Hemarthrosis
| Hemarthrosis | |
|---|---|
| Other names: Haemarthrosis | |
 | |
| Lipohemarthrosis (blood and fat in the joint space) seen in a person with a subtle tibial plateau fracture. The arrow indicates a fluid level between the upper fat component and the lower blood component. | |
| Specialty | Orthopedics |
Hemarthrosis is a bleeding into joint spaces. It is a common feature of hemophilia.
Signs and symptoms
Complications
Up to a quarter of all severe ligament or capsular knee injuries leading to a hemarthrosis are associated with cartilage damage that can lead to progressive degenerative arthritis.[1]
Causes
It usually follows injury but occurs mainly in patients with a predisposition to hemorrhage such as those being treated with warfarin (or other anticoagulants) and patients with hemophilia.
It can be associated with knee joint arthroplasty.[2]
It has also been reported as a part of hemorrhagic syndrome in the Crimean-Congo Hemorrhagic Fever, suggesting a viral cause to the bleeding in a joint space.[3][4]
Diagnosis
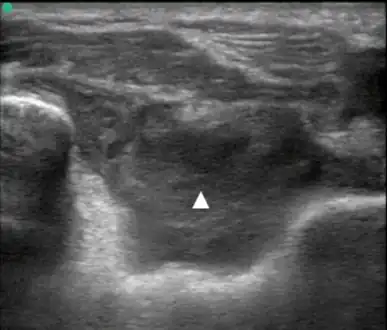 Posterior transverse view of the elbow with hemarthrosis
Posterior transverse view of the elbow with hemarthrosis X-ray of Hemarthrosis
X-ray of Hemarthrosis X-ray of Hemarthrosis
X-ray of Hemarthrosis
| Type | WBC per mm3 | % neutrophils | Viscosity | Appearance |
|---|---|---|---|---|
| Normal | <200 | 0 | High | Transparent |
| Osteoarthritis | <5000 | <25 | High | Clear yellow |
| Trauma | <10,000 | <50 | Variable | Bloody |
| Inflammatory | 2,000-50,000 | 50-80 | Low | Cloudy yellow |
| Septic arthritis | >50,000 | >75 | Low | Cloudy yellow |
| Gonorrhea | ~10,000 | 60 | Low | Cloudy yellow |
| Tuberculosis | ~20,000 | 70 | Low | Cloudy yellow |
| Inflammatory = gout, rheumatoid arthritis, rheumatic fever | ||||
Hemarthrosis is diagnosed through the methods listed below:
A physical examination is the first step, the joints of the patient are moved and bent to study the functioning.[7]
Synovial Fluid analysis is another method to diagnose Hemarthrosis. It involves a small needle being inserted into the joint to draw the fluid.[8] Reddish-colored hue of the sample is an indication of the blood being present. Imaging tests are normally done. The tests also include MRI, Ultrasound and X-ray test, which give better information about the joint inflammation.[9]
Treatment
In hemophilia it may occur spontaneously, and recurrent hemarthroses are a major cause of disability in that patient group due to hemophilic arthropathy, requiring synovectomy, joint replacement[10] and increased medical therapy to prevent further bleeding episodes.
Reducing hemarthroses events using intravenous administration of blood clotting factor concentrate on a regular basis starting in early childhood, reduces joint deterioration and increases the person's quality of life compared to "on demand" treatment (treating after a bleed).[11] The minimal effective dose and best dosage frequency have not been established.[11] It is not clear, due to lack of sufficient data, if preventative therapy with clotting factor concentrate is also effective at reducing joint deterioration if treatment is started after joint damage has occurred.[11]
References
- ↑ Goldberg A, Stansby G "Surgical Talk" 2nd edition
- ↑ Ohdera T, Tokunaga M, Hiroshima S, Yoshimoto E, Matsuda S (2004). "Recurrent hemarthrosis after knee joint arthroplasty: etiology and treatment". J Arthroplasty. 19 (2): 157–61. doi:10.1016/j.arth.2003.09.009. PMID 14973857.
- ↑ Ahmeti, Salih; Ajazaj-Berisha, Lindita; Halili, Bahrije; Shala, Anita (Apr 2014). "Acute arthritis in Crimean-Congo hemorrhagic fever". Journal of Global Infectious Diseases. 6 (2): 79–81. doi:10.4103/0974-777X.132052. PMC 4049045. PMID 24926169.
- ↑ Heyman, Paul; Cochez, Christel; Hofhuis, Agnetha; van der Giessen, Joke; Sprong, Hein; Porter, Sarah Rebecca; Losson, Bertrand; Saegerman, Claude; Donoso-Mantke, Oliver; Niedrig, Matthias; Papa, Anna (2010). "A Clear and Present Danger: Tick-borne Diseases in Europe". Expert Rev Anti Infect Ther. 8 (1): 33–50. doi:10.1586/eri.09.118. PMID 20014900. S2CID 28038692. Archived from the original on 2021-01-19. Retrieved 2022-06-27.
- ↑ Flynn, John A.; Choi, Michael J.; Wooster, L. Dwight (2013). Oxford American Handbook of Clinical Medicine. OUP USA. p. 400. ISBN 978-0-19-991494-4.
- ↑ Seidman, Aaron J.; Limaiem, Faten (2019), "Synovial Fluid Analysis", StatPearls, StatPearls Publishing, PMID 30725799, retrieved 2019-12-19
- ↑ "Hemarthrosis". Healthline. Archived from the original on 2021-01-21. Retrieved 2017-11-21.
- ↑ "Hemarthrosis - What You Need to Know". Drugs.com. Archived from the original on 2020-11-26. Retrieved 2017-11-21.
- ↑ Baker, C. L. (June 1992). "Acute hemarthrosis of the knee". Journal of the Medical Association of Georgia. 81 (6): 301–305. ISSN 0025-7028. PMID 1607844.
- ↑ Dunn AL (Sep 2005). "Management and prevention of recurrent hemarthrosis in patients with hemophilia". Current Opinion in Hematology. 12 (5): 390–4. doi:10.1097/01.moh.0000169285.66841.c8. PMID 16093785. S2CID 26117110.
- 1 2 3 Iorio, Alfonso; Marchesini, Emanuela; Marcucci, Maura; Stobart, Kent; Chan, Anthony Kc (2011-09-07). "Clotting factor concentrates given to prevent bleeding and bleeding-related complications in people with hemophilia A or B" (PDF). The Cochrane Database of Systematic Reviews (9): CD003429. doi:10.1002/14651858.CD003429.pub4. hdl:2434/231551. ISSN 1469-493X. PMID 21901684. Archived (PDF) from the original on 2022-09-27. Retrieved 2022-06-27.
External links
| Classification |
|---|