Chlortalidone
Chlortalidone, also known as chlorthalidone, is a thiazide-like diuretic drug[1] used to treat high blood pressure, swelling including that due to heart failure, liver failure, and nephrotic syndrome, diabetes insipidus, and renal tubular acidosis.[2][3] Because chlortalidone is reliably effective in most patients with high blood pressure, it is considered a preferred initial treatment.[4][2] It is also used to prevent calcium-based kidney stones.[2] It is taken by mouth.[2] Effects generally begin within three hours and last for up to three days.[2] Chlortalidone is more effective than hydrochlorothiazide for prevention of heart attack or stroke.[5]
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Hygroton, Thalitone, others |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a682342 |
| License data | |
| Pregnancy category |
|
| Routes of administration | By mouth |
| Drug class | Thiazide-like diuretic |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Protein binding | 75% |
| Elimination half-life | 40 hours |
| Excretion | Kidney |
| Identifiers | |
IUPAC name
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.000.930 |
| Chemical and physical data | |
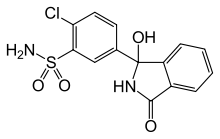
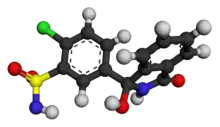
| Formula | C14H11ClN2O4S |
| Molar mass | 338.76 g·mol−1 |
| 3D model (JSmol) | |
| Chirality | Racemic mixture |
SMILES
| |
InChI
| |
| (verify) | |
Common adverse effects include low blood potassium, low blood sodium, high blood sugar, dizziness, and erectile dysfunction.[2][3][6] Other adverse effects may include gout, low blood magnesium, high blood calcium, allergic reactions, and low blood pressure.[2][3][7] Some reviews have found chlortalidone and hydrochlorothiazide to have a similar risk of adverse effects,[8][9] while other reviews have found chlortalidone to have a higher risk.[1][10] While it may be used in pregnancy it is a less preferred option.[2] How it works is not completely clear but is believed to involve increasing the amount of sodium and water lost by the kidneys.[2]
Chlortalidone was patented in 1957 and came into medical use in 1960.[11] It is on the World Health Organization's List of Essential Medicines.[12] It is available as a generic medication.[3] In 2020, it was the 133rd most commonly prescribed medication in the United States, with more than 4 million prescriptions.[13][14]
Medical use
High blood pressure
Chlortalidone is considered a first-line medication for treatment high blood pressure.[2] Some recommend chlortalidone over hydrochlorothiazide.[1][15] A meta-analysis of randomized controlled trials found that chlortalidone is more effective than hydrochlorothiazide for lowering blood pressure, while the two drugs have similar toxicity.[16][17][1][10]
Trials of chlortalidone for high blood pressure found that lower doses of chlortalidone (e.g., 12.5 mg daily in ALLHAT study) had maximal blood pressure lowering effect and that higher doses did not lower it more. Chlortalidone and other thiazide diuretics are effective for lowering high blood pressure in persons with chronic kidney disease, although the risk of adverse effects is higher in these persons.[18][19][20] [21]
Left ventricular hypertrophy
Chlortalidone is used to treat left ventricular hypertrophy in the heart; it works chiefly by lowering blood pressure, and thereby reducing systemic vascular resistance. There is evidence that chlortalidone is superior to hydrochlorothiazide for reducing the mass of the left ventricle of the heart in persons with enlargement of the left ventricle of the heart.[22] Chlortalidone is superior to angiotensin converting enzyme Inhibitors or angiotensin II receptor blockers for inducing regression of enlargement of the left ventricle, which is the main pumping chamber of the heart.[23]
Swelling
Chlortalidone reduces edema (swelling) by increasing urinary salt and water excretion, lowering intravascular hydrostatic pressure and thereby lowering transcapillary pressure (see Starling Equation). Edema may be caused by either increased hydrostatic pressure or reduced oncotic pressure in the blood vessels. Edema due to increased hydrostatic pressure may be a result of serious cardiopulmonary disease (which reduces glomerular perfusion in the kidney) or to kidney injury or disease (which may reduce glomerular excretion of salt and water by the kidney) or due to relatively benign conditions such as menstrual-related fluid retention, or as an adverse effect of dihydropyridine calcium channel blockers, which commonly cause swelling of the feet and lower legs. Edema due to decreased oncotic pressure may be a result of leaking of blood proteins through the glomeruli of an injured kidney[24] or a result of diminished synthesis of blood proteins by a damaged liver. Regardless of cause, chlortalidone may reduce the severity of edema by reducing intravascular volume and thereby reducing intravascular hydrostatic pressure.[25]
Bone fracture prevention
Chlortalidone decreases mineral bone loss by promoting calcium retention by the kidney, and by directly stimulating osteoblast differentiation and bone mineral formation.[26] A Cochrane review found tentative evidence that thiazide exposure was associated with a reduced risk of hip fracture.[27] A secondary analysis of data from the ALLHAT study found that chlortalidone reduced risk of hip and pelvis fracture.[28]
Kidney stone prevention
Chlortalidone reduces the amount of calcium excreted in urine, reducing the risk of calcium oxalate kidney stones.[29] In people who have had multiple episodes of calcium oxalate kidney stones, chlortalidone lowers the risk of having another episode of kidney stones.[30] Chlortalidone is more effective than hydrochlorothiazide for lowering urine calcium levels and is therefore probably more effective.[31]
Ménière's disease
Chlortalidone reduces the volume and thereby reduces the pressure in the inner ear chambers; elevated endolymph pressure in the inner ear is thought to be the cause of Ménière's disease or ’Endolymphatic hydrops.’ Synthesis of evidence from multiple small, low-quality studies indicates that chlortalidone or other thiazide diuretics are effective for Ménière's Disease.[32]
Diabetes insipidus
Chlortalidone (or other thiazide medication) is a key component of treatment of nephrogenic diabetes insipidus. Nephrogenic diabetes insipidus occurs when the kidney is unable to produce concentrated urine because it has an inadequate response to vasopressin-dependent removal of free water from the renal tubular filtrate. By blocking sodium ion resorption in the distal convoluted tubule, chlortalidone induces an increase in excretion of sodium ion in urine (natriuresis). Giving chlortalidone while simultaneously restricting dietary sodium intake causes mild hypovolemia (low intravascular volume), which induces isotonic reabsorption of solute from the proximal renal tubule, reducing solute delivery in the renal collecting tubule and renal medullary collecting duct. This reduced delivery of solute to the collecting tubule and medullary collecting duct allows increased water resorption and higher concentration of urine, which leads to reversal of nephrogenic diabetes insipidus by a means that is independent of vasopressin.[33]
Adverse effects
Some reviews have found a similar risk as hydrochlorothiazide,[8][9] while other reviews found a higher risk of side effects.[1][10]
- Hypokalemia (low blood potassium) occurs occasionally; the risk of hypokalemia is higher in persons who are magnesium deficient[34]
- Hypomagnesemia (low blood magnesium) a review of four clinical trials found that low blood magnesium occurred in 20% of persons within a few weeks of beginning treatment with 50 mg of chlortalidone daily.[35] The risk of chlortalidone-associated hypomagnesemia is higher in persons with diabetes mellitus who have low dietary magnesium intake.
- Hyponatremia (low blood sodium) occurred in 4.1% of subjects randomized to chlortalidone in the Systolic Hypertension in the Elderly Trial, compared to 1.3% of control subjects.[36] The risk of hyponatremia varies from 5 per 100,000 person-years for those younger than 40 years of age to 730 per 100,000 person-years in those older than 80 years of age.[37][38] Hyponatremia is more likely in persons with certain genetic variants of the prostaglandin transporter SLCO2A1 associated with elevated urinary PGE2 and inappropriately low plasma ADH levels in the setting of low plasma osmolality.[39] Thiazide-associated hyponatremia is often more severe than loop diuretic-associated hyponatremia because the predominant action of thiazides occurs late in the tubular flow, reducing opportunity to apply additional corrective action further along the tubule.[40]
- Hypercalcemia (high blood calcium level) can occur in normal persons exposed to chlortalidone but is more likely to occur when persons with sub-clinical hyperparathyroidism are exposed to chlortalidone.[41]
- Hyperuricemia, high levels of uric acid in the blood
- Hyperglycemia, high blood sugar is more common in persons who are magnesium deficient
- Hyperlipidemia, high cholesterol and triglycerides
- Headache
- Nausea/vomiting
- Photosensitivity increased susceptibility to sunburn of skin with sun exposure
- Photoonycholysis detachment of nails from nailbed with sun exposure[42]
- Weight gain
- Gout; approximately doubles the risk[43]
- Pancreatitis
The frequency and severity of these adverse effects is much reduced when chlortalidone is used at lower doses (e.g., 12.5 mg per day).
Mechanism of action
Chlortalidone reduces reabsorption of sodium and chloride primarily through inhibition of the Na+/Cl− symporter in the apical membrane of distal convoluted tubule cells in the kidney.[44] Although chlortalidone is often referred to as a "thiazide-like" diuretic, it is unlike thiazide diuretics in that, in addition to its inhibition of the Na+/Cl− symporter, it also strongly inhibits multiple isoforms of carbonic anhydrase.[45] Some of chlortalidone's diuretic effect is also due to this inhibition of carbonic anhydrase in the proximal tubule.[46] Chronic exposure to chlortalidone decreases the glomerular filtration rate. Chlortalidone's diuretic effect is diminished in persons with kidney impairment. By increasing the delivery of sodium to the distal renal tubule, chlortalidone indirectly increases potassium excretion via the sodium-potassium exchange mechanism (i.e. apical ROMK/Na channels coupled with basolateral Na+/K ATPases). This can result in a low blood concentration of potassium and chloride as well as a mild metabolic alkalosis; however, the diuretic effect of chlortalidone is not affected by the acid-base balance of the person being treated.
There is uncertainty about the mechanism of the blood pressure-lowering effect that occurs during chronic exposure to chlortalidone.[47] Initially, diuretics lower blood pressure by decreasing cardiac output and reducing plasma and extracellular fluid volume. Eventually, cardiac output returns to normal, and plasma and extracellular fluid volume return to slightly less than normal, but a reduction in peripheral vascular resistance is maintained, thus resulting in an overall lower blood pressure. The reduction in intravascular volume induces an elevation in plasma renin activity and aldosterone secretion, further contributing to the potassium loss associated with thiazide diuretic therapy.
Pharmacokinetics
Chlortalidone is slowly absorbed from the gastrointestinal tract after oral ingestion. It has a long half-life and therefore a prolonged diuretic action, which results in continued diuretic effects despite a skipped dose. This prolonged action of chlortalidone despite missing doses may account for the higher efficacy of chlortalidone compared to the shorter half-life medication, hydrochlorothiazide. Chlortalidone is eliminated from the body mostly by the kidney, as unchanged drug. Thus, in persons with diminished kidney function, the clearance of chlortalidone is reduced and the elimination half-life is increased.[48]
As with other thiazide diuretics, chlortalidone crosses the placenta and is excreted in breast milk.[49] Chlortalidone may suppress lactation, and has been used for this indication. Due to its long half-life, chlortalidone may accumulate in newborns via breast milk, despite receiving only about 6% of the maternal weight-adjusted dose.[50]
Chemistry
Chlortalidone is in the sulfamoylbenzamide class. As it lacks the benzothiadiazine structure of the thiazide-type diuretics, it is called a thiazide-like diuretic.[51] Chlortalidone is freely soluble in dimethylacetamide (DMA), dimethylformamide (DMF), dimethylsulfoxide (DMSO), and methanol; it is also soluble in warm ethanol.[52]
Chlortalidone is the official name of the medication according to the (INN/BAN), which is the medication naming system coordinated by the World Health Organization. Chlorthalidone is the official name of the medication according to the (USAN), which is the medication naming system coordinated by the USAN Council, which is co-sponsored by the American Medical Association (AMA), the United States Pharmacopeial Convention (USP), and the American Pharmacists Association (APhA).
Society and culture
Chlortalidone is banned for some sports (including cricket) because it is a diuretic, and can be used to reduce body weight or to mask the concomitant use of performance-enhancing drugs.[53] Sports such as wrestling or boxing categorize athletes according to body weight; taking a diuretic such as chlortalidone may lower body weight, and thereby permit an athlete to compete in a lighter weight class, which would provide an advantage. Diuretics such as chlortalidone also reduce the urine concentration of concomitantly-taken performance-enhancing drugs or of their metabolites, thus making it more difficult to detect these drugs using urine testing.[54]
References
- Acelajado MC, Hughes ZH, Oparil S, Calhoun DA (March 2019). "Treatment of Resistant and Refractory Hypertension". Circ. Res. 124 (7): 1061–1070. doi:10.1161/CIRCRESAHA.118.312156. PMC 6469348. PMID 30920924.
A long-acting thiazide-like diuretic, specifically chlorthalidone, if available, is recommended over hydrochlorothiazide (HCTZ) given its superior efficacy and clear benefit demonstrated in multiple outcome studies of hypertension.
- "Chlorthalidone Monograph for Professionals". Drugs.com. American Society of Health-System Pharmacists. Retrieved 18 April 2019.
- British national formulary : BNF 76 (76 ed.). Pharmaceutical Press. 2018. pp. 229–230. ISBN 9780857113382.
- Ernst, Michael E; Fravel, Michelle A (1 July 2022). "Thiazide and the Thiazide-Like Diuretics: Review of Hydrochlorothiazide, Chlorthalidone, and Indapamide". American Journal of Hypertension. 35 (7): 573–586. doi:10.1093/ajh/hpac048.
- Roush GC, Messerli FH (January 2021). "Chlorthalidone versus hydrochlorothiazide: major cardiovascular events, blood pressure, left ventricular mass, and adverse effects". J Hypertens. 39 (6): 1254–1260. doi:10.1097/HJH.0000000000002771. PMID 33470735. S2CID 231649367.
- Liamis G, Filippatos TD, Elisaf MS (February 2016). "Thiazide-associated hyponatremia in the elderly: what the clinician needs to know". Journal of Geriatric Cardiology. 13 (2): 175–82. doi:10.11909/j.issn.1671-5411.2016.02.001. PMC 4854958. PMID 27168745.
- "Chlorthalidone" (PDF). FDA. Retrieved 27 March 2020.
- Dineva S, Uzunova K, Pavlova V, Filipova E, Kalinov K, Vekov T (November 2019). "Comparative efficacy and safety of chlorthalidone and hydrochlorothiazide-meta-analysis". Journal of Human Hypertension. 33 (11): 766–774. doi:10.1038/s41371-019-0255-2. PMC 6892412. PMID 31595024.
- Roush GC, Abdelfattah R, Song S, Ernst ME, Sica DA, Kostis JB (October 2018). "Hydrochlorothiazide vs chlorthalidone, indapamide, and potassium-sparing/hydrochlorothiazide diuretics for reducing left ventricular hypertrophy: A systematic review and meta-analysis". Journal of Clinical Hypertension. 20 (10): 1507–1515. doi:10.1111/jch.13386. PMC 8030834. PMID 30251403.
- Springer K (December 2015). "Chlorthalidone vs. Hydrochlorothiazide for Treatment of Hypertension". American Family Physician. 92 (11): 1015–6. PMID 26760416.
- Fischer J, Ganellin CR (2006). Analogue-based Drug Discovery. John Wiley & Sons. p. 457. ISBN 9783527607495.
- World Health Organization (2021). World Health Organization model list of essential medicines: 22nd list (2021). Geneva: World Health Organization. hdl:10665/345533. WHO/MHP/HPS/EML/2021.02.
- "The Top 300 of 2020". ClinCalc. Retrieved 7 October 2022.
- "Chlorthalidone - Drug Usage Statistics". ClinCalc. Retrieved 7 October 2022.
- Vongpatanasin W (July 2015). "Hydrochlorothiazide is not the most useful nor versatile thiazide diuretic". Curr. Opin. Cardiol. 30 (4): 361–5. doi:10.1097/HCO.0000000000000178. PMC 4460599. PMID 26049382.
- Dineva S, Uzunova K, Pavlova V, Filipova E, Kalinov K, Vekov T (November 2019). "Comparative efficacy and safety of chlorthalidone and hydrochlorothiazide-meta-analysis". J Hum Hypertens. 33 (11): 766–774. doi:10.1038/s41371-019-0255-2. PMC 6892412. PMID 31595024.
- Carey RM, Whelton PK (March 2018). "Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Synopsis of the 2017 American College of Cardiology/American Heart Association Hypertension Guideline". Ann. Intern. Med. 168 (5): 351–358. doi:10.7326/M17-3203. PMID 29357392.
- Pourafshar N, Alshahrani S, Karimi A, Soleimani M (2018). "Thiazide Therapy in Chronic Kidney Disease: Renal and Extra Renal Targets". Curr. Drug Metab. 19 (12): 1012–1020. doi:10.2174/1389200219666180702104559. PMID 29962339. S2CID 49650101.
- Sinha AD, Agarwal R (March 2015). "Thiazide Diuretics in Chronic Kidney Disease". Curr. Hypertens. Rep. 17 (3): 13. doi:10.1007/s11906-014-0525-x. PMID 25749608. S2CID 6108618.
- Musini VM, Nazer M, Bassett K, Wright JM (May 2014). "Blood pressure-lowering efficacy of monotherapy with thiazide diuretics for primary hypertension". Cochrane Database Syst Rev (5): CD003824. doi:10.1002/14651858.CD003824.pub2. PMID 24869750.
- Sinha AD, Agarwal R (May 2019). "Clinical Pharmacology of Antihypertensive Therapy for the Treatment of Hypertension in CKD". Clin J Am Soc Nephrol. 14 (5): 757–764. doi:10.2215/CJN.04330418. PMC 6500954. PMID 30425103.
thiazides either alone or in combination with a loop diuretic in advanced CKD, and all show some degree of efficacy, whether for hypertension or diuresis
- Roush GC, Abdelfattah R, Song S, Ernst ME, Sica DA, Kostis JB (October 2018). "Hydrochlorothiazide vs chlorthalidone, indapamide, and potassium-sparing/hydrochlorothiazide diuretics for reducing left ventricular hypertrophy: A systematic review and meta-analysis". The Journal of Clinical Hypertension. 20 (10): 1507–1515. doi:10.1111/jch.13386. PMC 8030834. PMID 30251403.
- Roush GC, Abdelfattah R, Song S, Kostis JB, Ernst ME, Sica DA (June 2018). "Hydrochlorothiazide and alternative diuretics versus renin-angiotensin system inhibitors for the regression of left ventricular hypertrophy: a head-to-head meta-analysis". J. Hypertens. 36 (6): 1247–1255. doi:10.1097/HJH.0000000000001691. PMID 29465713. S2CID 3423953.
- Khan S, Floris M, Pani A, Rosner MH (July 2016). "Sodium and Volume Disorders in Advanced Chronic Kidney Disease". Adv Chronic Kidney Dis. 23 (4): 240–6. doi:10.1053/j.ackd.2015.12.003. PMID 27324677.
- O'Brien JG, Chennubhotla SA, Chennubhotla RV (June 2005). "Treatment of edema". Am Fam Physician. 71 (11): 2111–7. PMID 15952439.
- Dvorak MM, De Joussineau C, Carter DH, Pisitkun T, Knepper MA, Gamba G, et al. (September 2007). "Thiazide diuretics directly induce osteoblast differentiation and mineralized nodule formation by interacting with a sodium chloride co-transporter in bone". Journal of the American Society of Nephrology. 18 (9): 2509–16. doi:10.1681/ASN.2007030348. PMC 2216427. PMID 17656470.
- Aung K, Htay T (October 2011). "Thiazide diuretics and the risk of hip fracture". The Cochrane Database of Systematic Reviews (10): CD005185. doi:10.1002/14651858.CD005185.pub2. PMID 21975748. S2CID 28866803.
- Puttnam R, Davis BR, Pressel SL, Whelton PK, Cushman WC, Louis GT, et al. (January 2017). "Association of 3 Different Antihypertensive Medications With Hip and Pelvic Fracture Risk in Older Adults: Secondary Analysis of a Randomized Clinical Trial". JAMA Internal Medicine. 177 (1): 67–76. doi:10.1001/jamainternmed.2016.6821. PMID 27893045.
- Pearle MS, Roehrborn CG, Pak CY (November 1999). "Meta-analysis of randomized trials for medical prevention of calcium oxalate nephrolithiasis". J. Endourol. 13 (9): 679–85. doi:10.1089/end.1999.13.679. PMID 10608521. S2CID 2514178.
- Fink HA, Wilt TJ, Eidman KE, Garimella PS, MacDonald R, Rutks IR, Brasure M, Kane RL, Ouellette J, Monga M (April 2013). "Medical management to prevent recurrent nephrolithiasis in adults: a systematic review for an American College of Physicians Clinical Guideline". Ann. Intern. Med. 158 (7): 535–43. doi:10.7326/0003-4819-158-7-201304020-00005. PMID 23546565.
- Wolfgram DF, Gundu V, Astor BC, Jhagroo RA (August 2013). "Hydrochlorothiazide compared to chlorthalidone in reduction of urinary calcium in patients with kidney stones". Urolithiasis. 41 (4): 315–22. doi:10.1007/s00240-013-0568-5. PMID 23660825. S2CID 10227907.
- Crowson MG, Patki A, Tucci DL (May 2016). "A Systematic Review of Diuretics in the Medical Management of Ménière's Disease". Otolaryngol Head Neck Surg. 154 (5): 824–34. doi:10.1177/0194599816630733. PMID 26932948. S2CID 24741244.
- Verbalis JG (May 2003). "Diabetes insipidus". Rev Endocr Metab Disord. 4 (2): 177–85. doi:10.1023/a:1022946220908. PMID 12766546. S2CID 33533827.
- DiNicolantonio JJ, O'Keefe JH, Wilson W (2018). "Subclinical magnesium deficiency: a principal driver of cardiovascular disease and a public health crisis". Open Heart. 5 (1): e000668. doi:10.1136/openhrt-2017-000668. PMC 5786912. PMID 29387426.
- Pak CY (October 2000). "Correction of thiazide-induced hypomagnesemia by potassium-magnesium citrate from review of prior trials". Clin. Nephrol. 54 (4): 271–5. PMID 11076102.
- "Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension. Final results of the Systolic Hypertension in the Elderly Program (SHEP). SHEP Cooperative Research Group". JAMA. 265 (24): 3255–64. June 1991. doi:10.1001/jama.1991.03460240051027. PMID 2046107.
- Barber J, McKeever TM, McDowell SE, Clayton JA, Ferner RE, Gordon RD, Stowasser M, O'Shaughnessy KM, Hall IP, Glover M (April 2015). "A systematic review and meta-analysis of thiazide-induced hyponatraemia: time to reconsider electrolyte monitoring regimens after thiazide initiation?". Br J Clin Pharmacol. 79 (4): 566–77. doi:10.1111/bcp.12499. PMC 4386942. PMID 25139696.
- van Blijderveen JC, Straus SM, Rodenburg EM, Zietse R, Stricker BH, Sturkenboom MC, Verhamme KM (August 2014). "Risk of hyponatremia with diuretics: chlorthalidone versus hydrochlorothiazide". Am. J. Med. 127 (8): 763–71. doi:10.1016/j.amjmed.2014.04.014. PMID 24811554.
- Ware JS, Wain LV, Channavajjhala SK, Jackson VE, Edwards E, Lu R, Siew K, Jia W, Shrine N, Kinnear S, Jalland M, Henry AP, Clayton J, O'Shaughnessy KM, Tobin MD, Schuster VL, Cook S, Hall IP, Glover M (September 2017). "Phenotypic and pharmacogenetic evaluation of patients with thiazide-induced hyponatremia". J. Clin. Invest. 127 (9): 3367–3374. doi:10.1172/JCI89812. PMC 5669583. PMID 28783044.
- Peri A (2019). Disorders of fluid and electrolyte metabolism : focus on hyponatremia. Basel New York: Karger. ISBN 978-3-318-06383-7.
- Griebeler ML, Kearns AE, Ryu E, Thapa P, Hathcock MA, Melton LJ, Wermers RA (March 2016). "Thiazide-Associated Hypercalcemia: Incidence and Association With Primary Hyperparathyroidism Over Two Decades". J. Clin. Endocrinol. Metab. 101 (3): 1166–73. doi:10.1210/jc.2015-3964. PMC 4803175. PMID 26751196.
- Rubin A (2018). Scher and Daniel's nails : diagnosis, surgery, therapy. Cham: Springer. pp. 453–489. ISBN 978-3319656472.
- Evans PL, Prior JA, Belcher J, Mallen CD, Hay CA, Roddy E (July 2018). "Obesity, hypertension and diuretic use as risk factors for incident gout: a systematic review and meta-analysis of cohort studies". Arthritis Res. Ther. 20 (1): 136. doi:10.1186/s13075-018-1612-1. PMC 6034249. PMID 29976236.
- Gamba G (October 2009). "The thiazide-sensitive Na+-Cl- cotransporter: molecular biology, functional properties, and regulation by WNKs". Am. J. Physiol. Renal Physiol. 297 (4): F838–48. doi:10.1152/ajprenal.00159.2009. PMC 3350128. PMID 19474192.
- Kurtz TW (September 2010). "Chlorthalidone: don't call it "thiazide-like" anymore". Hypertension. 56 (3): 335–7. doi:10.1161/HYPERTENSIONAHA.110.156166. PMID 20625074.
- Johnston MM, Li H, Mufson D (December 1977). "Chlorthalidone analysis using carbonic anhydrase inhibition". J Pharm Sci. 66 (12): 1735–8. doi:10.1002/jps.2600661220. PMID 411910.
- Shahin MH, Johnson JA (April 2016). "Mechanisms and pharmacogenetic signals underlying thiazide diuretics blood pressure response". Curr Opin Pharmacol. 27: 31–7. doi:10.1016/j.coph.2016.01.005. PMC 4915478. PMID 26874237.
- Singer, Jeff M., Michael J. O'Hare, Carl R. Rehm, and John E. Zarembo. "Chlorthalidone." In Analytical Profiles of Drug Substances, vol. 14, pp. 1-36. Academic Press, 1985.
- Mulley BA, Parr GD, Pau WK, Rye RM, Mould JJ, Siddle NC (May 1978). "Placental transfer of chlorthalidone and its elimination in maternal milk". Eur. J. Clin. Pharmacol. 13 (2): 129–31. doi:10.1007/bf00609757. PMID 658109. S2CID 22930934.
- "LACTMED: CHLORTHALIDONE". toxnet.nlm.nih.gov. U.S. National Library of Medicine. Retrieved 13 December 2018.
- National Center for Biotechnology Information. PubChem Compound Database; CID=2732, "Chlorthalidone". PubChem. U.S. National Library of Medicine.
- Singer JM, O'Hare MJ, Rehm CR, Zarembo JE (January 1985). "Chlorthalidone". Analytical Profiles of Drug Substances. Vol. 14. Academic Press. pp. 1–36. doi:10.1016/S0099-5428(08)60575-4. ISBN 9780122608148.
- Cadwallader AB, de la Torre X, Tieri A, Botrè F (September 2010). "The abuse of diuretics as performance-enhancing drugs and masking agents in sport doping: pharmacology, toxicology and analysis". Br. J. Pharmacol. 161 (1): 1–16. doi:10.1111/j.1476-5381.2010.00789.x. PMC 2962812. PMID 20718736.
- "Yasir Shah provisionally suspended after failed drugs test". BBC News. 27 December 2015.
External links
- "Chlorthalidone". Drug Information Portal. U.S. National Library of Medicine.