MOG antibody disease
| MOG antibody disease | |
|---|---|
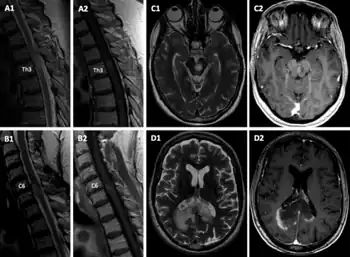 | |
| a1,2) sMRI T2- hyperintense lesion on level Th3 with Gd-enhancement on T1w on sagittal sequences b1,2) sMRI new cervical lesion on level C6 with T2 hyperintense signal and rim-enhancing pattern c1,2) cMRI shows a sharply demarcated pontomesencephalic; leopard pattern was noted on T2-weighted sequences with multiple small focal zones d1,2) demarcated confluent tumefactive parieto-occipital lesion across the splenium of the corpus callosum with rim-enhancing pattern | |
| Frequency | Lua error in Module:PrevalenceData at line 5: attempt to index field 'wikibase' (a nil value). |
MOG antibody disease (MOGAD) or MOG antibody-associated encephalomyelitis (MOG-EM)[1] is an inflammatory demyelinating disease of the central nervous system. Serum anti-myelin oligodendrocyte glycoprotein antibodies are present in up to half of patients with an acquired demyelinating syndrome and have been described in association with a range of phenotypic presentations, including acute disseminated encephalomyelitis, optic neuritis, transverse myelitis, and neuromyelitis optica.[2]
Signs and symptoms
The clinical presentation is variable and largely dependent upon the overall clinical manifestation.
The presence of anti-MOG autoantibodies has been described in association with the following conditions:[3]
- Seronegative neuromyelitis optica.[4][5]
- Acute disseminated encephalomyelitis, especially in recurrent and fulminant cases.[6]
- Multiple sclerosis.[3][7][8][9]
- Optic neuritis[10][3] (including cases of CRION (chronic relapsing inflammatory optic neuropathy[11])
- Transverse myelitis[3]
- Aseptic meningitis and meningoencephalitis (typically post-infectious).[12]
The most common presenting phenotypes are acute disseminated encephalomyelitis (ADEM) in children and optic neuritis (ON) in adults.[13] Some of these phenotypes have been studied in detail:
Seronegative neuromyelitis optica
Anti-MOG antibodies have been described in some patients with NMOSD[14][15] who were negative for the aquaporin 4 (AQP-4) antibody. However, most NMOSD is an astrocytopathy, specifically an AQP4 antibody-associated disease, whereas MOG antibody-associated disease is an oligodendrocytopathy, suggesting that these are two separate pathologic entities.[16] Rare cases have been described of patients with antibodies against both AQP4 and MOG. These patients typically have MS-like brain lesions, multifocal spine lesions and optic nerve atrophy.[17] However, the coexistence of both antibodies is still a matter of ongoing debate.[18]
ADEM
The presence of anti-MOG antibodies is more common in children with ADEM.[19][20]
Tumefactive demyelination
Rare cases of anti-MOG antibodies in association with tumefactive multiple sclerosis have been described.[21]
Causes
The reason why anti-MOG auto-antibodies appear remains unknown.
A post-infectious autoimmune process has been proposed as a possible pathophysiologic mechanism.[22] Other reports point to molecular mimicry between MOG and some viruses as a possible etiology.[23]
Histopathology
Demyelinating lesions of MOG-associated encephalomyelitis resemble more those observed in multiple sclerosis[24] than NMO. They are similar to pattern-II multiple sclerosis[25] with T-cells and macrophages surrounding blood vessels, preservation of oligodendrocytes and signs of complement system activation.
Several studies performed during 2020 have shown that MOGAD lesions differ from those seen in MS in many aspects, including their topographical distribution in the CNS, the type of demyelination, and the nature of the inflammatory response.[26]
- MOGAD demyelination occurs by confluence of small perivenous lesions, generally resulting in a demyelination pattern similar to that seen in acute disseminated encephalomyelitis. Demyelination in MOGAD is associated with complement deposition at the site of active myelin injury, but the degree of complement activation is much less compared to that seen in patients with aquaporin 4 antibody associated neuromyelitis optica (NMO).
- While in MS the dominant inflammatory reaction is seen around the larger drainage veins in the periventricular tissue and the meninges, in MOGAD the smaller veins and venules are mainly affected.
- Finally, in MOGAD, infiltrating lymphocytes are mainly CD4+ T-cells with low numbers of CD8+ T-cells and B-cells; the dominant lymphocytes in active MS lesions are tissue resident CD8+ effector memory T-cells and B-cells / plasma cells.
Diagnosis
MOG-IgG is detected by means of so-called cell-based assays (CBA). CBA using live cells transfected with full-length human MOG and employing Fc-specific detection antibodies are the gold standard for anti-MOG antibody testing.[27] Serum is the specimen of choice; cerebrospinal fluid (CSF) analysis is less sensitive compared to serum testing.[27][28][29]
Cerebrospinal fluid oligoclonal bands, the diagnostic mainstay in multiple sclerosis (MS), are rare in MOG-EM, both in adults[30] and in children.[31] If present at all, intrathecal IgG synthesis is low in most patients, often transient, and mainly restricted to acute attacks.[30][31] CSF findings are significantly more pronounced in acute myelitis than in acute ON, which is frequently associated with normal CSF findings, and depends significantly on disease activity (more pronounced during acute attacks), attack severity, and spinal cord lesion extension.[30][31] CSF white cell numbers in MOG-EM may be higher than in MS, especially in acute myelitis, but normal cell numbers do not rule out the disease.[30][31] CSF often contains neutrophil granulocytes and CSF L-lactate levels may be elevated, thus mimicking bacterial meningitis in some cases.[30][31] The intrathecal, polyclonal antiviral immune response (so-called MRZ reaction), which is present in around 63% of MS patients, is absent in MOG-EM.[30][31]
Proposed diagnostic criteria require serum positivity for MOG antibody as detected by CBA, a clinicoradiological presentation consistent with an acquired demyelinating syndrome (VEP can replace radiological evidence only in patients with acute ON), and exclusion of alternative diagnoses;[1] in addition, so-called 'red flags' have been defined, which, if present, should prompt physicians to challenge the diagnosis and to prompt re-testing for MOG-IgG, ideally using a second, methodologically different assay.[1]
In the young, MRI typically shows ADEM–like lesions and longitudinally extensive transverse myelitis (LETM), whereas optic neuritis and short transverse myelitis are more commonly seen in older patients.[32] However, rare cases of symptomatic MRI-negative MOG-related disease have been described.[33]
Clinical course
Two clinical courses have been described:[34]
- Monophasic (most common)
- Relapsing
Treatment
Acute therapy consists of high-dose corticosteroids, IVIG, or plasma exchange, and long-term immunosuppression may be necessary in recurrent cases.[35][36] Anti-MOG positive patients should not be treated with interferons as these may worsen the disease course similar to those with NMOSD.[29]
There are also anecdotal reports against using fingolimod[37] or Alemtuzumab.[38]
Prognosis
Residual disability develops in 50–80% of patients, with transverse myelitis at onset being the most significant predictor of long-term outcome.
Research
Animal models in experimental autoimmune encephalomyelitis, EAE, have shown that “MOG-specific EAE models (of different animal strains) display/mirror human multiple sclerosis" but EAE pathology is closer to NMO and ADEM than to the confluent demyelination observed in MS.[39]
History
Reports describing the possible involvement of anti-MOG antibodies in multiple sclerosis and other demyelinating conditions first appeared in the literature in the late 1980s, but evidence to support their role in demyelinating disease was always weak and inconsistent.[40] The possibility of an anti-MOG MS-subtype was considered around 2000.[41]
The turning point was in 2011, when Mader et al. developed a cell-based assay using HEK 293 cells which increased the detection rate of these antibodies in the serum.[42]
Reports about prevalence of anti-MOG in selected Multiple Sclerosis cases began to appear in 2016[43]
References
- 1 2 3 Jarius, S.; Paul, F.; Aktas, O.; Asgari, N.; Dale, R. C.; de Seze, J.; Franciotta, D.; Fujihara, K.; Jacob, A.; Kim, H. J.; Kleiter, I. (2018-05-03). "MOG encephalomyelitis: international recommendations on diagnosis and antibody testing". Journal of Neuroinflammation. 15 (1): 134. doi:10.1186/s12974-018-1144-2. ISSN 1742-2094. PMC 5932838. PMID 29724224. Archived from the original on 2022-04-19. Retrieved 2022-04-17.
- ↑ Ramanathan, Sudarshini; Dale, Russell C.; Brilot, Fabienne (2016). "Anti-MOG antibody: The history, clinical phenotype, and pathogenicity of a serum biomarker for demyelination". Autoimmunity Reviews. 15 (4): 307–324. doi:10.1016/j.autrev.2015.12.004. PMID 26708342.
- 1 2 3 4 Reindl, M; Di Pauli, F; Rostásy, K; Berger, T (Aug 2013). "The spectrum of MOG autoantibody-associated demyelinating diseases". Nat Rev Neurol. 9 (8): 455–61. doi:10.1038/nrneurol.2013.118. PMID 23797245. S2CID 7219279.
- ↑ Jarius, Sven; Paul, Friedemann; Weinshenker, Brian G.; Levy, Michael; Kim, Ho Jin; Wildemann, Brigitte (2020-10-22). "Neuromyelitis optica". Nature Reviews. Disease Primers. 6 (1): 85. doi:10.1038/s41572-020-0214-9. ISSN 2056-676X. PMID 33093467. Archived from the original on 2021-06-11. Retrieved 2022-04-17.
- ↑ Hyun, Jae-Won; Woodhall, Mark R; Kim, Su-Hyun; Hye Jeong, In; Kong, Byungsoo; Kim, Gayoung; Kim, Yeseul; Su Park, Min; Irani, Sarosh R; Waters, Patrick; Jin Kim, Ho (2017). "Longitudinal analysis of myelin oligodendrocyte glycoprotein antibodies in CNS inflammatory diseases". Journal of Neurology, Neurosurgery & Psychiatry. 88 (10): 811–817. doi:10.1136/jnnp-2017-315998. PMID 28684532. S2CID 22732252. Archived from the original on 2021-09-03. Retrieved 2022-04-17.
- ↑ Baumann, M.; Hennes, E.M.; Schanda, K.; Karenfort, M.; Bajer-Kornek, B.; Diepold, K.; Fiedler, B.; Marquardt, I.; Strautmanis, J.; Vieker, S.; Reindl, M.; Rostásy, K. (2015). "Clinical characteristics and neuroradiological findings in children with multiphasic demyelinating encephalomyelitis and MOG antibodies". European Journal of Paediatric Neurology. 19 (Supplement 1): S21. doi:10.1016/S1090-3798(15)30066-0.
- ↑ Jarius S, Metz I, König FB, Ruprecht K, Reindl M, Paul F, Brück W, Wildemann B. "Screening for MOG-IgG and 27 other anti-glial and anti-neuronal autoantibodies in 'pattern II multiple sclerosis' and brain biopsy findings in a MOG-IgG-positive case Mult Scler. 2016 Feb;
- ↑ Di Pauli, F. (2015). "Fulminant demyelinating encephalomyelitis: Insights from antibody studies and neuropathology". Neurology: Neuroimmunology. 2 (6): e175. doi:10.1212/NXI.0000000000000175. PMC 4635550. PMID 26587556.
- ↑ Spadaro, Melania (2016). "Autoantibodies to MOG in a distinct subgroup of adult multiple sclerosis". Neurology - Neuroimmunology Neuroinflammation. 3 (5): e257. doi:10.1212/NXI.0000000000000257. PMC 4949775. PMID 27458601.
- ↑ Tajfirouz, Deena A.; Bhatti, M. Tariq; Chen, John J. (26 November 2019). "Clinical Characteristics and Treatment of MOG-IgG–Associated Optic Neuritis". Current Neurology and Neuroscience Reports. 19 (12): 100. doi:10.1007/s11910-019-1014-z. PMID 31773369. S2CID 208278781.
- ↑ Chalmoukou, Konstantina; et al. (2015). "Anti-MOG antibodies are frequently associated with steroid-sensitive recurrent optic neuritis". Neurol Neuroimmunol Neuroinflamm. 2 (4): e131. doi:10.1212/NXI.0000000000000131. PMC 4496630. PMID 26185777.
- ↑ Narayan, Ram N; Wang, Cynthia; Sguigna, Peter; Husari, Khalil; Greenberg, Benjamin (2019). "Atypical Anti-MOG syndrome with aseptic meningoencephalitis and pseudotumor cerebri-like presentations". Multiple Sclerosis and Related Disorders. 27: 30–33. doi:10.1016/j.msard.2018.10.003. PMID 30300850.
- ↑ de Mol, CL; Wong, YYM; van Pelt, ED; Wokke, BHA; Siepman, TAM; Neuteboom, RF; Hamann, D; Hintzen, RQ (16 May 2019). "The clinical spectrum and incidence of anti-MOG-associated acquired demyelinating syndromes in children and adults". Multiple Sclerosis Journal. 26 (7): 806–814. doi:10.1177/1352458519845112. PMC 7294530. PMID 31094288.
- ↑ Pröbstel, Anne-Katrin; et al. (2015). "Anti-MOG antibodies are present in a subgroup of patients with a neuromyelitis optica phenotype". Journal of Neuroinflammation. 12 (1): 46. doi:10.1186/s12974-015-0256-1. PMC 4359547. PMID 25889963.
- ↑ CYNTHIA MCKELVEY, Press Report, What’s the Role of Myelin Oligodendrocyte Glycoprotein in NMO? Archived 2022-02-26 at the Wayback Machine
- ↑ Ramanathan, Sudarshini; Dale, Russell C.; Brilot, Fabienne (2016). "Anti-MOG antibody: The history, clinical phenotype, and pathogenicity of a serum biomarker for demyelination". Autoimmunity Reviews. 15 (4): 307–324. doi:10.1016/j.autrev.2015.12.004. PMID 26708342.
- ↑ Ya, Yaping; et al. (2015). "Autoantibody to MOG suggests two distinct clinical subtypes of NMOSD". Science China Life Sciences. 59 (12): 1270–1281. doi:10.1007/s11427-015-4997-y. PMC 5101174. PMID 26920678.
- ↑ Weber, Martin S.; Derfuss, Tobias; Brück, Wolfgang (2018). "Anti–Myelin Oligodendrocyte Glycoprotein Antibody–Associated Central Nervous System Demyelination—A Novel Disease Entity?". JAMA Neurol. 75 (8): 909–910. doi:10.1001/jamaneurol.2018.1055. PMID 29913011.
- ↑ Knapp-Tężycka, Justyna; Zawadzka, Marta; Knurowska, Agata; Anuszkiewicz, Karolina; Stogowski, Piotr; Wiśniewska, Sylwia; Lemka, Małgorzata; Mazurkiewicz-Bełdzińska, Maria (2020). "Zapalenie nerwów wzrokowych, mózgu i rdzenia związane z MOG-IgG (MONEM)". Polski Przeglad Neurologiczny. 16: 46–50. doi:10.5603/PPN.2020.0005. Archived from the original on 2022-05-14. Retrieved 2022-04-17.
- ↑ Silvia Tenembaum et al. Spectrum of MOG Autoantibody-Associated Inflammatory Diseases in Pediatric Patients, Neurology April 6, 2015 vol. 84 no. 14 Supplement I4-3A
- ↑ Yaqing Shu Youming Long Shisi Wang Wanming Hu Jian Zhou Huiming Xu Chen Chen Yangmei Ou Zhengqi Lu Alexander Y. Lau Xinhua Yu Allan G. Kermode Wei Qiu, Brain histopathological study and prognosis in MOG antibody‐associated demyelinating pseudotumor, 08 January 2019, https://doi.org/10.1002/acn3.712
- ↑ Kakalacheva, Kristina; et al. (2016). "Infectious Mononucleosis Triggers Generation of IgG Auto-Antibodies against Native Myelin Oligodendrocyte Glycoprotein". Viruses. 8 (2): 51. doi:10.3390/v8020051. PMC 4776206. PMID 26907324.
- ↑ De Luca et al. Cross-reactivity between myelin oligodendrocyte glycoprotein and human endogenous retrovirus W protein: nanotechnological evidence for the potential trigger of multiple sclerosis, Micron Volume 120, May 2019, Pages 66-73, doi: https://doi.org/10.1016/j.micron.2019.02.005 Archived 2021-09-03 at the Wayback Machine
- ↑ Spadaro Melania; et al. (2015). "Histopathology and clinical course of MOG-antibody-associated encephalomyelitis". Annals of Clinical and Translational Neurology. 2 (3): 295–301. doi:10.1002/acn3.164. PMC 4369279. PMID 25815356.
- ↑ Deena A. Tajfirouz, M. Tariq Bhatti, John J. Chen, Clinical Characteristics and Treatment of MOG-IgG–Associated Optic Neuritis Current Neurology and Neuroscience Reports, December 2019
- ↑ Lassmann, Hans (12 January 2021). "Neuroinflammation: 2021 update". Free Neuropathology. 2: 1–1. doi:10.17879/freeneuropathology-2021-3166.
- 1 2 Jarius S, Paul F, Aktas O, Asgari N, Dale RC, de Seze J, et al. (May 2018). "MOG encephalomyelitis: international recommendations on diagnosis and antibody testing". J Neuroinflammation. 15 (1): 134. doi:10.1186/s12974-018-1144-2. PMC 5932838. PMID 29724224.
- ↑ Jarius, Sven (2016). "MOG-IgG in NMO and related disorders: a multicenter study of 50 patients. Part 1: Frequency, syndrome specificity, influence of disease activity, long-term course, association with AQP4-IgG, and origin". Journal of Neuroinflammation. 13: 279. doi:10.1186/s12974-016-0717-1. PMID 27788675. Archived from the original on 2022-03-29. Retrieved 2022-04-17.
- 1 2 Nakashima, Ichiro (2015). "Anti-myelin oligodendrocyte glycoprotein antibody in demyelinating diseases". Clinical and Experimental Neuroimmunology. 6: 59–63. doi:10.1111/cen3.12262. S2CID 74183244.
- 1 2 3 4 5 6 Jarius, Sven (2020). "Cerebrospinal fluid findings in patients with myelin oligodendrocyte glycoprotein (MOG) antibodies. Part 1: Results from 163 lumbar punctures in 100 adult patients". Journal of Neuroinflammation. 17 (1): 261. doi:10.1186/s12974-020-01824-2. PMC 7470615. PMID 32883348.
- 1 2 3 4 5 6 Jarius, Sven (2020). "Cerebrospinal fluid findings in patients with myelin oligodendrocyte glycoprotein (MOG) antibodies. Part 2: Results from 108 lumbar punctures in 80 pediatric patients". Journal of Neuroinflammation. 17: 261. doi:10.1186/s12974-020-01825-1. PMC 7470445. Archived from the original on 2022-01-26. Retrieved 2022-04-17.
- ↑ Maciej Jurynczyk Ruth Geraldes Fay Probert Mark R. Woodhall Patrick Waters George Tackley Gabriele DeLuca Saleel Chandratre Maria I. Leite Angela Vincent, Distinct brain imaging characteristics of autoantibody-mediated CNS conditions and multiple sclerosis, Brain, Volume 140, Issue 3, 1 March 2017, Pages 617–627, https://doi.org/10.1093/brain/aww350 Archived 2022-05-14 at the Wayback Machine, 24 February 2017
- ↑ Pérez CA, Garcia-Tarodo S, Troxell R. MRI-Negative Myelitis Associated With Myelin Oligodendrocyte Glycoprotein Antibody Spectrum Demyelinating Disease. Child Neurol Open. 2019;6:2329048X19830475. Published 2019 Feb 17. https://doi.org/10.1177/2329048X19830475 Archived 2022-05-14 at the Wayback Machine
- ↑ Pandit, Lekha; Mustafa, Sharik; Nakashima, Ichiro; Takahashi, Toshyuki; Kaneko, Kimhiko (2018). "MOG-IgG-associated disease has a stereotypical clinical course, asymptomatic visual impairment and good treatment response". Multiple Sclerosis Journal - Experimental, Translational and Clinical. 4 (3): 205521731878782. doi:10.1177/2055217318787829. PMC 6050870. PMID 30038790.
- ↑ Oshiro A, Nakamura S, Tamashiro K, Fujihara K. Anti-MOG + neuromyelitis optica spectrum disorders treated with plasmapheresis, No To Hattatsu. 2016 May;48(3):199-203
- ↑ Rocio Vazquez do Campo, Ramon Yarza, Sebastian Lopez Chiriboga and Kevin Barrett, Myelin Oligodendrocyte Glycoprotein (MOG) Autoimmunity. A Case Report, Neurology April 5, 2016 vol. 86 no. 16 Supplement P5.346
- ↑ Miyazaki, T; Nakajima, H; Motomura, M; Tanaka, K; Maeda, Y; Shiraishi, H; Tsujino, A (2016). "A case of recurrent optic neuritis associated with cerebral and spinal cord lesions and autoantibodies against myelin oligodendrocyte glycoprotein relapsed after fingolimod therapy". Rinsho Shinkeigaku. 56 (4): 265–9. doi:10.5692/clinicalneurol.cn-000756. PMID 27010093.
- ↑ Seneviratne, Sinali; Marriott, Mark; Monif, Mastura (2019). "065 Presence of anti-myelin oligodendrocyte glycoprotein antibodies in the serum of two patients following alemtuzumab therapy for suspected multiple sclerosis". Journal of Neurology, Neurosurgery & Psychiatry. 90: A21.2–A21. doi:10.1136/jnnp-2019-anzan.57.
- ↑ Kezuka; et al. (2012). "Relationship Between NMO-Antibody and Anti–MOG Antibody in Optic Neuritis". Journal of Neuro-Ophthalmology. 32 (2): 107–110. doi:10.1097/WNO.0b013e31823c9b6c. PMID 22157536. S2CID 46667141.
- ↑ Fujihara K, et al. (8 March 2018). "Myelin oligodendrocyte glycoprotein immunoglobulin G-associated disease: An overview". Clinical and Experimental Neuroimmunology. 9: 48–55. doi:10.1111/cen3.12434.
- ↑ Egg, R; Reindl, M; Deisenhammer, F; Linington, C; Berger, T (October 2001). "Anti-MOG and anti-MBP antibody subclasses in multiple sclerosis". Multiple Sclerosis Journal. 7 (5): 285–289. doi:10.1177/135245850100700503. PMID 11724443. S2CID 23520476.
- ↑ Mader, S; Gredler, V; Schanda, K; et al. (2011). "Complement activating antibodies to myelin oligodendrocyte glycoprotein in neuromyelitis optica and related disorders". J Neuroinflammation. 8: 184. doi:10.1186/1742-2094-8-184. PMC 3278385. PMID 22204662.
- ↑ Spadaro, M; Gerdes, LA; Krumbholz, M; Ertl-Wagner, B; Thaler, FS; Schuh, E; Metz, I; Blaschek, A; Dick, A; Brück, W; Hohlfeld, R; Meinl, E; Kümpfel, T (2016). "Autoantibodies to MOG in a distinct subgroup of adult multiple sclerosis". Neurol Neuroimmunol Neuroinflamm. 3 (5): e257. doi:10.1212/NXI.0000000000000257. PMC 4949775. PMID 27458601.