Hyper IgM syndrome
Hyper IgM syndrome describes a group of primary immune deficiency disorders characterized by defective CD40 signaling; via B cells affecting class switch recombination (CSR) and somatic hypermutation. Immunoglobulin (Ig) class switch recombination deficiencies are characterized by elevated serum Immunoglobulin M (IgM) levels and a considerable deficiency in Immunoglobulins G (IgG), A (IgA) and E (IgE). As a consequence, people with HIGM have decreased concentrations of serum IgG and IgA and normal or elevated IgM, leading to increased susceptibility to infections.[8][7][9]
| Hyper IgM syndrome | |
|---|---|
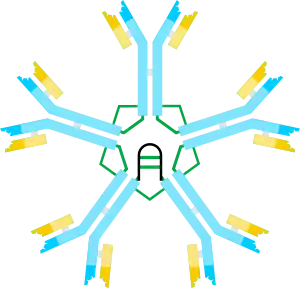 | |
| Immunoglobulin M | |
| Specialty | Immunology |
| Symptoms | Chronic diarrhea[1] |
| Types | Hyper-IgM syndrome type 1, 2, 3, 4 and 5[2][3][4][5][6] |
| Diagnostic method | MRI, Chest radiography[1] |
| Treatment | Allogeneic hematopoietic cell transplantation[7] |
Signs and symptoms
Among the presentation consistent with hyper IgM syndrome are the following:[1][10]
- Infection/Pneumocystis pneumonia (PCP), which is common in infants with hyper IgM syndrome, is a serious illness.[8] PCP is one of the most frequent and severe opportunistic infections in people with weakened immune systems. Many CD40 Ligand Deficiency are first diagnosed after having PCP in their first year of life. The fungus is common and is present in over 70% of healthy people's lungs, however, Hyper IgM patients are not able to fight it off without the administration of Bactrim
- Hepatitis (Hepatitis C)
- Chronic diarrhea
- Hypothyroidism
- Neutropenia
- Arthritis
- Encephalopathy (degenerative)
Cause
Different genetic defects cause HIgM syndrome, the vast majority are inherited as an X-linked recessive genetic trait and most with the condition are male.[7]
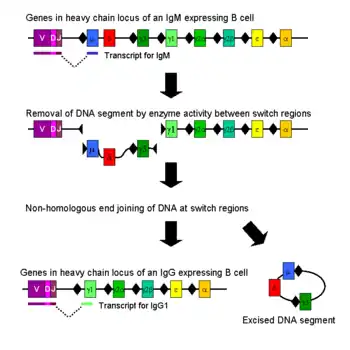
IgM is the form of antibody that all B cells produce initially before they undergo class switching due to exposure to a recognized antigen. Healthy B cells efficiently switch to other types of antibodies as needed to attack invading bacteria, viruses, and other pathogens. In people with hyper IgM syndromes, the B cells keep making IgM antibodies because they can't switch to a different antibody. This results in an overproduction of IgM antibodies and an underproduction of IgA, IgG, and IgE.[11][7]
Pathophysiology
CD40 is a co-stimulatory receptor on B cells that, when bound to CD40 ligand (CD40L), sends a signal to the B-cell receptor.[12] When there is a defect in CD40, this leads to defective T-cell interaction with B cells. Consequently, humoral immune response is affected. Certain insults, usually from encapsulated bacteria and toxin, then have a greater opportunity to damage the body.[1]
Diagnosis
The diagnosis of hyper IgM syndrome can be done via the following methods and tests:[1]
- MRI
- Chest radiography
- Pulmonary function test
- Lymph node test
- Laboratory test (to measure CD40)
Types
Five types of hyper IgM syndrome have been characterized:
- Hyper-IgM syndrome type 1 (X-linked), characterized by mutations of the CD40LG gene. In this type, T cells cannot tell B cells to switch classes.[2]
- Hyper-IgM syndrome type 2 (autosomal recessive), characterized by mutations of the AICDA gene. In this type, B cells cannot recombine genetic material to change heavy chain production[3]
- Hyper-IgM syndrome type 3 characterized by mutations of the CD40 gene. In this type, B cells cannot receive the signal from T cells to switch classes.[4]
- Hyper-IgM syndrome type 4 which is a defect in class switch recombination downstream of the AICDA gene that does not impair Somatic Hypermutation.[13]
- Hyper-IgM syndrome type 5 characterized by mutations of the UNG gene.[5]
Treatment
In terms of treatment for hyper IgM syndrome, there is the use of allogeneic hematopoietic cell transplantation. Additionally, anti-microbial therapy, use of granulocyte colony-stimulating factor, immunosuppressants, as well as other treatments, may be needed.[7]
See also
References
- "X-linked Immunodeficiency With Hyper IgM Clinical Presentation: History, Physical, Causes". emedicine.medscape.com. Retrieved 27 November 2016.
- "OMIM Entry - # 308230 - IMMUNODEFICIENCY WITH HYPER-IgM, TYPE 1; HIGM1". www.omim.org. Retrieved 16 November 2016.
- "OMIM Entry - # 605258 - IMMUNODEFICIENCY WITH HYPER-IgM, TYPE 2; HIGM2". omim.org. Retrieved 16 November 2016.
- "OMIM Entry - # 606843 - IMMUNODEFICIENCY WITH HYPER-IgM, TYPE 3; HIGM3". www.omim.org. Retrieved 16 November 2016.
- "OMIM Entry - # 608106 - IMMUNODEFICIENCY WITH HYPER-IgM, TYPE 5; HIGM5". omim.org. Retrieved 16 November 2016.
- "OMIM Entry - 608184 - IMMUNODEFICIENCY WITH HYPER-IgM, TYPE 4; HIGM4". www.omim.org. Retrieved 2 January 2018.
- Johnson, Judith; Filipovich, Alexandra H.; Zhang, Kejian (1 January 1993). "X-Linked Hyper IgM Syndrome". GeneReviews. PMID 20301576. Retrieved 12 November 2016.update 2013
- Etzioni, Amos; Ochs, Hans D. (1 October 2004). "The Hyper IgM Syndrome—An Evolving Story". Pediatric Research. 56 (4): 519–525. doi:10.1203/01.PDR.0000139318.65842.4A. ISSN 0031-3998. PMID 15319456.
- "Hyper-Immunoglobulin M (Hyper-IgM) Syndromes | NIH: National Institute of Allergy and Infectious Diseases". www. niaid.nih.gov. Retrieved 27 November 2016.
- Davies, E Graham; Thrasher, Adrian J (27 November 2016). "Update on the hyper immunoglobulin M syndromes". British Journal of Haematology. 149 (2): 167–180. doi:10.1111/j.1365-2141.2010.08077.x. ISSN 0007-1048. PMC 2855828. PMID 20180797.
- Reference, Genetics Home. "X-linked hyper IgM syndrome". Genetics Home Reference. Retrieved 27 November 2016.
- Reference, Genetics Home. "CD40 gene". Genetics Home Reference. Retrieved 27 November 2016.
- Lougaris V, Badolato R, Ferrari S, Plebani A (2005). "Hyper immunoglobulin M syndrome due to CD40 deficiency: clinical, molecular, and immunological features". Immunol. Rev. 203: 48–66. doi:10.1111/j.0105-2896.2005.00229.x. PMID 15661021. S2CID 6678540.subscription needed
Further reading
- Strober, Warren; Gottesman, Susan R. (2014). Immunology: Clinical Case Studies and Disease Pathophysiology. John Wiley & Sons. ISBN 9781118966006. Retrieved 27 November 2016.
- Kleinman, Ronald (2008). Walker's Pediatric Gastrointestinal Disease. PMPH-USA. ISBN 9781550093643. Retrieved 27 November 2016.