Trypanosoma brucei
Trypanosoma brucei is a species of parasitic kinetoplastid belonging to the genus Trypanosoma that is present in sub-Saharan Africa. Unlike other protozoan parasites that normally infect blood and tissue cells, it is exclusively extracellular and inhabits the blood plasma and body fluids.[1] It causes deadly vector-borne diseases: African trypanosomiasis or sleeping sickness in humans, and animal trypanosomiasis or nagana in cattle and horses.[2] It is a species complex grouped into three subspecies: T. b. brucei, T. b. gambiense and T. b. rhodesiense.[3] The first is a parasite of non-human mammals and causes nagana, while the latter two are zoonotic infecting both humans and animals and cause African trpanosomiasis.
| Trypanosoma brucei | |
|---|---|
 | |
| T. b. brucei TREU667 (Bloodstream form, phase-contrast picture. Black bar indicates 10 µm.) | |
| Scientific classification | |
| Domain: | Eukaryota |
| Phylum: | Euglenozoa |
| Class: | Kinetoplastea |
| Order: | Trypanosomatida |
| Family: | Trypanosomatidae |
| Genus: | Trypanosoma |
| Species: | T. brucei |
| Binomial name | |
| Trypanosoma brucei Plimmer & Bradford, 1899 | |
| Subspecies | |
| |
T. brucei is transmitted between mammal hosts by an insect vector belonging to different species of tsetse fly (Glossina). Transmission occurs by biting during the insect's blood meal. The parasites undergo complex morphological changes as they move between insect and mammal over the course of their life cycle. The mammalian bloodstream forms are notable for their cell surface proteins, variant surface glycoproteins, which undergo remarkable antigenic variation, enabling persistent evasion of host adaptive immunity leading to chronic infection. T. brucei is one of only a few pathogens known to cross the blood brain barrier.[4] There is an urgent need for the development of new drug therapies, as current treatments can have severe side effects and can prove fatal to the patient.[5]
Whilst not historically regarded as T. brucei subspecies due to their different means of transmission, clinical presentation, and loss of kinetoplast DNA, genetic analyses reveal that T. equiperdum and T. evansi are evolved from parasites very similar to T. b. brucei, and are thought to be members of the brucei clade.[6]
The parasite was discovered in 1894 by Sir David Bruce, after whom the scientific name was given in 1899.[7][8]
History and discovery
Early records
Sleeping sickness in animals were described in ancient Egyptian writings. During the Middle Ages, Arabian traders noted the prevalence of sleeping sickness among Africans and their dogs.[9] It was a major infectious diseases in southern and eastern Africa in the 19th century.[10] The Zulu Kingdom (now part of South Africa) was severely struck by the disease, which became known to the British as nagana,[2] a Zulu word for to be low or depressed in spirit. In other parts of Africa, Europeans called it the "fly disease."[11][12]

John Aktins, an English naval surgeon, gave first medical description of human sleeping sickness in 1734. He attributed deaths which he called "sleepy distemper" in Guinea to the infection.[13] Another English physician Thomas Masterman Winterbottom gave clearer description of the symptoms from Sierra Leone in 1803.[14] Winterbottom described a key feature of the disease as swollen posterior cervical lymph nodes and slaves who developed such swellings were ruled unfit for trade.[13] The symptom is eponymously known as "Winterbottom's sign."[15]
Discovery of the parasite
The Royal Army Medical Corps appointed David Bruce, who at the time was assistant professor of pathology at the Army Medical School in Netley with a rank of Captain in the army, in 1894 to investigate a disease known as nagana in South Africa. The disease caused severe problems among the local cattle and British Army horses.[3] On 27 October 1894, Bruce and his microbiologist-wife Mary Elizabeth Bruce (née Steele) moved to Ubombo Hill, where the disease was most prevalent.[16]
On the sixth day of investigation, Bruce identified parasites from the blood of diseased cows. He initially noted them as a kind of filaria (tiny roundworms), but by the end of the year established that the parasites were "haematozoa" (protozoan) and were the cause of nagana .[3] It was the discovery of Trypanosoma brucei.[17] The scientific name was created by British zoologists Henry George Plimmer and John Rose Bradford in 1899 as Trypanosoma brucii due to printer's error.[3][18] The genus Trypanosoma was already introduced by Hungarian physician David Gruby in his description of T. sanguinis, a species he discovered in frogs in 1843.[19]
Outbreaks
In Uganda, the first case of human infection was reported in 1898.[10] It was followed by an outbreak in 1900.[20] By 1901, it became severe with death toll estimated to about 20,000.[21] More than 250,000 people died in the epidemic that lasted for two decades.[20] The disease commonly popularised as "negro lethargy."[22][23] It was not known whether the human sleeping sickness and nagana were similar or the two disease were caused by similar parasites.[24] Even the observations of Forde and Dutton did not indicate that the trypanosome was related to sleeping sickness.[25]
Sleeping Sickness Commission
The Royal Society constituted a three-member Sleeping Sickness Commission on 10 May 1902 to investigate the epidemic in Uganda.[26] The Commission comprised George Carmichael Low from the London School of Hygiene and Tropical Medicine as the leader, his colleague Aldo Castellani and Cuthbert Christy, a medical officer on duty in Bombay, India.[27][28] At the time, a debate remained on the etiology, some favoured bacterial infection while some believed as helminth infection.[29] The first investigation focussed on Filaria perstans (later renamed Mansonella perstans), a small roundworm transmitted by flies, and bacteria as possible causes, only to discover that the epidemic was not related to these pathogens.[30][31] The team was described as an "ill-assorted group"[31] and a "queer lot",[32] and the expedition "a failure."[21] Low, whose conduct was described as "truculent and prone to take offence," left the Commission and Africa after three months.[33]
In February 1902, the British War Office, following a request from the Royal Society, appointed David Bruce to lead the second Sleeping Sickness Commission.[34] With David Nunes Nabarro (from the University College Hospital), Bruce and his wife joined Castellani and Christy on 16 March.[31] In November 1902, Castellani had found the trypanosomes in the cerebrospinal fluid of an infected person. He was convinced that the trypanosome was the causative parasite of sleeping sickness. Like Low, his conduct has been criticised and the Royal Society refused to publish his report. He was further infuriated when Bruce advised him not to make rash conclusion without further evidences, as there were many other parasites to consider.[26] Castellani left Africa in April and published his report as "On the discovery of a species of Trypanosoma in the cerebrospinal fluid of cases of sleeping sickness" in The Lancet.[35] By then the Royal Society had already published the report.[36] By August 1903, Bruce and his team established that the disease was transmitted the tsetse fly, Glossina palpalis.[37] However, Bruce did not understand the trypanosoma life cycle and believed that the parasites were simply transmitted from one person to another.[9]
Around the same time, Germany sent an expeditionary team led by Robert Koch to investigate the epidemic in Togo and East Africa. In 1909, one of the team members, Friedrich Karl Kleine discovered that the parasite had developmental stages in the tsetse flies.[9] Bruce, in the third Sleeping Sickness Commission (1908–1912) that included Albert Ernest Hamerton, H.R. Bateman and Frederick Percival Mackie, established the complete developmental stages of the trypanosome in tsetse fly.[38][39]
Discovery of human trypanosomes
British Colonial Surgeon Robert Michael Forde was the first to find the parasite in human. He found it from an English steamboat captain who was admitted to a hospital at Bathurst, Gambia, in 1901.[9] His report in 1902 indicates that he believed it to be a kind of filarial worm.[14] From the same person, Forde's colleague Joseph Everett Dutton identified it as a protozoan belonging to the genus Trypanosoma.[3] Knowing the distinct features, Dutton proposed a new species name in 1902:
At present then it is impossible to decide definitely as to the species, but if on further study it should be found to differ from other disease-producing trypanosomes I would suggest that it be called Trypanosoma gambiense.[40]
Another human trypanosome (now called T. brucei rhodesiense) was discovered by British parasitologists John William Watson Stephens and Harold Benjamin Fantham.[9] In 1910, Stephens noted in his experimental infection in rats that the trypanosome, obtained from an individual from Northern Rhodesia (later Zambia), was not the same as T. gambiense. The source of the parasite, an Englishman travelling in Rhodesia was found with the blood parasites in 1909, and was transported to and admitted at the Royal Southern Hospital in Liverpool under the care of Ronald Ross.[3] Fantham described the parasite's morphology and found that it was a different trypanosome.[41][42]
Species
T. brucei is a species complex that includes:
- T. brucei gambiense which causes slow onset chronic trypanosomiasis in humans. It is most common in central and western Africa, where humans are thought to be the primary reservoir.[43] In 1973, David Hurst Molyneux was the first to find infection of this strain in wildlife and domestic animals.[44][45] Since 2002, there are several reports showing that animals, including cattle, are also infected.[45] It is responsible for 98% of all human African trypanosomiasis,[46] and is roughly 100% fatal.[47]
- T. brucei rhodesiense which causes fast onset acute trypanosomiasis in humans. A highly zoonotic parasite, it is prevalent in southern and eastern Africa, where game animals and livestock are thought to be the primary reservoir.[43][46]
- T. brucei brucei which causes animal trypanosomiasis, along with several other species of Trypanosoma. T. b. brucei is not infective to humans due to its susceptibility to lysis by trypanosome lytic factor-1 (TLF-1).[48][49] However, it is closely related to, and shares fundamental features with the human-infective subspecies.[50] Only rarely can the T. b. brucei infect a human.[51]
The subspecies cannot be distinguished from their structure as they are all identical under microscopes. Geographical location is the main distinction.[46] Molecular markers have been developed for individual indentification. Serum resistance-associated (SRA) gene is used to differentiate T. b. rhodesiense from other subspecies.[52] TgsGP gene, found only in type 1 T. b. gambiense is also a specific distinction between T. b. gambiense strains.[53]
The subspecies lack many of the features commonly considered necessary to constitute monophyly.[54] As such Lukeš et al., 2022 proposes a new polyphyly by ecotype.[54]
Etymology
The genus name is derived from two Greek words: τρυπανον (trypanon or trupanon), which means "borer" or "auger", referring to the corkscrew-like movement;[55] and σῶμα (sôma), meaning "body."[56][57] The specific name is after David Bruce, who discovered the parasites in 1894.[7][8] The subspecies, the human strains, are named after the regions in Africa where they were first identified: T. brucei gambiense was described from an Englishman in Gambia in 1901; T. brucei rhodesiense was found from another Englishman in Northern Rhodesia in 1909.[3]
Structure

T. brucei is a typical unicellular eukaryotic cell, and measures 8 to 50 μm in length. It has an elongated body having a streamlined and tapered shape. Its cell membrane (called pellicle) encloses the cell organelles, including the nucleus, mitochondria, endoplasmic reticulum, Golgi apparatus, and ribosomes. In addition, there is an unusual organelle called the kinetoplast, which is a complex of thousands of mitochondria.[58] The kinetoplast lies near the basal body with which it is indistinguishable under microscope. From the basal body arises a single flagellum that run towards the anterior end. Along the body surface, the flagellum is attached to the cell membrane forming an undulating membrane. Only the tip of the flagellum is free at the anterior end.[59] The cell surface of the bloodstream form features a dense coat of variant surface glycoproteins (VSGs) which is replaced by an equally dense coat of procyclins when the parasite differentiates into the procyclic phase in the tsetse fly midgut.[60]
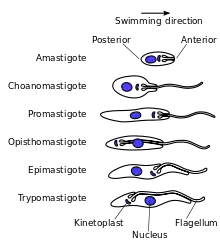
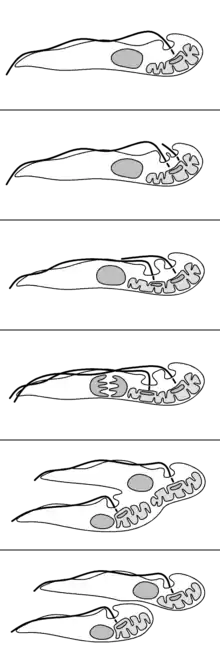
Trypanosomatids show several different classes of cellular organisation of which two are adopted by T. brucei at different stages of the life cycle:[59]
- Epimastigote, which is found in tsetse fly. Its kinetoplast and basal body lie anterior to the nucleus, with a long flagellum attached along the cell body. The flagellum starts from the centre of the body.
- Trypomastigote, which is found in mammalian hosts. The kinetoplast and basal body are posterior of nucleus. The flagellum arises from the posterior end of the body.
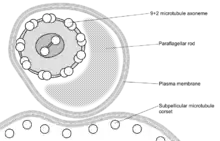
These names are derived from the Greek mastig- meaning whip, referring to the trypanosome's whip-like flagellum. The trypanosome flagellum has two main structures. It is made up of a typical flagellar axoneme, which lies parallel to the paraflagellar rod,[61] a lattice structure of proteins unique to the kinetoplastids, euglenoids and dinoflagellates.[62][63]
The microtubules of the flagellar axoneme lie in the normal 9+2 arrangement, orientated with the + at the anterior end and the − in the basal body. The cytoskeletal structure extends from the basal body to the kinetoplast. The flagellum is bound to the cytoskeleton of the main cell body by four specialised microtubules, which run parallel and in the same direction to the flagellar tubulin.[64][65]
The flagellar function is twofold — locomotion via oscillations along the attached flagellum and cell body in human blood stream and tsetse fly gut,[66][67] and attachment to the salivary gland epithelium of the fly during the epimastigote stage.[55][68] The flagellum propels the body in such a way that the axoneme generates the oscillation and a flagellar wave is created along the undulating membrane. As a result the body moves in a corkscrew pattern.[55] In flagella of other organisms, the movement starts from the base towards the tip, while in T. brucei and other trypanosomatids, the beat originates from the tip and progresses towards the base, forcing the body to move towards the direction of the tip of the flagellum.[68]
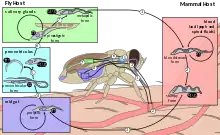
Life cycle
T. brucei completes its life cycle between tsetse fly (of the genus Glossina) and mammalian hosts, including humans, cattle, horses, and wild animals. In stressful environments, T. brucei produces exosomes containing the spliced leader RNA and uses the endosomal sorting complexes required for transport (ESCRT) system to secrete them as extracellular vesicles.[69] When absorbed by other trypanosomes these EVs cause repulsive movement away from the area and so away from bad environments.[69]
In mammalian host
Infection occurs when a vector tsetse fly bites a mammalian host. The fly injects the metacyclic trypomastigotes into the skin tissue. The trypomastigotes enter the lymphatic system and into the bloodstream. The initial trypomastigotes are short and stumpy (SS).[70] They are protected from the host's immune system by producing antigentic variation called variant surface glycoproteins on their body surface.[1] Once inside the bloodstream, they grow into long and slender forms (LS). Then, they multiply by binary fission. Some of the daughter cells then become short and stumpy again.[71][72][2] Some of them remains as intermediate forms, representing a transitional stage between the long and short forms.[46] The long slender forms are able to penetrate the blood vessel endothelium and invade extravascular tissues, including the central nervous system (CNS)[66] and placenta in pregnant women.[73]
Sometimes, wild animals can be infected by the tsetse fly and they act as reservoirs. In these animals, they do not produce the disease, but the live parasite can be transmitted back to the normal hosts.[70] Besides preparation to be taken up and vectored to another host by a tsetse fly, transition from LS to SS in the mammal serves to prolong the host's lifespan – controlling parasitemia aids in increasing the total transmitting duration of any particular infested host.[72][2]
In tsetse fly
Unlike anopheline mosquitos and sandflies that transmit other protozoan infections in which only females are involved, both sexes of tsetse flies are blood feeders and equally transmit trypanosomes.[74] The short and stumpy trypomastigotes (SS) are taken up by tsetse flies during a blood meal.[72][2] Survival in the tsetse midgut is one reason for the particular adaptations of the SS stage.[72][2] The trypomastigotes enter the midgut of the fly where they become procyclic trypomastigotes as they replace their VSG with other protein coats called procyclins.[1] Because the fly faces digestive damage from immune factors in the bloodmeal, it produces serpins to suppress the infection. The serpins including GmmSRPN3, GmmSRPN5, GmmSRPN9, and especially GmmSRPN10 are then hijacked by the parasite to aid its own midgut infection, using them to inactivate bloodmeal trypanolytic factors which would otherwise make the fly host inhospitable.[75]: 346
The procyclic trypomastigotes cross the peritrophic matrix, undergo slight elongation and migrate to the anterior part of the midgut as non-proliferative long mesocyclic trypomastigotes. As they reach the proventriculus, they became thinner and undergo cytoplasmic rearrangement to give rise to proliferative epimastigotes.[74] The epimastigotes divide asymmetrically to produce long and short epimastigotes. The long epimastigote cannot move to other places and simply die off by apoptosis.[76][77] The short epimastigote migrate from the proventriculus via the foregut and proboscis to the salivary glands where they get attached to the salivary gland epithelium.[55] Even all the short forms do not succeed in the complete migration to the salivary glands as most of them perish on the way–only up to five may survive.[74][78]
In the salivary glands, the survivors undergo phases of reproduction. The first cycle in an equal mitosis by which a mother cell produces two similar daughter epimastigotes. They remain attach to the epithelium. This phase is the main reproduction in first-stage infection to ensure sufficient number of parasites in the salivary gland.[74] The second cycle, which usually occurs in late-stage infection, involves unequal mitosis that produces two different daughter cells from the mother epimastigote. One daughter is an epimastigote that remains non-infective and the other is a trypomastigote.[79] The trypomastigote detach from the epithelium and undergo transformation into short and stumpy trypomastigotes. The surface procyclins are replaced with VSGs and become the infective metacyclic trypomastigotes.[46] Complete development in the fly takes about 20 days.[70][71] They are injected into the mammalian host along with the saliva on biting, and are known as salivarian.[74]
In the case of T. b. brucei infecting Glossina palpalis gambiensis, the parasite changes the proteome contents of the fly's head and causes behavioral changes such as unnecessarily increased feeding frequency, which increases transmission opportunities. This is related to altered glucose metabolism that causes a perceived need for more calories. (The metabolic change, in turn, being due to complete absence of glucose-6-phosphate 1-dehydrogenase in infected flies.) Monoamine neurotransmitter synthesis is also altered: production of aromatic L-amino acid decarboxylase involved in dopamine and serotonin synthesis, and α-methyldopa hypersensitive protein was induced. This is similar to the alterations in other dipteran vectors' head proteomes under infection by other eukaryotic parasites of mammals.[80]
Reproduction
Binary fission
The reproduction of T. brucei is unusual compared to most eukaryotes. The nuclear membrane remains intact and the chromosomes do not condense during mitosis. The basal body, unlike the centrosome of most eukaryotic cells, does not play a role in the organisation of the spindle and instead is involved in division of the kinetoplast. The events of reproduction are:[59]
- The basal body duplicates and both remain associated with the kinetoplast. Each basal body forms a separate flagellum.
- Kinetoplast DNA undergoes synthesis then the kinetoplast divides coupled with separation of the two basal bodies.
- Nuclear DNA undergoes synthesis while a new flagellum extends from the younger, more posterior, basal body.
- The nucleus undergoes mitosis.
- Cytokinesis progresses from the anterior to posterior.
- Division completes with abscission.
Meiosis
In the 1980s, DNA analyses of the developmental stages of T. brucei started to indicate that the trypomastigote in the tsetse fly undergoes meiosis, i.e., a sexual reproduction stage.[81] But it is not always necessary for a complete life cycle.[82] The existence of meiosis-specific proteins was reported in 2011.[83] The haploid gametes (daughter cells produced after meiosis) were discovered in 2014. The haploid trypomastigote-like gametes can interact with each other via their flagella and undergo cell fusion (the process is called syngamy).[84][85] Thus, in addition to binary fission, T. brucei can multiply by sexual reproduction. Trypanosomes belong to the supergroup Excavata and are one of the earliest diverging lineages among eukaryotes.[86] The discovery of sexual reproduction in T. brucei supports the hypothesis that meiosis and sexual reproduction are ancestral and ubiquitous features of eukaryotes.[87]
Infection and pathogenicity
The insect vectors for T. brucei are different species of tsetse fly (genus Glossina). The major vectors of T. b. gambiense, causing West African sleeping sickness, are G. palpalis, G. tachinoides, and G. fuscipes. While the principal vectors of T. b. rhodesiense, causing East African sleeping sickness, are G. morsitans, G. pallidipes, and G. swynnertoni. Animal trypanosomiasis is transmitted by a dozen species of Glossina.[88]
In later stages of a T. brucei infection of a mammalian host the parasite may migrate from the bloodstream to also infect the lymph and cerebrospinal fluids. It is under this tissue invasion that the parasites produce the sleeping sickness.[70]
In addition to the major form of transmission via the tsetse fly, T. brucei may be transferred between mammals via bodily fluid exchange, such as by blood transfusion or sexual contact, although this is thought to be rare.[89][90] Newborn babies can be infected (vertical or congenital transmission) from infected mothers.[91]
Chemotherapy
There are four drugs generally recommended for the first-line treatment of African trypanosomiasis: suramin developed in 1921, pentamidine developed in 1941, melarsoprol developed in 1949 and eflornithine developed in 1990.[92][93] These drugs ane not fully effective and are toxic to humans.[94] In addition, drug resistance has developed in the parasites against all the drugs.[95] The drugs are of limtied application since they are effective against specific strains of T. brucei and the life cycle stages of the parasites. Suram is used only for first-stage infection of T. b. rhodensiense, pentamidine for first-stage infection of T. b. gambiense, and eflornithine for second-stage infection of T. b. gambiense. Melarsopol is the only drug effective against the two types of parasite in both infection stages,[96] but is highly toxic, such that 5% of treated individuals die of brain damage (reactive encephalopathy).[97] Another drug, nifurtimox, recommended for Chagas disease (American trypanosomiasis), is itself a weak drug but in combination with melarsopol, it is used as the first-line medication against second-stage infection of T. b. gambiense.[98][99]
Historically, arsenic and mercuric compounds were introduced in the early 20th century, with success particularly in animal infections.[100][101] German physician Paul Ehrlich and his Japanese associate Kiyoshi Shiga developed the first specific trypanocidal drug in 1904 from a dye, trypan red, which they named Trypanroth.[102] These chemical preparations were effective only at high and toxic dosages, and were not suitable for clinical use.[103]
Animal trypanosomiasis is treated with six drugs: diminazene aceturate, homidium (homidium bromide and homidium chloride), isometamidium chloride, melarsomine, quinapyramine, and suramin. They are all highly toxic to animals,[104] and drug resistance is prevalent.[105] Homidium is the first prescription anti-trypanosomal drug. It was developed as a modified compound of phenantridine, which was found in 1938 to have trypanocidal activity against the bovine parasite, T. congolense.[106] Among its products, dimidium bromide and its derivatives were first used in 1948 in animal cases in Africa,[107][108][109] and became known as homidium (or as ethidium bromide in molecular biology[110]).[111][112]
Alternative therapy
Some phytochemicals have shown research promise against the T. b. brucei strain.[113] Aderbauer et al., 2008 and Umar et al., 2010 find Khaya senegalensis is effective in vitro and Ibrahim et al., 2013 and 2008 in vivo (in rats).[113] Ibrahim et al., 2013 find a lower dose reduces parasitemia by this subspecies and a higher dose is curative and prevents injury.[113]
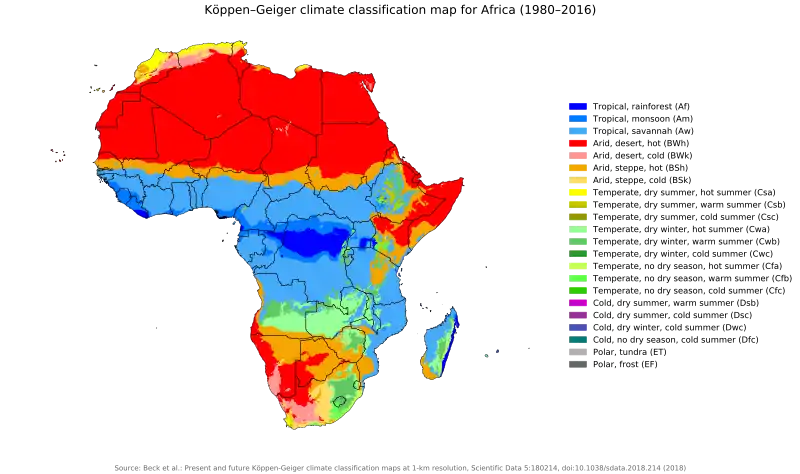
Distribution
T. brucei is found where its tsetse fly vectors are prevalent in continental Africa. That is to say, tropical rainforest (Af), tropical monsoon (Am), and tropical savannah (Aw) areas of continental Africa.[59] Hence, the equatorial region of Africa is called the "sleeping sickness" belt. However, the specific type of the trypanosome differs according to geography. T. b. rhodesiense is found primarily in East Africa (Botswana, Democratic Republic of the Congo, Ethiopia, Kenya, Malawi, Tanzania, Uganda and Zimbabwe), while T. b. gambiense is found in Central and West Africa.
Impact
T. brucei is a major cause of livestock disease in sub-Saharan Africa.[2][114] It is thus of tremendous veterinary concern and one of the greatest limitations on agriculture in Africa and the economic life of sub-Saharan Africa.[2][114]
Evolution
Trypanosoma brucei gambiense evolved from a single progenitor ~10,000 years ago.[115] It is evolving asexually and its genome shows the Meselson effect.[115]
Genetics
There are two subpopulations of T. b. gambiense that possesses two distinct groups that differ in genotype and phenotype. Group 2 is more akin to T. b. brucei than group 1 T. b. gambiense.[116]
All T. b. gambiense are resistant to killing by a serum component — trypanosome lytic factor (TLF) of which there are two types: TLF-1 and TLF-2. Group 1 T. b. gambiense parasites avoid uptake of the TLF particles while those of group 2 are able to either neutralize or compensate for the effects of TLF.[117]
In contrast, resistance in T. b. rhodesiense is dependent upon the expression of a serum resistance associated (SRA) gene.[118] This gene is not found in T. b. gambiense.[119]
Genome
The genome of T. brucei is made up of:[120]
- 11 pairs of large chromosomes of 1 to 6 megabase pairs.
- 3–5 intermediate chromosomes of 200 to 500 kilobase pairs.
- Around 100 minichromosomes of around 50 to 100 kilobase pairs. These may be present in multiple copies per haploid genome.
Most genes are held on the large chromosomes, with the minichromosomes carrying only VSG genes. The genome has been sequenced and is available on GeneDB.[121]
The mitochondrial genome is found condensed into the kinetoplast, an unusual feature unique to the kinetoplastid protozoans. The kinetoplast and the basal body of the flagellum are strongly associated via a cytoskeletal structure[122]
In 1993, a new base, ß-d-glucopyranosyloxymethyluracil (base J), was identified in the nuclear DNA of T. brucei.[123]
VSG coat
The surface of T. brucei and other species of trypanosomes is covered by a dense external coat called variant surface glycoprotein (VSG).[124] VSGs are 60-kDa proteins which are densely packed (~5 x 106 molecules) to form a 12–15 nm surface coat. VSG dimers make up about 90% of all cell surface proteins in trypanosomes. They also make up ~10% of total cell protein. For this reason, these proteins are highly immunogenic and an immune response raised against a specific VSG coat will rapidly kill trypanosomes expressing this variant. However, with each cell division there is a possibility that the progeny will switch expression to change the VSG that is being expressed.[125][126]
This VSG coat enables an infecting T. brucei population to persistently evade the host's immune system, allowing chronic infection. VSG is highly immunogenic, and an immune response raised against a specific VSG coat rapidly kills trypanosomes expressing this variant. Antibody-mediated trypanosome killing can also be observed in vitro by a complement-mediated lysis assay. However, with each cell division there is a possibility that one or both of the progeny will switch expression to change the VSG that is being expressed. The frequency of VSG switching has been measured to be approximately 0.1% per division.[127] As T. brucei populations can peak at a size of 1011 within a host[128] this rapid rate of switching ensures that the parasite population is typically highly diverse.[129][130] Because host immunity against a specific VSG does not develop immediately, some parasites will have switched to an antigenically distinct VSG variant, and can go on to multiply and continue the infection. The clinical effect of this cycle is successive 'waves' of parasitemia (trypanosomes in the blood).[124]
Expression of VSG genes occurs through a number of mechanisms yet to be fully understood.[131] The expressed VSG can be switched either by activating a different expression site (and thus changing to express the VSG in that site), or by changing the VSG gene in the active site to a different variant. The genome contains many hundreds if not thousands of VSG genes, both on minichromosomes and in repeated sections ('arrays') in the interior of the chromosomes. These are transcriptionally silent, typically with omitted sections or premature stop codons, but are important in the evolution of new VSG genes. It is estimated up to 10% of the T. brucei genome may be made up of VSG genes or pseudogenes. It is thought that any of these genes can be moved into the active site by recombination for expression.[126] VSG silencing is largely due to the effects of histone variants H3.V and H4.V. These histones cause changes in the three-dimensional structure of the T. brucei genome that results in a lack of expression. VSG genes are typically located in the subtelomeric regions of the chromosomes, which makes it easier for them to be silenced when they are not being used.[132][133] It remains unproven whether the regulation of VSG switching is purely stochastic or whether environmental stimuli affect switching frequency. Switching is linked to two factors: variation in activation of individual VSG genes; and differentiation to the "short stumpy" stage - triggered by conditions of high population density - which is the nonreproductive, interhost transmission stage.[75] As of 2021 it also remains unexplained how this transition is timed and how the next surface protein gene is chosen.[2] These questions of antigenic variation in T. brucei and other parasites are among the most interesting in the field of infection.[2]
Killing by human serum and resistance to human serum killing
Trypanosoma brucei brucei (as well as related species T. equiperdum and T. evansi) is not human infective because it is susceptible to innate immune system 'trypanolytic' factors present in the serum of some primates, including humans. These trypanolytic factors have been identified as two serum complexes designated trypanolytic factors (TLF-1 and −2) both of which contain haptoglobin related protein (HPR) and apolipoprotein LI (ApoL1). TLF-1 is a member of the high density lipoprotein family of particles while TLF-2 is a related high molecular weight serum protein binding complex.[134][135] The protein components of TLF-1 are haptoglobin related protein (HPR), apolipoprotein L-1 (apoL-1) and apolipoprotein A-1 (apoA-1). These three proteins are colocalized within spherical particles containing phospholipids and cholesterol. The protein components of TLF-2 include IgM and apolipoprotein A-I.[136]
Trypanolytic factors are found only in a few species, including humans, gorillas, mandrills, baboons and sooty mangabeys. This appears to be because haptoglobin-related protein and apolipoprotein L-1 are unique to primates. This suggests these genes originated in the primate genome 25 million years ago-35 million years ago.[137]
Human infective subspecies T. b. gambiense and T. b. rhodesiense have evolved mechanisms of resisting the trypanolytic factors, described below.
ApoL1
ApoL1 is a member of a six gene family, ApoL1-6, that have arisen by tandem duplication. These proteins are normally involved in host apoptosis or autophagic death and possess a Bcl-2 homology domain 3.[138] ApoL1 has been identified as the toxic component involved in trypanolysis.[139] ApoLs have been subject to recent selective evolution possibly related to resistance to pathogens.[140]
The gene encoding ApoL1 is found on the long arm of chromosome 22 (22q12.3). Variants of this gene, termed G1 and G2, provide protection against T. b. rhodesiense.[141] These benefits are not without their downside as a specific ApoL1 glomerulopathy has been identified.[141][142] This glomerulopathy may help to explain the greater prevalence of hypertension in African populations.[143]
The gene encodes a protein of 383 residues, including a typical signal peptide of 12 amino acids.[144] The plasma protein is a single chain polypeptide with an apparent molecular mass of 42 kiloDaltons. ApoL1 has a membrane pore forming domain functionally similar to that of bacterial colicins.[145] This domain is flanked by the membrane addressing domain and both these domains are required for parasite killing.
Within the kidney, ApoL1 is found in the podocytes in the glomeruli, the proximal tubular epithelium and the arteriolar endothelium.[146] It has a high affinity for phosphatidic acid and cardiolipin and can be induced by interferon gamma and tumor necrosis factor alpha.[147]
Hpr
Hpr is 91% identical to haptoglobin (Hp), an abundant acute phase serum protein, which possesses a high affinity for hemoglobin (Hb). When Hb is released from erythrocytes undergoing intravascular hemolysis Hp forms a complex with the Hb and these are removed from circulation by the CD163 scavenger receptor. In contrast to Hp–Hb, the Hpr–Hb complex does not bind CD163 and the Hpr serum concentration appears to be unaffected by hemolysis.[148]
Killing mechanism
The association of HPR with hemoglobin allows TLF-1 binding and uptake via the trypanosome haptoglobin-hemoglobin receptor (TbHpHbR).[149] TLF-2 enters trypanosomes independently of TbHpHbR.[149] TLF-1 uptake increases when haptoglobin level is low. TLF-1 overtakes haptoglobin and binds free hemoglobin in the serum. However the complete absence of haptoglobin is associated with a decreased killing rate by serum.[150]
The trypanosome haptoglobin-hemoglobin receptor is an elongated three a-helical bundle with a small membrane distal head.[151] This protein extends above the variant surface glycoprotein layer that surrounds the parasite.
The first step in the killing mechanism is the binding of TLF to high affinity receptors—the haptoglobin-hemoglobin receptors—that are located in the flagellar pocket of the parasite.[149][152] The bound TLF is endocytosed via coated vesicles and then trafficked to the parasite lysosomes. ApoL1 is the main lethal factor in the TLFs and kills trypanosomes after insertion into endosomal / lysosomal membranes.[139] After ingestion by the parasite, the TLF-1 particle is trafficked to the lysosome wherein ApoL1 is activated by a pH mediated conformational change. After fusion with the lysosome the pH drops from ~7 to ~5. This induces a conformational change in the ApoL1 membrane addressing domain which in turn causes a salt bridge linked hinge to open. This releases ApoL1 from the HDL particle to insert in the lysosomal membrane. The ApoL1 protein then creates anionic pores in the membrane which leads to depolarization of the membrane, a continuous influx of chloride and subsequent osmotic swelling of the lysosome. This influx in its turn leads to rupture of the lysosome and the subsequent death of the parasite.[153]
Resistance mechanisms: T. b. gambiense
Trypanosoma brucei gambiense causes 97% of human cases of sleeping sickness. Resistance to ApoL1 is principally mediated by the hydrophobic β-sheet of the T. b. gambiense specific glycoprotein.[154] Other factors involved in resistance appear to be a change in the cysteine protease activity and TbHpHbR inactivation due to a leucine to serine substitution (L210S) at codon 210.[154] This is due to a thymidine to cytosine mutation at the second codon position.[155]
These mutations may have evolved due to the coexistence of malaria where this parasite is found.[154] Haptoglobin levels are low in malaria because of the hemolysis that occurs with the release of the merozoites into the blood. The rupture of the erythrocytes results in the release of free haem into the blood where it is bound by haptoglobin. The haem is then removed along with the bound haptoglobin from the blood by the reticuloendothelial system.[156]
Resistance mechanisms: T. b. rhodesiense
Trypanosoma brucei rhodesiense relies on a different mechanism of resistance: the serum resistance associated protein (SRA). The SRA gene is a truncated version of the major and variable surface antigen of the parasite, the variant surface glycoprotein.[157] However, it has little similarity (low sequence homology) with the VSG gene (<25%). SRA is an expression site associated gene in T. b. rhodesiense and is located upstream of the VSGs in the active telomeric expression site.[158] The protein is largely localized to small cytoplasmic vesicles between the flagellar pocket and the nucleus. In T. b. rhodesiense the TLF is directed to SRA containing endosomes while some dispute remains as to its presence in the lysosome.[139][159] SRA binds to ApoL1 using a coiled–coiled interaction at the ApoL1 SRA interacting domain while within the trypanosome lysosome.[139] This interaction prevents the release of the ApoL1 protein and the subsequent lysis of the lysosome and death of the parasite.
Baboons are known to be resistant to T. b. rhodesiense. The baboon version of the ApoL1 gene differs from the human gene in a number of respects including two critical lysines near the C terminus that are necessary and sufficient to prevent baboon ApoL1 binding to SRA.[160] Experimental mutations allowing ApoL1 to be protected from neutralization by SRA have been shown capable of conferring trypanolytic activity on T. b. rhodesiense.[118] These mutations resemble those found in baboons, but also resemble natural mutations conferring protection of humans against T. b. rhodesiense which are linked to kidney disease.[141]
See also
- List of parasites (human)
- Simon Gaskell, professor of chemistry and current principal of Queen Mary, University of London, researches various forms of mass spectrometry to determine the quantity and longevity of these proteins.
- Tryptophol, a chemical compound produced by the T. brucei which induces sleep in humans[161]
References
- Romero-Meza, Gabriela; Mugnier, Monica R. (2020). "Trypanosoma brucei". Trends in Parasitology. 36 (6): 571–572. doi:10.1016/j.pt.2019.10.007. PMC 7375462. PMID 31757771.
- Luzak V, López-Escobar L, Siegel TN, Figueiredo LM (October 2021). "Cell-to-Cell Heterogeneity in Trypanosomes". Annual Review of Microbiology. Annual Reviews. 75 (1): 107–128. doi:10.1146/annurev-micro-040821-012953. PMID 34228491. S2CID 235759288.
- Baker JR (March 1995). "The subspecific taxonomy of Trypanosoma brucei". Parasite. 2 (1): 3–12. doi:10.1051/parasite/1995021003. PMID 9137639.

- Masocha W, Kristensson K (2012). "Passage of parasites across the blood-brain barrier". Virulence. 3 (2): 202–212. doi:10.4161/viru.19178. PMC 3396699. PMID 22460639.
- Legros D, Ollivier G, Gastellu-Etchegorry M, Paquet C, Burri C, Jannin J, Büscher P (July 2002). "Treatment of human African trypanosomiasis--present situation and needs for research and development". The Lancet. Infectious Diseases. 2 (7): 437–440. doi:10.1016/S1473-3099(02)00321-3. hdl:10144/18268. PMID 12127356.
- Gibson W (July 2007). "Resolution of the species problem in African trypanosomes". International Journal for Parasitology. 37 (8–9): 829–838. doi:10.1016/j.ijpara.2007.03.002. PMID 17451719.
- Joubert JJ, Schutte CH, Irons DJ, Fripp PJ (1993). "Ubombo and the site of David Bruce's discovery of Trypanosoma brucei". Transactions of the Royal Society of Tropical Medicine and Hygiene. 87 (4): 494–495. doi:10.1016/0035-9203(93)90056-v. PMID 8249096.
- Cook GC (1994). "Sir David Bruce's elucidation of the aetiology of nagana--exactly one hundred years ago". Transactions of the Royal Society of Tropical Medicine and Hygiene. 88 (3): 257–258. doi:10.1016/0035-9203(94)90068-x. PMID 7974656.
- Steverding D (February 2008). "The history of African trypanosomiasis". Parasites & Vectors. 1 (1): 3. doi:10.1186/1756-3305-1-3. PMC 2270819. PMID 18275594.
- Berrang-Ford L, Odiit M, Maiso F, Waltner-Toews D, McDermott J (December 2006). "Sleeping sickness in Uganda: revisiting current and historical distributions". African Health Sciences. 6 (4): 223–231. PMC 1832067. PMID 17604511.
- Mullen GR, Durden LA (2009). Medical and Veterinary Entomology (2 ed.). Academic Press. p. 297. ISBN 978-0-08-091969-0.
- Bruce D (1895). Preliminary Report on the Tsetse Fly Disease or Nagana, in Zululand. Durban (South Africa): Bennett & Davis. p. 1.
- Kennedy PG (February 2004). "Human African trypanosomiasis of the CNS: current issues and challenges". The Journal of Clinical Investigation. 113 (4): 496–504. doi:10.1172/JCI34802. PMC 2214720.
- Cox FE (June 2004). "History of sleeping sickness (African trypanosomiasis)". Infectious Disease Clinics of North America. 18 (2): 231–245. doi:10.1016/j.idc.2004.01.004. PMID 15145378.
- Ormerod WE (October 1991). "Hypothesis: the significance of Winterbottom's sign". The Journal of Tropical Medicine and Hygiene. 94 (5): 338–340. PMID 1942213.
- Cook GC (2007). Tropical Medicine: An Illustrated History of The Pioneers. Burlington (US): Elsevier Ltd. pp. 145–156. ISBN 978-0-08-055939-1.
- Ellis H (March 2006). "Sir David Bruce, a pioneer of tropical medicine". British Journal of Hospital Medicine. 67 (3): 158. doi:10.12968/hmed.2006.67.3.20624. PMID 16562450.
- Martini E (1903). "Ueber die Entwickelung der Tsetseparasiten in Säugethieren" [Preliminary note on the morphology and distribution of the parasite found in tsetse disease]. Zeitschrift für Hygiene und Infektionskrankheiten (in German). 42 (1): 341–351. doi:10.1007/BF02217469. S2CID 12816407.
- Novy FG (1907). "Trypanosomes". Journal of the American Medical Association. XLVIII (1): 1–10. doi:10.1001/jama.1907.25220270001001.
- Fèvre EM, Coleman PG, Welburn SC, Maudlin I (April 2004). "Reanalyzing the 1900-1920 sleeping sickness epidemic in Uganda". Emerging Infectious Diseases. 10 (4): 567–573. doi:10.3201/eid1004.020626. PMID 15200843.
- Cook G (2007). Tropical Medicine: An Illustrated History of The Pioneers. London: Elsevier. pp. 133–135. ISBN 978-0-08-055939-1.
- Mott FW (December 1899). "The Changes in the Central Nervous System of Two Cases of Negro Lethargy: Sequel to Dr. Manson's Clinical Report". British Medical Journal. 2 (2033): 1666–1669. doi:10.1136/bmj.2.2033.1666. PMC 2412509. PMID 20758763.
- Cook GC (January 1996). "The 'Negro lethargy' in Uganda". Parasitology Today. 12 (1): 41. doi:10.1016/0169-4758(96)90083-6. PMID 15275309.
- Castellani A (1903). "The history of the association of Trypanosoma with sleeping sickness". British Medical Journal. 2 (2241): 1565. doi:10.1136/bmj.2.2241.1565-a. PMC 2514975.
- Köhler W, Köhler M (September 2002). "Zentralblatt für Bakteriologie--100 years ago: sleeping sickness--intoxication or infectious disease?". International Journal of Medical Microbiology. 292 (3–4): 141–147. doi:10.1078/1438-4221-00190. PMID 12398205.
- Boyd J (June 1973). "Sleeping sickness. The Castellani-Bruce controversy". Notes and Records of the Royal Society of London. 28: 93–110. doi:10.1098/rsnr.1973.0008. PMID 11615538. S2CID 37631020.
- Cook GC (January 1993). "George Carmichael Low FRCP: an underrated figure in British tropical medicine". Journal of the Royal College of Physicians of London. 27 (1): 81–82. PMC 5396591. PMID 8426352.
- Cook GC (1993). "Royal Society of Tropical Medicine and Hygiene meeting at Manson House, London, 10 December 1992. George Carmichael Low FRCP: twelfth president of the Society and underrated pioneer of tropical medicine". Transactions of the Royal Society of Tropical Medicine and Hygiene. 87 (4): 355–360. doi:10.1016/0035-9203(93)90002-8. PMID 8249057.
- Amaral I (December 2012). "Bacteria or parasite? the controversy over the etiology of sleeping sickness and the Portuguese participation, 1898-1904". Historia, Ciencias, Saude--Manguinhos. 19 (4): 1275–1300. doi:10.1590/s0104-59702012005000004. PMID 23184240.
- Cook GC (May 2012). "Patrick Manson (1844-1922) FRS: Filaria (Mansonella) perstans and sleeping sickness (African trypanosomiasis)". Journal of Medical Biography. 20 (2): 69. doi:10.1258/jmb.2010.010051. PMID 22791871. S2CID 33661530.
- Lumsden WH (August 1974). "Some episodes in the history of African trypanosomiasis". Proceedings of the Royal Society of Medicine. 67 (8): 789–796. doi:10.1177/003591577406700846. PMC 1645813. PMID 4607392.
- Wiggins CA (November 1960). "Early days in East Africa and Uganda". East African Medical Journal. 37: 699–708 contd. PMID 13785176.
- Davies JN (March 1962). "The cause of sleeping-sickness? Entebbe 1902-03. I". East African Medical Journal. 39: 81–99. PMID 13883839.
- J.R. B. (1932). "Sir David Bruce. 1855-1931". Obituary Notices of Fellows of the Royal Society. 1 (1): 79–85. doi:10.1098/rsbm.1932.0017. ISSN 1479-571X. JSTOR 768965.
- Castellani A (1903). "On the discovery of a species of trypanosoma in the cerebrospinal fluid of cases of sleeping sickness". The Lancet. 161 (4164): 1735–1736. doi:10.1016/S0140-6736(01)70338-8.
- Castellani A (1903). "On the discovery of a species of trypanosoma in the cerebrospinal fluid of cases of sleeping sickness". Proceedings of the Royal Society of London. 71 (467–476): 501–508. doi:10.1098/rspl.1902.0134. S2CID 59110369.
- Welburn SC, Maudlin I, Simarro PP (December 2009). "Controlling sleeping sickness - a review" (PDF). Parasitology. 136 (14): 1943–1949. doi:10.1017/S0031182009006416. PMID 19691861. S2CID 41052902.
- Bruce D, Hamerton AE, Bateman HR, Mackie FP (1909). "The development of Trypanosoma gambiense in Glossina palpalis". Proceedings of the Royal Society of London. Series B. 81 (550): 405–414. doi:10.1098/rspb.1909.0041.
- Bruce D, Hamerton AE, Bateman HR, Mackie FP (1911). "Further researches on the development of Trypanosoma gambiense in Glossina palpalis". Proceedings of the Royal Society of London. Series B. 83 (567): 513–527. doi:10.1098/rspb.1911.0034.
- Dutton JE (1902). "Preliminary note upon a trypanosome occurring in the blood of man". Wellcome Collection. Retrieved 21 March 2021.
{{cite web}}: CS1 maint: url-status (link) - Stephens JW, Fantham HB, Ross R (1910). "On the peculiar morphology of a trypanosome from a case of sleeping sickness and the possibility of its being a new species (T. rhodesiense)". Proceedings of the Royal Society of London. Series B. 83 (561): 28–33. doi:10.1098/rspb.1910.0064.
- Stephens JW, Fantham HB (1910). "On the Peculiar Morphology of a Trypanosome From a Case of Sleeping Sickness and the Possibility of Its Being a New Species (T. Rhodesiense)". Annals of Tropical Medicine & Parasitology. 4 (3): 343–350. doi:10.1080/00034983.1910.11685723.
- Barrett MP, Burchmore RJ, Stich A, Lazzari JO, Frasch AC, Cazzulo JJ, Krishna S (November 2003). "The trypanosomiases". Lancet. 362 (9394): 1469–1480. doi:10.1016/S0140-6736(03)14694-6. PMID 14602444. S2CID 7917540.
- Molyneux DH (1973). "Animal reservoirs and Gambian trypanosomiasis". Annales de la Société Belge de Médecine Tropicale. 53 (6): 605–618. PMID 4204667.
- Büscher P, Cecchi G, Jamonneau V, Priotto G (November 2017). "Human African trypanosomiasis". Lancet. 390 (10110): 2397–2409. doi:10.1016/S0140-6736(17)31510-6. PMID 28673422. S2CID 4853616.
- Franco, Jose R; Simarro, Pere P; Diarra, Abdoulaye; Jannin, Jean G (2014). "Epidemiology of human African trypanosomiasis". Clinical Epidemiology. 6: 257–275. doi:10.2147/CLEP.S39728. ISSN 1179-1349. PMC 4130665. PMID 25125985.
- Jamonneau, Vincent; Ilboudo, Hamidou; Kaboré, Jacques; Kaba, Dramane; Koffi, Mathurin; Solano, Philippe; Garcia, André; Courtin, David; Laveissière, Claude; Lingue, Kouakou; Büscher, Philippe; Bucheton, Bruno (2012). "Untreated human infections by Trypanosoma brucei gambiense are not 100% fatal". PLOS Neglected Tropical Diseases. 6 (6): e1691. doi:10.1371/journal.pntd.0001691. ISSN 1935-2735. PMC 3373650. PMID 22720107.
- Stephens NA, Kieft R, Macleod A, Hajduk SL (December 2012). "Trypanosome resistance to human innate immunity: targeting Achilles' heel". Trends in Parasitology. 28 (12): 539–545. doi:10.1016/j.pt.2012.09.002. PMC 4687903. PMID 23059119.
- Rifkin MR (August 1984). "Trypanosoma brucei: biochemical and morphological studies of cytotoxicity caused by normal human serum". Experimental Parasitology. Elsevier. 58 (1): 81–93. doi:10.1016/0014-4894(84)90023-7. PMID 6745390.
- Balmer O, Beadell JS, Gibson W, Caccone A (February 2011). "Phylogeography and taxonomy of Trypanosoma brucei". PLOS Neglected Tropical Diseases. 5 (2): e961. doi:10.1371/journal.pntd.0000961. PMC 3035665. PMID 21347445.
- Deborggraeve S, Koffi M, Jamonneau V, Bonsu FA, Queyson R, Simarro PP, et al. (August 2008). "Molecular analysis of archived blood slides reveals an atypical human Trypanosoma infection". Diagnostic Microbiology and Infectious Disease. 61 (4): 428–433. doi:10.1016/j.diagmicrobio.2008.03.006. PMID 18455900.
- Radwanska, Magdalena; Chamekh, Mustapha; Vanhamme, Luc; Claes, Filip; Magez, Stefan; Magnus, Eddy; de Baetselier, Patrick; Büscher, Philippe; Pays, Etienne (2002). "The serum resistance-associated gene as a diagnostic tool for the detection of Trypanosoma brucei rhodesiense". The American Journal of Tropical Medicine and Hygiene. 67 (6): 684–690. doi:10.4269/ajtmh.2002.67.684. ISSN 0002-9637. PMID 12518862. S2CID 3232109.
- Felu, Cecile; Pasture, Julie; Pays, Etienne; Pérez-Morga, David (2007). "Diagnostic potential of a conserved genomic rearrangement in the Trypanosoma brucei gambiense-specific TGSGP locus". The American Journal of Tropical Medicine and Hygiene. 76 (5): 922–929. doi:10.4269/ajtmh.2007.76.922. ISSN 0002-9637. PMID 17488917.
- Lukeš, Julius; Kachale, Ambar; Votýpka, Jan; Butenko, Anzhelika; Field, Mark (2022). "African trypanosome strategies for conquering new hosts and territories: the end of monophyly?". Trends in Parasitology. Cell Press. 38 (9): 724–736. doi:10.1016/j.pt.2022.05.011. ISSN 1471-4922.
- Krüger T, Schuster S, Engstler M (December 2018). "Beyond Blood: African Trypanosomes on the Move". Trends in Parasitology. 34 (12): 1056–1067. doi:10.1016/j.pt.2018.08.002. PMID 30181072. S2CID 52154369.
- "Etymologia: Trypanosoma". Emerging Infectious Diseases. 12 (9): 1473. 2006. doi:10.3201/eid1209.ET1209. ISSN 1080-6040. PMC 3293449.
- Morriswood, Brooke (2015). "Form, Fabric, and Function of a Flagellum-Associated Cytoskeletal Structure". Cells. 4 (4): 726–747. doi:10.3390/cells4040726. ISSN 2073-4409. PMC 4695855. PMID 26540076.
- Amodeo S, Jakob M, Ochsenreiter T (April 2018). "Characterization of the novel mitochondrial genome replication factor MiRF172 in Trypanosoma brucei". Journal of Cell Science. The Company of Biologists. 131 (8): jcs211730. doi:10.1242/jcs.211730. PMC 5963845. PMID 29626111.
- "African animal trypanosomes". Food and Agricultural Organization. Retrieved 28 January 2016.
- Romero-Meza G, Mugnier MR (June 2020). "Trypanosoma brucei". Trends in Parasitology. 36 (6): 571–572. doi:10.1016/j.pt.2019.10.007. PMC 7375462. PMID 31757771.
- Koyfman AY, Schmid MF, Gheiratmand L, Fu CJ, Khant HA, Huang D, et al. (July 2011). "Structure of Trypanosoma brucei flagellum accounts for its bihelical motion". Proceedings of the National Academy of Sciences of the United States of America. 108 (27): 11105–11108. Bibcode:2011PNAS..10811105K. doi:10.1073/pnas.1103634108. PMC 3131312. PMID 21690369.
- v (1988). "The paraflagellar rod: a structure in search of a function". Biology of the Cell. 63 (2): 169–181. doi:10.1016/0248-4900(88)90056-1. ISSN 0248-4900. S2CID 86009836.
- Bastin P, Matthews KR, Gull K (August 1996). "The paraflagellar rod of kinetoplastida: solved and unsolved questions". Parasitology Today. 12 (8): 302–307. doi:10.1016/0169-4758(96)10031-4. PMID 15275181.
- Sunter JD, Gull K (April 2016). "The Flagellum Attachment Zone: 'The Cellular Ruler' of Trypanosome Morphology". Trends in Parasitology. Cell Press. 32 (4): 309–324. doi:10.1016/j.pt.2015.12.010. PMC 4827413. PMID 26776656. S2CID 1080165.
- Woods A, Sherwin T, Sasse R, MacRae TH, Baines AJ, Gull K (July 1989). "Definition of individual components within the cytoskeleton of Trypanosoma brucei by a library of monoclonal antibodies". Journal of Cell Science. 93 ( Pt 3) (3): 491–500. doi:10.1242/jcs.93.3.491. PMID 2606940.
- Langousis G, Hill KL (July 2014). "Motility and more: the flagellum of Trypanosoma brucei". Nature Reviews. Microbiology. 12 (7): 505–518. doi:10.1038/nrmicro3274. PMC 4278896. PMID 24931043.
- Halliday C, de Castro-Neto A, Alcantara CL, Cunha-E-Silva NL, Vaughan S, Sunter JD (April 2021). "Trypanosomatid Flagellar Pocket from Structure to Function". Trends in Parasitology. 37 (4): 317–329. doi:10.1016/j.pt.2020.11.005. PMID 33308952. S2CID 229179306.
- Ralston KS, Kabututu ZP, Melehani JH, Oberholzer M, Hill KL (2009). "The Trypanosoma brucei flagellum: moving parasites in new directions". Annual Review of Microbiology. 63: 335–362. doi:10.1146/annurev.micro.091208.073353. PMC 3821760. PMID 19575562.
- Juan T, Fürthauer M (February 2018). "Biogenesis and function of ESCRT-dependent extracellular vesicles". Seminars in Cell & Developmental Biology. Elsevier. 74: 66–77. doi:10.1016/j.semcdb.2017.08.022. PMID 28807885.
- Chatterjee KD (2009). Parasitology (Protozoology and Helminthology) in relation to clinical medicine (13 ed.). New Delhi: CBC Publishers. pp. 56–57. ISBN 978-8-12-39-1810-5.
- "Parasites - African Trypanosomiasis (also known as Sleeping Sickness)". Centers for Disease Control and Prevention. Retrieved 29 January 2016.
- Seed JR, Wenck MA (June 2003). "Role of the long slender to short stumpy transition in the life cycle of the african trypanosomes". Kinetoplastid Biology and Disease. BioMed Central. 2 (1): 3. doi:10.1186/1475-9292-2-3. PMC 165594. PMID 12844365.
- McClure, Elizabeth M.; Goldenberg, Robert L. (2009). "Infection and stillbirth". Seminars in Fetal & Neonatal Medicine. 14 (4): 182–189. doi:10.1016/j.siny.2009.02.003. ISSN 1878-0946. PMC 3962114. PMID 19285457.
- Rotureau, Brice; Van Den Abbeele, Jan (2013). "Through the dark continent: African trypanosome development in the tsetse fly". Frontiers in Cellular and Infection Microbiology. 3: 53. doi:10.3389/fcimb.2013.00053. ISSN 2235-2988. PMC 3776139. PMID 24066283.
- Mideo N, Acosta-Serrano A, Aebischer T, Brown MJ, Fenton A, Friman VP, et al. (January 2013). "Life in cells, hosts, and vectors: parasite evolution across scales". Infection, Genetics and Evolution. 13: 344–347. doi:10.1016/j.meegid.2012.03.016. PMID 22465537. (VPF ORCID 0000-0002-1592-157X).
- Proto, William R.; Coombs, Graham H.; Mottram, Jeremy C. (2013). "Cell death in parasitic protozoa: regulated or incidental?". Nature Reviews. Microbiology. 11 (1): 58–66. doi:10.1038/nrmicro2929. ISSN 1740-1534. PMID 23202528. S2CID 1633550.
- Van Den Abbeele, J.; Claes, Y.; van Bockstaele, D.; Le Ray, D.; Coosemans, M. (1999). "Trypanosoma brucei spp. development in the tsetse fly: characterization of the post-mesocyclic stages in the foregut and proboscis". Parasitology. 118 ( Pt 5) (5): 469–478. doi:10.1017/s0031182099004217. ISSN 0031-1820. PMID 10363280. S2CID 32217938.
- Oberle, Michael; Balmer, Oliver; Brun, Reto; Roditi, Isabel (2010). "Bottlenecks and the maintenance of minor genotypes during the life cycle of Trypanosoma brucei". PLOS Pathogens. 6 (7): e1001023. doi:10.1371/journal.ppat.1001023. ISSN 1553-7374. PMC 2912391. PMID 20686656.
- Rotureau, Brice; Subota, Ines; Buisson, Johanna; Bastin, Philippe (2012). "A new asymmetric division contributes to the continuous production of infective trypanosomes in the tsetse fly". Development. 139 (10): 1842–1850. doi:10.1242/dev.072611. ISSN 1477-9129. PMID 22491946. S2CID 7068417.
- Lefèvre T, Thomas F, Ravel S, Patrel D, Renault L, Le Bourligu L, et al. (December 2007). "Trypanosoma brucei brucei induces alteration in the head proteome of the tsetse fly vector Glossina palpalis gambiensis". Insect Molecular Biology. Royal Entomological Society (Wiley). 16 (6): 651–660. doi:10.1111/j.1365-2583.2007.00761.x. PMID 18092995. S2CID 3134104.
- Zampetti-Bosseler F, Schweizer J, Pays E, Jenni L, Steinert M (August 1986). "Evidence for haploidy in metacyclic forms of Trypanosoma brucei". Proceedings of the National Academy of Sciences of the United States of America. 83 (16): 6063–6064. Bibcode:1986PNAS...83.6063Z. doi:10.1073/pnas.83.16.6063. PMC 386438. PMID 3461475.
- Jenni L (1990). "Sexual stages in trypanosomes and implications". Annales de Parasitologie Humaine et Comparée. 65 (Suppl 1): 19–21. doi:10.1051/parasite/1990651019. PMID 2264676.
- Peacock L, Ferris V, Sharma R, Sunter J, Bailey M, Carrington M, Gibson W (March 2011). "Identification of the meiotic life cycle stage of Trypanosoma brucei in the tsetse fly". Proceedings of the National Academy of Sciences of the United States of America. 108 (9): 3671–3676. Bibcode:2011PNAS..108.3671P. doi:10.1073/pnas.1019423108. PMC 3048101. PMID 21321215.
- Peacock L, Bailey M, Carrington M, Gibson W (January 2014). "Meiosis and haploid gametes in the pathogen Trypanosoma brucei". Current Biology. 24 (2): 181–186. doi:10.1016/j.cub.2013.11.044. PMC 3928991. PMID 24388851.
- Peacock L, Ferris V, Bailey M, Gibson W (February 2014). "Mating compatibility in the parasitic protist Trypanosoma brucei". Parasites & Vectors. 7 (1): 78. doi:10.1186/1756-3305-7-78. PMC 3936861. PMID 24559099.
- Hampl V, Hug L, Leigh JW, Dacks JB, Lang BF, Simpson AG, Roger AJ (March 2009). "Phylogenomic analyses support the monophyly of Excavata and resolve relationships among eukaryotic "supergroups"". Proceedings of the National Academy of Sciences of the United States of America. 106 (10): 3859–3864. Bibcode:2009PNAS..106.3859H. doi:10.1073/pnas.0807880106. PMC 2656170. PMID 19237557.
- Malik SB, Pightling AW, Stefaniak LM, Schurko AM, Logsdon JM (August 2007). "An expanded inventory of conserved meiotic genes provides evidence for sex in Trichomonas vaginalis". PLOS ONE. 3 (8): e2879. Bibcode:2008PLoSO...3.2879M. doi:10.1371/journal.pone.0002879. PMC 2488364. PMID 18663385.
- Krisnky WL (2009). "Tsetse fly (Glossinidae)". In Mullen GR, Durden L (eds.). Medical and Veterinary Entomology (2 ed.). Amsterdam: Elsevier. p. 296. ISBN 978-0-0-80-91969-0.
- "African Trypanosomes: epidemiology and risk factors". Centers for Disease Control. 2 May 2017.
- Rocha G, Martins A, Gama G, Brandão F, Atouguia J (January 2004). "Possible cases of sexual and congenital transmission of sleeping sickness". Lancet. 363 (9404): 247. doi:10.1016/S0140-6736(03)15345-7. PMID 14738812. S2CID 5311361.
- Lindner, Andreas K.; Priotto, Gerardo (2010). "The unknown risk of vertical transmission in sleeping sickness--a literature review". PLOS Neglected Tropical Diseases. 4 (12): e783. doi:10.1371/journal.pntd.0000783. ISSN 1935-2735. PMC 3006128. PMID 21200416.
- Nok AJ (May 2003). "Arsenicals (melarsoprol), pentamidine and suramin in the treatment of human African trypanosomiasis". Parasitology Research. 90 (1): 71–79. doi:10.1007/s00436-002-0799-9. PMID 12743807. S2CID 35019516.
- Burri C, Brun R (June 2003). "Eflornithine for the treatment of human African trypanosomiasis". Parasitology Research. 90 Supp 1: S49–S52. doi:10.1007/s00436-002-0766-5. PMID 12811548. S2CID 35509112.
- Docampo R, Moreno SN (June 2003). "Current chemotherapy of human African trypanosomiasis". Parasitology Research. 90 Supp 1: S10–S13. doi:10.1007/s00436-002-0752-y. PMID 12811544. S2CID 21917230.
- Barrett MP, Vincent IM, Burchmore RJ, Kazibwe AJ, Matovu E (September 2011). "Drug resistance in human African trypanosomiasis". Future Microbiology. 6 (9): 1037–1047. doi:10.2217/fmb.11.88. PMID 21958143.
- Babokhov P, Sanyaolu AO, Oyibo WA, Fagbenro-Beyioku AF, Iriemenam NC (July 2013). "A current analysis of chemotherapy strategies for the treatment of human African trypanosomiasis". Pathogens and Global Health. 107 (5): 242–252. doi:10.1179/2047773213Y.0000000105. PMC 4001453. PMID 23916333.
- Kennedy PG (February 2013). "Clinical features, diagnosis, and treatment of human African trypanosomiasis (sleeping sickness)". The Lancet. Neurology. 12 (2): 186–194. doi:10.1016/S1474-4422(12)70296-X. PMID 23260189. S2CID 8688394.
- Lutje V, Seixas J, Kennedy A (June 2013). "Chemotherapy for second-stage human African trypanosomiasis". The Cochrane Database of Systematic Reviews (6): CD006201. doi:10.1002/14651858.CD006201.pub3. PMC 6532745. PMID 23807762.
- Bottieau E, Clerinx J (March 2019). "Human African Trypanosomiasis: Progress and Stagnation". Infectious Disease Clinics of North America. 33 (1): 61–77. doi:10.1016/j.idc.2018.10.003. PMID 30712768. S2CID 73432597.
- Thomas HW (May 1905). "Some Experiments in the Treatment of Trypanosomiasis". British Medical Journal. 1 (2317): 1140–1143. doi:10.1136/bmj.1.2317.1140. PMC 2320665. PMID 20762118.
- Moore B, Nierenstein M, Todd JL (1907). "On the Treatment of Trypanosomiasis by Atoxyl (an Organic Arsenical Compound), followed by a Mercuric Salt (Mercuric Chloride) being a Bio-Chemical Study of the Reaction of a Parasitic Protozoon to Different Chemical Reagents at Different Stages of its Life History". The Biochemical Journal. 2 (5–6): 300–324. doi:10.1042/bj0020300. PMC 1276215. PMID 16742071.
- Wenyon CM (April 1907). "Action of the Colours of Benzidine on Mice Infected with Trypanosoma dimorphon". The Journal of Hygiene. 7 (2): 273–290. doi:10.1017/s0022172400033295. PMC 2236235. PMID 20474312.
- Nocht B (1935). "Present state of knowledge of chemotherapy". Chinese Medical Journal. 49 (5): 479–489.
- Giordani F, Morrison LJ, Rowan TG, DE Koning HP, Barrett MP (December 2016). "The animal trypanosomiases and their chemotherapy: a review". Parasitology. 143 (14): 1862–1889. doi:10.1017/S0031182016001268. PMC 5142301. PMID 27719692.
- Kasozi KI, MacLeod ET, Waiswa C, Mahero M, Ntulume I, Welburn SC (August 2022). "Systematic Review and Meta-Analysis on Knowledge Attitude and Practices on African Animal Trypanocide Resistance". Tropical Medicine and Infectious Disease. 7 (9): 205. doi:10.3390/tropicalmed7090205. PMC 9503918. PMID 36136616.
- Walls LP (1947). "The chemotherapy of phenanthridine compounds". Journal of the Society of Chemical Industry. 66 (6): 182–187. doi:10.1002/jctb.5000660604.
- Wilson SG (April 1948). "Further observations on the curative value of dimidium bromide in Trypanosoma congolense infections in bovines in Uganda". The Journal of Comparative Pathology and Therapeutics. 58 (2): 94–106. doi:10.1016/s0368-1742(48)80008-1. PMID 18861668.
- Wilson SG (1948). "Further Observations on the Curative Value of Dimidium Bromide (Phenanthridinium 1553) in Trypanosoma Congolense Infections in Bovines in Uganda". Journal of Comparative Pathology and Therapeutics. 58 (2): 94–106. doi:10.1016/S0368-1742(48)80008-1. PMID 18861668.
- Carmichael J (April 1950). "Dimidium bromide or phenanthridinium 1553; a note on the present position". The Veterinary Record. 62 (17): 257. doi:10.1136/vr.62.17.257-a. PMID 15418753. S2CID 33016283.
- Lai JS, Herr W (August 1992). "Ethidium bromide provides a simple tool for identifying genuine DNA-independent protein associations". Proceedings of the National Academy of Sciences of the United States of America. 89 (15): 6958–6962. Bibcode:1992PNAS...89.6958L. doi:10.1073/pnas.89.15.6958. PMC 49624. PMID 1495986.
- Elslager EF, Thompson PE (1962). "Parasite Chemotherapy". Annual Review of Pharmacology. 2 (1): 193–214. doi:10.1146/annurev.pa.02.040162.001205. ISSN 0066-4251.
- Kasozi KI, MacLeod ET, Ntulume I, Welburn SC (2022). "An Update on African Trypanocide Pharmaceutics and Resistance". Frontiers in Veterinary Science. 9: 828111. doi:10.3389/fvets.2022.828111. PMC 8959112. PMID 35356785.
- Ibrahim MA, Mohammed A, Isah MB, Aliyu AB (May 2014). "Anti-trypanosomal activity of African medicinal plants: a review update". Journal of Ethnopharmacology. International Society of Ethnopharmacology (Elsevier). 154 (1): 26–54. doi:10.1016/j.jep.2014.04.012. PMID 24742753.
- Auty H, Torr SJ, Michoel T, Jayaraman S, Morrison LJ (August 2015). "Cattle trypanosomosis: the diversity of trypanosomes and implications for disease epidemiology and control". Revue Scientifique et Technique. O.I.E (World Organisation for Animal Health). 34 (2): 587–598. doi:10.20506/rst.34.2.2382. PMID 26601459. S2CID 42700199.
- Weir W, Capewell P, Foth B, Clucas C, Pountain A, Steketee P, et al. (January 2016). "Population genomics reveals the origin and asexual evolution of human infective trypanosomes". eLife. 5: e11473. doi:10.7554/eLife.11473. PMC 4739771. PMID 26809473.
- Paindavoine P, Pays E, Laurent M, Geltmeyer Y, Le Ray D, Mehlitz D, Steinert M (February 1986). "The use of DNA hybridization and numerical taxonomy in determining relationships between Trypanosoma brucei stocks and subspecies". Parasitology. 92 (Pt 1): 31–50. doi:10.1017/S0031182000063435. PMID 3960593. S2CID 33529173.
- Capewell P, Veitch NJ, Turner CM, Raper J, Berriman M, Hajduk SL, MacLeod A (September 2011). "Differences between Trypanosoma brucei gambiense groups 1 and 2 in their resistance to killing by trypanolytic factor 1". PLOS Neglected Tropical Diseases. 5 (9): e1287. doi:10.1371/journal.pntd.0001287. PMC 3167774. PMID 21909441.
- Lecordier L, Vanhollebeke B, Poelvoorde P, Tebabi P, Paturiaux-Hanocq F, Andris F, et al. (December 2009). Mansfield JM (ed.). "C-terminal mutants of apolipoprotein L-I efficiently kill both Trypanosoma brucei brucei and Trypanosoma brucei rhodesiense". PLOS Pathogens. 5 (12): e1000685. doi:10.1371/journal.ppat.1000685. PMC 2778949. PMID 19997494.
- De Greef C, Imberechts H, Matthyssens G, Van Meirvenne N, Hamers R (September 1989). "A gene expressed only in serum-resistant variants of Trypanosoma brucei rhodesiense". Molecular and Biochemical Parasitology. 36 (2): 169–176. doi:10.1016/0166-6851(89)90189-8. PMID 2528066.
- Ogbadoyi E, Ersfeld K, Robinson D, Sherwin T, Gull K (March 2000). "Architecture of the Trypanosoma brucei nucleus during interphase and mitosis". Chromosoma. 108 (8): 501–513. doi:10.1007/s004120050402. PMID 10794572. S2CID 3850480.
- Jackson AP, Sanders M, Berry A, McQuillan J, Aslett MA, Quail MA, et al. (April 2010). "The genome sequence of Trypanosoma brucei gambiense, causative agent of chronic human african trypanosomiasis". PLOS Neglected Tropical Diseases. 4 (4): e658. doi:10.1371/journal.pntd.0000658. PMC 2854126. PMID 20404998.
- Ogbadoyi EO, Robinson DR, Gull K (May 2003). "A high-order trans-membrane structural linkage is responsible for mitochondrial genome positioning and segregation by flagellar basal bodies in trypanosomes". Molecular Biology of the Cell. 14 (5): 1769–1779. doi:10.1091/mbc.E02-08-0525. PMC 165075. PMID 12802053.
- Borst P, Sabatini R (2008). "Base J: discovery, biosynthesis, and possible functions". Annual Review of Microbiology. 62: 235–251. doi:10.1146/annurev.micro.62.081307.162750. PMID 18729733.
- Barry JD, McCulloch R (2001). "Antigenic variation in trypanosomes: enhanced phenotypic variation in a eukaryotic parasite". Advances in Parasitology Volume 49. Advances in Parasitology. Vol. 49. pp. 1–70. doi:10.1016/S0065-308X(01)49037-3. ISBN 978-0-12-031749-3. PMID 11461029.
- Barry JD, McCulloch R (2001). "Antigenic variation in trypanosomes: enhanced phenotypic variation in a eukaryotic parasite". Advances in Parasitology Volume 49. Advances in Parasitology. Vol. 49. pp. 1–70. doi:10.1016/S0065-308X(01)49037-3. ISBN 978-0-12-031749-3. PMID 11461029.
- Morrison LJ, Marcello L, McCulloch R (December 2009). "Antigenic variation in the African trypanosome: molecular mechanisms and phenotypic complexity". Cellular Microbiology. 11 (12): 1724–1734. doi:10.1111/j.1462-5822.2009.01383.x. PMID 19751359. S2CID 26552797.
- Turner CM (August 1997). "The rate of antigenic variation in fly-transmitted and syringe-passaged infections of Trypanosoma brucei". FEMS Microbiology Letters. 153 (1): 227–231. doi:10.1111/j.1574-6968.1997.tb10486.x. PMID 9252591.
- Barry JD, Hall JP, Plenderleith L (September 2012). "Genome hyperevolution and the success of a parasite". Annals of the New York Academy of Sciences. 1267 (1): 11–17. Bibcode:2012NYASA1267...11B. doi:10.1111/j.1749-6632.2012.06654.x. PMC 3467770. PMID 22954210.
- Hall JP, Wang H, Barry JD (11 July 2013). "Mosaic VSGs and the scale of Trypanosoma brucei antigenic variation". PLOS Pathogens. 9 (7): e1003502. doi:10.1371/journal.ppat.1003502. PMC 3708902. PMID 23853603.
- Mugnier MR, Cross GA, Papavasiliou FN (March 2015). "The in vivo dynamics of antigenic variation in Trypanosoma brucei". Science. 347 (6229): 1470–1473. Bibcode:2015Sci...347.1470M. doi:10.1126/science.aaa4502. PMC 4514441. PMID 25814582.
- Pays E (November 2005). "Regulation of antigen gene expression in Trypanosoma brucei". Trends in Parasitology. 21 (11): 517–520. doi:10.1016/j.pt.2005.08.016. PMID 16126458.
- Rudenko G (26 October 2018). "Faculty of 1000 evaluation for Genome organization and DNA accessibility control antigenic variation in trypanosomes". F1000. doi:10.3410/f.734240334.793552268.
- Müller LS, Cosentino RO, Förstner KU, Guizetti J, Wedel C, Kaplan N, et al. (November 2018). "Genome organization and DNA accessibility control antigenic variation in trypanosomes". Nature. Nature Research. 563 (7729): 121–125. Bibcode:2018Natur.563..121M. doi:10.1038/s41586-018-0619-8. PMC 6784898. PMID 30333624.
- Hajduk SL, Moore DR, Vasudevacharya J, Siqueira H, Torri AF, Tytler EM, Esko JD (March 1989). "Lysis of Trypanosoma brucei by a toxic subspecies of human high density lipoprotein". The Journal of Biological Chemistry. 264 (9): 5210–5217. doi:10.1016/S0021-9258(18)83720-6. PMID 2494183.
- Raper J, Fung R, Ghiso J, Nussenzweig V, Tomlinson S (April 1999). "Characterization of a novel trypanosome lytic factor from human serum". Infection and Immunity. 67 (4): 1910–1916. doi:10.1128/IAI.67.4.1910-1916.1999. PMC 96545. PMID 10085035.
- Vanhollebeke B, Pays E (May 2010). "The trypanolytic factor of human serum: many ways to enter the parasite, a single way to kill" (PDF). Molecular Microbiology. 76 (4): 806–814. doi:10.1111/j.1365-2958.2010.07156.x. PMID 20398209. S2CID 7740199.
- Lugli EB, Pouliot M, Portela Md, Loomis MR, Raper J (November 2004). "Characterization of primate trypanosome lytic factors". Molecular and Biochemical Parasitology. 138 (1): 9–20. doi:10.1016/j.molbiopara.2004.07.004. PMID 15500911.
- Vanhollebeke B, Pays E (September 2006). "The function of apolipoproteins L". Cellular and Molecular Life Sciences. 63 (17): 1937–1944. doi:10.1007/s00018-006-6091-x. PMID 16847577. S2CID 12713960.
- Vanhamme L, Paturiaux-Hanocq F, Poelvoorde P, Nolan DP, Lins L, Van Den Abbeele J, et al. (March 2003). "Apolipoprotein L-I is the trypanosome lytic factor of human serum". Nature. 422 (6927): 83–87. Bibcode:2003Natur.422...83V. doi:10.1038/nature01461. PMID 12621437. S2CID 4310920.
- Smith EE, Malik HS (May 2009). "The apolipoprotein L family of programmed cell death and immunity genes rapidly evolved in primates at discrete sites of host-pathogen interactions". Genome Research. 19 (5): 850–858. doi:10.1101/gr.085647.108. PMC 2675973. PMID 19299565.
- Genovese G, Friedman DJ, Ross MD, Lecordier L, Uzureau P, Freedman BI, et al. (August 2010). "Association of trypanolytic ApoL1 variants with kidney disease in African Americans". Science. 329 (5993): 841–845. Bibcode:2010Sci...329..841G. doi:10.1126/science.1193032. PMC 2980843. PMID 20647424.
- Wasser WG, Tzur S, Wolday D, Adu D, Baumstein D, Rosset S, Skorecki K (2012). "Population genetics of chronic kidney disease: the evolving story of APOL1". Journal of Nephrology. 25 (5): 603–618. doi:10.5301/jn.5000179. PMID 22878977.
- Lipkowitz MS, Freedman BI, Langefeld CD, Comeau ME, Bowden DW, Kao WH, et al. (January 2013). "Apolipoprotein L1 gene variants associate with hypertension-attributed nephropathy and the rate of kidney function decline in African Americans". Kidney International. 83 (1): 114–120. doi:10.1038/ki.2012.263. PMC 3484228. PMID 22832513.
- Duchateau PN, Pullinger CR, Orellana RE, Kunitake ST, Naya-Vigne J, O'Connor PM, et al. (October 1997). "Apolipoprotein L, a new human high density lipoprotein apolipoprotein expressed by the pancreas. Identification, cloning, characterization, and plasma distribution of apolipoprotein L". The Journal of Biological Chemistry. 272 (41): 25576–25582. doi:10.1074/jbc.272.41.25576. PMID 9325276.
- Pérez-Morga D, Vanhollebeke B, Paturiaux-Hanocq F, Nolan DP, Lins L, Homblé F, et al. (July 2005). "Apolipoprotein L-I promotes trypanosome lysis by forming pores in lysosomal membranes". Science. 309 (5733): 469–472. Bibcode:2005Sci...309..469P. doi:10.1126/science.1114566. PMID 16020735. S2CID 33189804.
- Madhavan SM, O'Toole JF, Konieczkowski M, Ganesan S, Bruggeman LA, Sedor JR (November 2011). "APOL1 localization in normal kidney and nondiabetic kidney disease". Journal of the American Society of Nephrology. 22 (11): 2119–2128. doi:10.1681/ASN.2011010069. PMC 3231786. PMID 21997392.
- Zhaorigetu S, Wan G, Kaini R, Jiang Z, Hu CA (November 2008). "ApoL1, a BH3-only lipid-binding protein, induces autophagic cell death". Autophagy. 4 (8): 1079–1082. doi:10.4161/auto.7066. PMC 2659410. PMID 18927493.
- Widener J, Nielsen MJ, Shiflett A, Moestrup SK, Hajduk S (September 2007). "Hemoglobin is a co-factor of human trypanosome lytic factor". PLOS Pathogens. 3 (9): 1250–1261. doi:10.1371/journal.ppat.0030129. PMC 1971115. PMID 17845074.
- Vanhollebeke B, De Muylder G, Nielsen MJ, Pays A, Tebabi P, Dieu M, et al. (May 2008). "A haptoglobin-hemoglobin receptor conveys innate immunity to Trypanosoma brucei in humans". Science. 320 (5876): 677–681. Bibcode:2008Sci...320..677V. doi:10.1126/science.1156296. PMID 18451305. S2CID 206512161.
- Vanhollebeke B, Nielsen MJ, Watanabe Y, Truc P, Vanhamme L, Nakajima K, et al. (March 2007). "Distinct roles of haptoglobin-related protein and apolipoprotein L-I in trypanolysis by human serum". Proceedings of the National Academy of Sciences of the United States of America. 104 (10): 4118–4123. Bibcode:2007PNAS..104.4118V. doi:10.1073/pnas.0609902104. PMC 1820718. PMID 17360487.
- Higgins MK, Tkachenko O, Brown A, Reed J, Raper J, Carrington M (January 2013). "Structure of the trypanosome haptoglobin-hemoglobin receptor and implications for nutrient uptake and innate immunity". Proceedings of the National Academy of Sciences of the United States of America. 110 (5): 1905–1910. Bibcode:2013PNAS..110.1905H. doi:10.1073/pnas.1214943110. PMC 3562850. PMID 23319650.
- Green HP, Del Pilar Molina Portela M, St Jean EN, Lugli EB, Raper J (January 2003). "Evidence for a Trypanosoma brucei lipoprotein scavenger receptor". The Journal of Biological Chemistry. 278 (1): 422–427. doi:10.1074/jbc.M207215200. PMID 12401813.
- Pays E, Vanhollebeke B, Vanhamme L, Paturiaux-Hanocq F, Nolan DP, Pérez-Morga D (June 2006). "The trypanolytic factor of human serum". Nature Reviews. Microbiology. 4 (6): 477–486. doi:10.1038/nrmicro1428. PMID 16710327. S2CID 6151924.
- Uzureau P, Uzureau S, Lecordier L, Fontaine F, Tebabi P, Homblé F, et al. (September 2013). "Mechanism of Trypanosoma brucei gambiense resistance to human serum". Nature. 501 (7467): 430–434. Bibcode:2013Natur.501..430U. doi:10.1038/nature12516. PMID 23965626. S2CID 4400057.
- DeJesus E, Kieft R, Albright B, Stephens NA, Hajduk SL (2013). "A single amino acid substitution in the group 1 Trypanosoma brucei gambiense haptoglobin-hemoglobin receptor abolishes TLF-1 binding". PLOS Pathogens. 9 (4): e1003317. doi:10.1371/journal.ppat.1003317. PMC 3630162. PMID 23637606.
- Smith A, McCulloh RJ (2015). "Hemopexin and haptoglobin: allies against heme toxicity from hemoglobin not contenders". Frontiers in Physiology. 6: 187. doi:10.3389/fphys.2015.00187. PMC 4485156. PMID 26175690.
- Pays E, Vanhollebeke B (July 2008). "Mutual self-defence: the trypanolytic factor story". Microbes and Infection. 10 (9): 985–989. doi:10.1016/j.micinf.2008.07.020. PMID 18675374.
- Xong HV, Vanhamme L, Chamekh M, Chimfwembe CE, Van Den Abbeele J, Pays A, et al. (December 1998). "A VSG expression site-associated gene confers resistance to human serum in Trypanosoma rhodesiense". Cell. 95 (6): 839–846. doi:10.1016/S0092-8674(00)81706-7. PMID 9865701.
- Shiflett AM, Faulkner SD, Cotlin LF, Widener J, Stephens N, Hajduk SL (2007). "African trypanosomes: intracellular trafficking of host defense molecules". The Journal of Eukaryotic Microbiology. 54 (1): 18–21. doi:10.1111/j.1550-7408.2006.00228.x. PMID 17300512. S2CID 20054667.
- Thomson R, Molina-Portela P, Mott H, Carrington M, Raper J (November 2009). "Hydrodynamic gene delivery of baboon trypanosome lytic factor eliminates both animal and human-infective African trypanosomes". Proceedings of the National Academy of Sciences of the United States of America. 106 (46): 19509–19514. Bibcode:2009PNAS..10619509T. doi:10.1073/pnas.0905669106. PMC 2780755. PMID 19858474.
- Richard Seed, John; Seed, Thomas M.; Sechelski, John (January 1978). "The biological effects of tryptophol (indole-3-ethanol): Hemolytic, biochemical and behavior modifying activity". Comparative Biochemistry and Physiology Part C: Comparative Pharmacology. 60 (2): 175–185. doi:10.1016/0306-4492(78)90091-6. PMID 28889.
External links
- "Trypanosomiasis, African (Trypanosoma brucei gambiense) (Trypanosoma brucei rhodesiense)". DPDx—Laboratory Identification of Parasitic Diseases of Public Health Concern. Centers for Disease Control and Prevention. 29 November 2013.
- "Trypanosoma brucei". NCBI Taxonomy Browser. 5691.
- "Parasites – African Trypanosomiasis (also known as Sleeping Sickness)". Centers for Disease Control and Prevention. 8 June 2018.