Thyroglobulin
Thyroglobulin (Tg) is a 660 kDa, dimeric glycoprotein produced by the follicular cells of the thyroid and used entirely within the thyroid gland. Tg is secreted and accumulated at hundreds of grams per litre in the extracellular compartment of the thyroid follicles, accounting for approximately half of the protein content of the thyroid gland.[5] Human TG (hTG) is a homodimer of subunits each containing 2768 amino acids as synthesized (a short signal peptide of 19 aminoacids may be removed from the N-terminus in the mature protein).[6]
| TG | |||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Identifiers | |||||||||||||||||||||||||||||||||||||||||||||||||||
| Aliases | TG, AITD3, TGN, thyroglobulin | ||||||||||||||||||||||||||||||||||||||||||||||||||
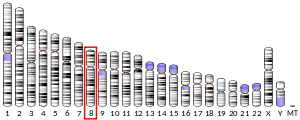
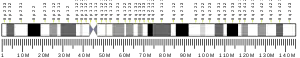
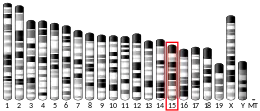
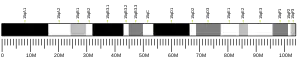
| External IDs | OMIM: 188450 MGI: 98733 HomoloGene: 2430 GeneCards: TG | ||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| Wikidata | |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
Thyroglobulin is in all vertebrates the main precursor to thyroid hormones, which are produced when thyroglobulin's tyrosine residues are combined with iodine and the protein is subsequently cleaved. Each thyroglobulin molecule contains approximately 100–120 tyrosine residues, but only a small number (20) of these are subject to iodination by thyroperoxidase in the follicular colloid. Therefore, each Tg molecule forms approximately 10 thyroid hormone molecules.[5]
Function
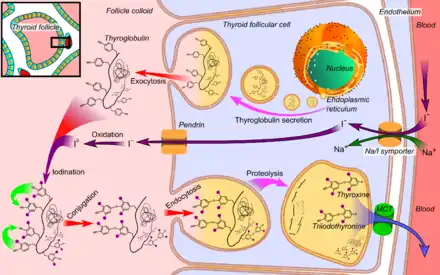
Thyroglobulin (Tg) acts as a substrate for the synthesis of the thyroid hormones thyroxine (T4) and triiodothyronine (T3), as well as the storage of the inactive forms of thyroid hormone and iodine within the follicular lumen of a thyroid follicle.[7]
Newly synthesized thyroid hormones (T3 and T4) are attached to thyroglobulin and comprise the colloid within the follicle. When stimulated by thyroid stimulating hormone (TSH), the colloid is endocytosed from the follicular lumen into the surrounding thyroid follicular epithelial cells. The colloid is subsequently cleaved by proteases to release thyroglobulin from its T3 and T4 attachments.[8]
The active forms of thyroid hormone: T3 and T4, are then released into circulation where they are either unbound or attached to plasma proteins, and thyroglobulin is recycled back into the follicular lumen where it can continue to serve as a substrate for thyroid hormone synthesis.[8]
Clinical significance
Half-life and clinical elevation
Metabolism of thyroglobulin occurs in the liver via thyroid gland recycling of the protein. Circulating thyroglobulin has a half-life of 65 hours. Following thyroidectomy, it may take many weeks before thyroglobulin levels become undetectable. Thyroglobulin levels may be tested regularly for a few weeks or months following the removal of the thyroid.[9] After thyroglobulin levels become undetectable (following thyroidectomy), levels can be serially monitored in follow-up of patients with papillary or follicular thyroid carcinoma.
A subsequent elevation of the thyroglobulin level is an indication of recurrence of papillary or follicular thyroid carcinoma. In other words, a rise in thyroglobulin levels in the blood may be a sign that thyroid cancer cells are growing and/or the cancer is spreading.[9] Hence, thyroglobulin levels in the blood are mainly used as a tumor marker[10][9] for certain kinds of thyroid cancer (particularly papillary or follicular thyroid cancer). Thyroglobulin is not produced by medullary or anaplastic thyroid carcinoma.
Thyroglobulin levels are tested via a simple blood test. Tests are often ordered after thyroid cancer treatment.[9]
Thyroglobulin antibodies
In the clinical laboratory, thyroglobulin testing can be complicated by the presence of anti-thyroglobulin antibodies (ATAs, alternatively referred to as TgAb). Anti-thyroglobulin antibodies are present in 1 in 10 normal individuals, and a greater percentage of patients with thyroid carcinoma. The presence of these antibodies can result in falsely low (or rarely falsely high) levels of reported thyroglobulin, a problem that can be somewhat circumvented by concomitant testing for the presence of ATAs. The ideal strategy for a clinician's interpretation and management of patient care in the event of confounding detection of ATAs is testing to follow serial quantitative measurements (rather than a single laboratory measurement).
ATAs are often found in patients with Hashimoto's thyroiditis or Graves' disease. Their presence is of limited use in the diagnosis of these diseases, since they may also be present in healthy euthyroid individuals. ATAs are also found in patients with Hashimoto's encephalopathy, a neuroendocrine disorder related to—but not caused by—Hashimoto's thyroiditis.[11]
References
- GRCh38: Ensembl release 89: ENSG00000042832 - Ensembl, May 2017
- GRCm38: Ensembl release 89: ENSMUSG00000053469 - Ensembl, May 2017
- "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- "Mouse PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- Boron WF (2003). Medical Physiology: A Cellular And Molecular Approach. Elsevier/Saunders. p. 1044. ISBN 1-4160-2328-3.
- "Protein" thyroglobulin precursor [Homo sapiens]". National Center for Biotechnology Information, U.S. National Library of Medicine.
- "TG thyroglobulin [Homo sapiens (human)] – Gene – NCBI". www.ncbi.nlm.nih.gov. Retrieved 2019-09-16.
- Rousset BL, Dupuy C, Miot F, Dumont J (2000). "Chapter 2 Thyroid Hormone Synthesis and Secretion". In Feingold KR, Anawalt B, Boyce A, Chrousos G (eds.). Endotext. MDText.com, Inc. PMID 25905405. Retrieved 2019-09-17.
- "Thyroglobulin: MedlinePlus Lab Test Information". medlineplus.gov. Retrieved 2019-05-06.
- "ACS :: Tumor Markers". American Cancer Society. Retrieved 2009-03-28.
- Ferracci F, Moretto G, Candeago RM, Cimini N, Conte F, Gentile M, et al. (February 2003). "Antithyroid antibodies in the CSF: their role in the pathogenesis of Hashimoto's encephalopathy". Neurology. 60 (4): 712–714. doi:10.1212/01.wnl.0000048660.71390.c6. PMID 12601119. S2CID 21610036.
- Delom F, Mallet B, Carayon P, Lejeune PJ (June 2001). "Role of extracellular molecular chaperones in the folding of oxidized proteins. Refolding of colloidal thyroglobulin by protein disulfide isomerase and immunoglobulin heavy chain-binding protein". The Journal of Biological Chemistry. 276 (24): 21337–21342. doi:10.1074/jbc.M101086200. PMID 11294872.
- Delom F, Lejeune PJ, Vinet L, Carayon P, Mallet B (February 1999). "Involvement of oxidative reactions and extracellular protein chaperones in the rescue of misassembled thyroglobulin in the follicular lumen". Biochemical and Biophysical Research Communications. 255 (2): 438–443. doi:10.1006/bbrc.1999.0229. PMID 10049727.
Further reading
- Coscia F, Taler-Verčič A, Chang VT, Sinn L, O'Reilly FJ, Izoré T, et al. (February 2020). "The structure of human thyroglobulin". Nature. 578 (7796): 627–630. Bibcode:2020Natur.578..627C. doi:10.1038/s41586-020-1995-4. PMC 7170718. PMID 32025030.
- Mazzaferri EL, Robbins RJ, Spencer CA, Braverman LE, Pacini F, Wartofsky L, et al. (April 2003). "A consensus report of the role of serum thyroglobulin as a monitoring method for low-risk patients with papillary thyroid carcinoma". The Journal of Clinical Endocrinology and Metabolism. 88 (4): 1433–1441. doi:10.1210/jc.2002-021702. PMID 12679418.
- Henry M, Zanelli E, Piechaczyk M, Pau B, Malthièry Y (February 1992). "A major human thyroglobulin epitope defined with monoclonal antibodies is mainly recognized by human autoantibodies". European Journal of Immunology. 22 (2): 315–319. doi:10.1002/eji.1830220205. PMID 1371467. S2CID 38620713.
- Targovnik HM, Cochaux P, Corach D, Vassart G (March 1992). "Identification of a minor Tg mRNA transcript in RNA from normal and goitrous thyroids". Molecular and Cellular Endocrinology. 84 (1–2): R23–R26. doi:10.1016/0303-7207(92)90087-M. PMID 1639210. S2CID 35326294.
- Dunn AD, Crutchfield HE, Dunn JT (October 1991). "Thyroglobulin processing by thyroidal proteases. Major sites of cleavage by cathepsins B, D, and L". The Journal of Biological Chemistry. 266 (30): 20198–20204. doi:10.1016/S0021-9258(18)54909-7. PMID 1939080.
- Lamas L, Anderson PC, Fox JW, Dunn JT (August 1989). "Consensus sequences for early iodination and hormonogenesis in human thyroglobulin". The Journal of Biological Chemistry. 264 (23): 13541–13545. doi:10.1016/S0021-9258(18)80031-X. PMID 2760035.
- Marriq C, Lejeune PJ, Venot N, Vinet L (January 1989). "Hormone synthesis in human thyroglobulin: possible cleavage of the polypeptide chain at the tyrosine donor site". FEBS Letters. 242 (2): 414–418. doi:10.1016/0014-5793(89)80513-7. PMID 2914619. S2CID 32367745.
- Christophe D, Cabrer B, Bacolla A, Targovnik H, Pohl V, Vassart G (July 1985). "An unusually long poly(purine)-poly(pyrimidine) sequence is located upstream from the human thyroglobulin gene". Nucleic Acids Research. 13 (14): 5127–5144. doi:10.1093/nar/13.14.5127. PMC 321854. PMID 2991855.
- Baas F, van Ommen GJ, Bikker H, Arnberg AC, de Vijlder JJ (July 1986). "The human thyroglobulin gene is over 300 kb long and contains introns of up to 64 kb". Nucleic Acids Research. 14 (13): 5171–5186. doi:10.1093/nar/14.13.5171. PMC 311533. PMID 3016640.
- Kubak BM, Potempa LA, Anderson B, Mahklouf S, Venegas M, Gewurz H, Gewurz AT (September 1988). "Evidence that serum amyloid P component binds to mannose-terminated sequences of polysaccharides and glycoproteins". Molecular Immunology. 25 (9): 851–858. doi:10.1016/0161-5890(88)90121-6. PMID 3211159.
- Malthiéry Y, Lissitzky S (June 1987). "Primary structure of human thyroglobulin deduced from the sequence of its 8448-base complementary DNA". European Journal of Biochemistry. 165 (3): 491–498. doi:10.1111/j.1432-1033.1987.tb11466.x. PMID 3595599.
- Parma J, Christophe D, Pohl V, Vassart G (August 1987). "Structural organization of the 5' region of the thyroglobulin gene. Evidence for intron loss and "exonization" during evolution". Journal of Molecular Biology. 196 (4): 769–779. doi:10.1016/0022-2836(87)90403-7. PMID 3681978.
- Bergé-Lefranc JL, Cartouzou G, Mattéi MG, Passage E, Malezet-Desmoulins C, Lissitzky S (1985). "Localization of the thyroglobulin gene by in situ hybridization to human chromosomes". Human Genetics. 69 (1): 28–31. doi:10.1007/BF00295525. PMID 3967888. S2CID 9234835.
- Malthiéry Y, Lissitzky S (February 1985). "Sequence of the 5'-end quarter of the human-thyroglobulin messenger ribonucleic acid and of its deduced amino-acid sequence". European Journal of Biochemistry. 147 (1): 53–58. doi:10.1111/j.1432-1033.1985.tb08717.x. PMID 3971976.
- Avvedimento VE, Di Lauro R, Monticelli A, Bernardi F, Patracchini P, Calzolari E, et al. (1985). "Mapping of human thyroglobulin gene on the long arm of chromosome 8 by in situ hybridization". Human Genetics. 71 (2): 163–166. doi:10.1007/BF00283375. PMID 4043966. S2CID 28315029.
- Xiao S, Pollock HG, Taurog A, Rawitch AB (June 1995). "Characterization of hormonogenic sites in an N-terminal, cyanogen bromide fragment of human thyroglobulin". Archives of Biochemistry and Biophysics. 320 (1): 96–105. doi:10.1006/abbi.1995.1346. PMID 7793989.
- Corral J, Martín C, Pérez R, Sánchez I, Mories MT, San Millan JL, et al. (February 1993). "Thyroglobulin gene point mutation associated with non-endemic simple goitre". Lancet. 341 (8843): 462–464. doi:10.1016/0140-6736(93)90209-Y. PMID 8094490. S2CID 34165624.
- Gentile F, Salvatore G (December 1993). "Preferential sites of proteolytic cleavage of bovine, human and rat thyroglobulin. The use of limited proteolysis to detect solvent-exposed regions of the primary structure". European Journal of Biochemistry. 218 (2): 603–621. doi:10.1111/j.1432-1033.1993.tb18414.x. PMID 8269951.
- Mallet B, Lejeune PJ, Baudry N, Niccoli P, Carayon P, Franc JL (December 1995). "N-glycans modulate in vivo and in vitro thyroid hormone synthesis. Study at the N-terminal domain of thyroglobulin". The Journal of Biological Chemistry. 270 (50): 29881–29888. doi:10.1074/jbc.270.50.29881. PMID 8530385.
- Yang SX, Pollock HG, Rawitch AB (March 1996). "Glycosylation in human thyroglobulin: location of the N-linked oligosaccharide units and comparison with bovine thyroglobulin". Archives of Biochemistry and Biophysics. 327 (1): 61–70. doi:10.1006/abbi.1996.0093. PMID 8615697.
- Molina F, Bouanani M, Pau B, Granier C (August 1996). "Characterization of the type-1 repeat from thyroglobulin, a cysteine-rich module found in proteins from different families". European Journal of Biochemistry. 240 (1): 125–133. doi:10.1111/j.1432-1033.1996.0125h.x. PMID 8797845.
- Grani G, Fumarola A (June 2014). "Thyroglobulin in lymph node fine-needle aspiration washout: a systematic review and meta-analysis of diagnostic accuracy". The Journal of Clinical Endocrinology and Metabolism. 99 (6): 1970–1982. doi:10.1210/jc.2014-1098. PMID 24617715.
External links
- First look at the structure of human TG
- Thyroglobulin – Lab Tests Online
- Histology at KUMC endo-endo11
- Overview at colostate.edu
- Histology image: 14302loa – Histology Learning System at Boston University