adulthood. 1 (2): 124–133. doi:10.1089/aut.2018.0035. PMC 6493410. PMID 31058260. S2CID 142504027.
- Clarke J, van Amerom G (2007). "'Surplus suffering': differences between organizational understandings of Asperger's syndrome and those people who claim the 'disorder'". Disability & Society. 22 (7): 761–76. doi:10.1080/09687590701659618. S2CID 145736625.
- Baron-Cohen S (2002). "Is Asperger syndrome necessarily viewed as a disability?". Focus Autism Other Dev Disabl. 17 (3): 186–91. doi:10.1177/10883576020170030801. S2CID 145629311. A preliminary, freely readable draft, with slightly different wording in the quoted text, is in: Baron-Cohen S (2002). "Is Asperger's syndrome necessarily a disability?" (PDF). Cambridge: Autism Research Centre. Archived from the original (PDF) on 17 December 2008. Retrieved 2 December 2008.
- Pellicano, Elizabeth; den Houting, Jacquiline (2021). "Annual Research Review: Shifting from 'normal science' to neurodiversity in autism science". Journal of Child Psychology and Psychiatry, and Allied Disciplines. 63 (4): 381–396. doi:10.1111/jcpp.13534. ISSN 1469-7610. PMC 9298391. PMID 34730840. S2CID 241118562.
- "The Autism Rights Movement". nymag.com. Retrieved 26 October 2021.
- Morgan, Jules (1 October 2016). "Autism spectrum disorder: difference or disability?". The Lancet Neurology. 15 (11): 1126. doi:10.1016/S1474-4422(16)30002-3. ISSN 1474-4422. S2CID 54341655.
- Silverman, Chloe (1 September 2008). "Fieldwork on Another Planet: Social Science Perspectives on the Autism Spectrum". BioSocieties. 3 (3): 325–341. doi:10.1017/S1745855208006236. ISSN 1745-8560. S2CID 145379758.
- "A medical condition or just a difference? The question roils autism community". Washington Post. ISSN 0190-8286. Retrieved 15 October 2021.
- Ratner P (10 July 2016). "Should Autism Be Cured or Is "Curing" Offensive?". Big Think. Retrieved 16 June 2019.
- Jaarsma P, Welin S (March 2012). "Autism as a natural human variation: reflections on the claims of the neurodiversity movement". Health Care Analysis. 20 (1): 20–30. doi:10.1007/s10728-011-0169-9. PMID 21311979. S2CID 18618887.
- McGee M (August 2012). "Neurodiversity". Contexts. 11 (3): 12–13. doi:10.1177/1536504212456175. S2CID 220720495.
- Sarrett J (April 2016). "Biocertification and Neurodiversity the Role and Implications of Self-Diagnosis in Autistic Communities". www.researchgate.net. Retrieved 6 March 2022.
- Aguiar MC, de Pondé MP (March 2019). "Parenting a child with autism". Jornal Brasileiro de Psiquiatria. 68 (1): 42–47. doi:10.1590/0047-2085000000223. ISSN 0047-2085. S2CID 165119472. Retrieved 17 February 2021.
- Levinovitz A (29 April 2015). "An Alternative-Medicine Believer's Journey Back to Science". WIRED. Retrieved 13 February 2017.
The entire diagnosis and explanation took no more than 45 minutes. 'In the moment of diagnosis, it feels like the death of your hopes and dreams,' Louise [Laidler] says. There's a quiet grief in her voice, even though two decades have passed. 'In a way, it's even harder than a death, because you can't mourn and go on,' she says. 'You have to figure out how to care for your new child.'
- Karst JS, Van Hecke AV (September 2012). "Parent and family impact of autism spectrum disorders: a review and proposed model for intervention evaluation". Clinical Child and Family Psychology Review. 15 (3): 247–77. doi:10.1007/s10567-012-0119-6. PMID 22869324. S2CID 19170894.
- Montes G, Halterman JS (April 2008). "Association of childhood autism spectrum disorders and loss of family income". Pediatrics. 121 (4): e821–e826. doi:10.1542/peds.2007-1594. PMID 18381511. S2CID 55179. Archived from the original on 4 March 2010.
- Montes G, Halterman JS (July 2008). "Child care problems and employment among families with preschool-aged children with autism in the United States". Pediatrics. 122 (1): e202–e208. doi:10.1542/peds.2007-3037. PMID 18595965. S2CID 22686553. Archived from the original on 6 December 2009.
- Piven J, Palmer P, Jacobi D, Childress D, Arndt S (February 1997). "Broader autism phenotype: evidence from a family history study of multiple-incidence autism families". The American Journal of Psychiatry. 154 (2): 185–190. doi:10.1176/ajp.154.2.185. PMID 9016266.
Sources
- "Neurodevelopmental Disorders". Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR). Washington, DC: American Psychiatric Association. 18 March 2022. ISBN 9780890425770. LCCN 2021051782.
- "6A02 Autism spectrum disorder". International Classification of Diseases 11th Revision (ICD-11). World Health Organisation. February 2022 [adopted in 2019]. 6A02. Retrieved 14 May 2022.
Further reading
- Gabovitch, Elaine; Dutra, Courtney; Lauer, Emily. (2016). The Healthy People 2020 Roadmap for Massachusetts Children & Youth with ASD/DD: Understanding Needs and Measuring Outcomes (Report). Worcester: UMASS Chan Medical School. Retrieved 30 June 2022.
- Matson JL, Dempsey T (2008). "Stereotypy in Adults with Autism Spectrum Disorders: Relationship and Diagnostic Fidelity". Journal of Developmental and Physical Disabilities, 20(2) 155–165. doi 10.1007/s10882-007-9086-0. S2CID 143874013.
- Johnny L Matson; Michael L Matson; Tessa T Rivet (September 2007). "Social-skills treatments for children with autism spectrum disorders: an overview". Behavior Modification. 31 (5): 682–707. doi:10.1177/0145445507301650. ISSN 0145-4455. PMID 17699124. Wikidata Q28240738.
- Johnny L Matson; Mary Shoemaker (14 July 2009). "Intellectual disability and its relationship to autism spectrum disorders". Research in Developmental Disabilities. 30 (6): 1107–1114. doi:10.1016/J.RIDD.2009.06.003. ISSN 0891-4222. PMID 19604668. Wikidata Q37552242. eISSN 1873-3379
- Pedersen AL, Pettygrove S, Lu Z, Andrews J, Meaney FJ, Kurzius-Spencer M, et al. (August 2017). "DSM Criteria that Best Differentiate Intellectual Disability from Autism Spectrum Disorder". Child Psychiatry and Human Development, 48(4): 537–545. doi:10.1007/s10578-016-0681-0. PMID 27558812. S2CID 4377173.
- Volkmar, Fred R.; Wiesner, Lisa A. (2009). A practical guide to autism: what every parent, family member, and teacher needs to know. Hoboken: Wiley. ISBN 9780470394731. OCLC 748908084. Retrieved 12 July 2022.
| Library resources about Autism spectrum |