Liver tumor
| Liver tumor | |
|---|---|
| Other names: Hepatic tumor | |
 | |
| Left lobe liver tumor in 50-year-old man | |
| Specialty | Oncololgy |
| Symptoms | None, enlarged liver, abdominal pain, yellowish skin and eyes, vomiting, itchiness[1] |
| Types | Benign: Hemangioma, liver cyst, hepatic granuloma, hepatocellular adenoma[2] Malignant: Metastasis, hepatocellar carcinoma, bile duct cancer, hepatoblastoma[3] |
| Diagnostic method | Medical imaging, tissue biopsy[1] |
| Treatment | Depends on the type[1] |
Liver tumors are abnormal growths within the liver.[1] They may be benign or malignant (liver cancer).[2] Symptoms may vary from none to an enlarged liver, abdominal pain, yellowish skin and eyes, vomiting, and itchiness.[1]
Benign tumors include hemangiomas, liver cysts, hepatic granulomas, and hepatocellular adenomas.[2] Malignant tumors may form within the liver or spread from elsewhere in the body (metastasis).[2] The most common type to form within the liver is a hepatocellular carcinoma, with other types including bile duct cancer and hepatoblastoma.[1][3] They may be discovered on medical imaging and confirmed by tissue biopsy.[1]
Treatment depends on the type of tumor and may vary from none to chemotherapy, surgery, and liver transplant.[1] Benign tumors of the liver are relatively common.[1] Cancerous tumors of the liver are most commonly metastatic.[1] The first descriptions of surgery for liver tumors date from the late 1800s; however, it was not until the 1970s that major advances were made.[4]
Classification
Liver tumors are divided into two main groups, benign and cancerous.
Benign
There are several types of benign liver tumor.
Hemangiomas: These are the most common type of benign liver tumor, found in up to 7% of autopsy specimens. They start in blood vessels. Most of these tumors do not cause symptoms and do not need treatment. Some may bleed and need to be removed if it is mild to severe. A rare tumor is Infantile hemangioendothelioma.
Hepatic adenomas: These benign epithelial liver tumors develop in the liver and are also an uncommon occurrence, found mainly in women using estrogens as contraceptives, or in cases of steroid abuse. They are, in most cases, located in the right hepatic lobe and are frequently seen as solitary. The size of adenomas range from 1 to 30 cm. Symptoms associated with hepatic adenomas are all associate with large lesions which can cause intense abdominal pain. Over the last few decades there has been an increase with occurrences of this specific type of adenoma. The prognosis for these tumors has still not been mastered. Some correlations have been made such as malignant transformation, spontaneous hemorrhage, and rupture.
Focal nodular hyperplasia (FNH) is the second most common tumor of the liver. This tumor is the result of a congenital arteriovenous malformation hepatocyte response. This process is one in which all normal constituents of the liver are present, but the pattern by which they are presented is abnormal. Even though those conditions exist the liver still seems to perform in the normal range. Other types include nodular regenerative hyperplasia and hamartoma.
Cancerous
- Most cases are metastases from other tumors, frequently of the GI tract (like colon cancer, carcinoid tumors mainly of the appendix, etc.), but also from breast cancer, ovarian cancer, lung cancer, renal cancer, prostate cancer, etc.
- The most frequent, malignant, primary liver cancer is hepatocellular carcinoma (HCC, also named hepatoma, which is a misnomer because adenomas are usually benign).
- More rare primary forms of liver cancer include cholangiocarcinoma, mixed tumors, sarcoma and hepatoblastoma; a rare malignant tumor in children.
 Large HCC filling almost entire of right lobe
Large HCC filling almost entire of right lobe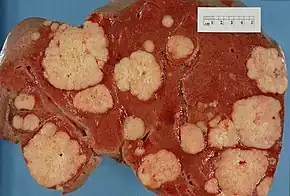 Cross section of a human liver, showing multiple large pale tumor deposits. The tumor is an adenocarcinoma derived from a primary lesion in the body of the pancreas.
Cross section of a human liver, showing multiple large pale tumor deposits. The tumor is an adenocarcinoma derived from a primary lesion in the body of the pancreas._(Radiopaedia_8480).jpg.webp) Hepatocellular carcinoma
Hepatocellular carcinoma
Diagnosis

Upon discovery of a liver tumor, the main issue in the workup is to determine whether the tumor is benign or malignant. Many imaging modalities are used to aid in the diagnosis of malignant liver tumors. For the most common of these, hepatocellular carcinoma (HCC), these include sonography (ultrasound), computed tomography (CT) and magnetic resonance imaging (MRI). When imaging the liver with ultrasound, a mass greater than 2 cm has more than 95% chance of being HCC. The majority of cholangiocarcimas occur in the hilar region of the liver, and often present as bile duct obstruction. If the cause of obstruction is suspected to be malignant, endoscopic retrograde cholangiopancreatography (ERCP), ultrasound, CT, MRI and magnetic resonance cholangiopancreatography (MRCP) are used.[6]
Tumor markers, chemicals sometimes found in the blood of people with cancer, can be helpful in diagnosing and monitoring the course of liver cancers. High levels of alpha-fetoprotein (AFP) in the blood can be found in many cases of HCC and intrahepatic cholangiocarcinoma. Cholangiocarcinoma can be detected with these commonly used tumor markers: carbohydrate antigen 19-9 (CA 19-9), carcinoembryonic antigen (CEA) and cancer antigen 125 (CA125). These tumour markers are found in primary liver cancers, as well as in other cancers and certain other disorders.[7][8]
Ultrasound
Ultrasonography of liver tumors involves two stages: detection and characterization. Tumor detection is based on the performance of the method and should include morphometric information (three axes dimensions, volume) and topographic information (number, location specifying liver segment and lobe/lobes). The specification of these data is important for staging liver tumors and prognosis. Tumor characterization is a complex process based on a sum of criteria leading towards tumor nature definition. Often, other diagnostic procedures, especially interventional ones are no longer necessary. Tumor characterization using the ultrasound method will be based on the following elements: consistency (solid, liquid, mixed), echogenicity, structure appearance (homogeneous or heterogeneous), delineation from adjacent liver parenchyma (capsular, imprecise), elasticity, posterior acoustic enhancement effect, the relation with neighboring organs or structures (displacement, invasion), vasculature (presence and characteristics on Doppler ultrasonography and contrast-enhanced ultrasound (CEUS).
Computed tomography

When evaluating hepatic masses by abdominal computed tomography (CT), it can be advantageous to have both late arterial and portal venous phase images since some tumors enhance briskly during the arterial phase (hepatocellular carcinoma, hepatic adenoma, follicular nodular hyperplasia (FNH), and hypervascular metastasis), but may be occult or difficult to characterize on portal venous phase imaging alone. However, it should be stressed that the addition of late arterial phase images is only indicated if one of these tumors is suspected, or if there is a need for further characterization of a hepatic mass, since the large majority of patients will not benefit from the addition of this phase. In addition, if there is a need to definitively characterize a hepatic mass, MRI is generally more sensitive and specific, with no associated radiation dose.
Treatment
The treatment of a hepatic tumor can entail locoregional ablation therapy, liver transplant,partial hepatectomy, chemotherapy, but of course depends on the individual situation/condition of the person.[9]
References
- 1 2 3 4 5 6 7 8 9 10 "Liver Tumors". www.hopkinsmedicine.org. Archived from the original on 26 February 2021. Retrieved 27 February 2021.
- 1 2 3 4 "Overview of Liver Tumors - Liver and Gallbladder Disorders". Merck Manuals Consumer Version. Archived from the original on 20 January 2021. Retrieved 23 February 2021.
- 1 2 "Cancerous tumours of the liver - Canadian Cancer Society". www.cancer.ca. Archived from the original on 25 May 2021. Retrieved 27 February 2021.
- ↑ Jarnagin, William R. (2012). Blumgart's Surgery of the Liver, Pancreas and Biliary Tract E-Book: Expert Consult - Online. Elsevier Health Sciences. p. 12. ISBN 978-1-4557-4606-4. Archived from the original on 2021-05-25. Retrieved 2021-02-27.
- ↑ Table 37.2 Archived 2020-02-24 at the Wayback Machine in: Sternberg, Stephen (2012). Sternberg's diagnostic surgical pathology. Place of publication not identified: LWW. ISBN 978-1-4511-5289-0. OCLC 953861627.
- ↑ Ariff, B; Lloyd, CR; Khan, S; Shariff, M; Thillainayagam, AV; Bansi, DS; Khan, SA; Taylor-Robinson, SD; Lim, AK (Mar 21, 2009). "Imaging of liver cancer". World Journal of Gastroenterology. 15 (11): 1289–300. doi:10.3748/wjg.15.1289. PMC 2658841. PMID 19294758.
- ↑ Malaguarnera, G; Paladina, I; Giordano, M; Malaguarnera, M; Bertino, G; Berretta, M (2013). "Serum markers of intrahepatic cholangiocarcinoma". Disease Markers. 34 (4): 219–28. doi:10.1155/2013/196412. PMC 3809974. PMID 23396291.
- ↑ Zhao YJ, Ju Q, Li GC (2013). "Tumor markers for hepatocellular carcinoma". Mol Clin Oncol. 1 (4): 593–598. doi:10.3892/mco.2013.119. PMC 3915636. PMID 24649215.
- ↑ Liu, Chun-Yu; Chen, Kuen-Feng; Chen, Pei-Jer (2015). "Treatment of Liver Cancer". Cold Spring Harbor Perspectives in Medicine. 5 (9). doi:10.1101/cshperspect.a021535. ISSN 2157-1422. Archived from the original on 28 August 2021. Retrieved 29 April 2021.
External links
| Classification |
|
|---|