Mineral deficiency
Mineral deficiency is a lack of the dietary minerals, the micronutrients that are needed for an organism's proper health.[1] The cause may be a poor diet, impaired uptake of the minerals that are consumed, or a dysfunction in the organism's use of the mineral after it is absorbed. These deficiencies can result in many disorders including anemia and goitre. Examples of mineral deficiency include, zinc deficiency, iron deficiency, and magnesium deficiency.
Individual Mineral Deficiency
| Mineral | Symptoms & Diagnosis | Information |
|---|---|---|
| Calcium deficiency | Asymtomaic or, in severe cases, can have dramatic symptoms and be life-threatening. Symptoms of include numbness in fingers and toes, muscle cramps, irritability, impaired mental capacity and muscle twitching.[2] Vitamin D related hypocalcemia may be associated with a lack of vitamin D in the diet, a lack of sufficient UV exposure, or disturbances in renal function. Low vitamin D in the body can lead to a lack of calcium absorption and secondary hyperparathyroidism (hypocalcemia and raised parathyroid hormone).[2] | Parathyroid related or vitamin D related. |
| Chromium deficiency | Severely impaired glucose tolerance, weight loss, peripheral neuropathy and confusion.[3][4] | The authorities in the European Union do not recognize chromium as an essential nutrient,[5] those in the United States do, and identify an adequate intake for adults as between 25 and 45 μg/day, depending on age and sex.[4] Dietary supplements containing chromium are widely available in the United States, with claims for benefits for fasting plasma glucose, hemoglobin A1C and weight loss. Reviews report the changes as modest, and without scientific consensus that the changes have a clinically relevant impact.[6][7] |
| Copper deficiency | Neurological problems including myelopathy, peripheral neuropathy, and optic neuropathy. Blood symptoms of anemia and neutropenia.[8] | Copper deficiency can manifest in parallel with vitamin B12 and other nutritional deficiencies.[9] The most common cause of copper deficiency is a remote gastrointestinal surgery, such as gastric bypass surgery, due to malabsorption of copper, or zinc toxicity. |
| Fluorine deficiency | Increased dental caries and possibly osteoporosis | Fluorine is not considered to be an essential nutrient, but the importance of fluorides for preventing tooth decay is well-recognized,[10] although the effect is predominantly topical.[11] |
| iron deficiency | fatigue, dizziness/lightheadedness, pallor, hair loss, twitches, irritability, weakness, pica, brittle or grooved nails, hair thinning, pagophagia, restless legs syndrome[12] | Iron deficiency may be caused by blood loss, inadequate intake, medications interfering with absorption, mechanical hemolysis from athletics, malabsorption syndromes, inflammation, and parasitic infections. In a 2014 U.S. government consumption survey and reported that for men and women ages 20 and older the average iron intakes were, respectively, 16.6 and 12.6 mg/day.[13] |
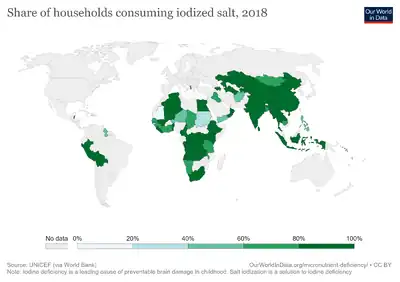
| Iodine deficiency | Goiter, congenital iodine deficiency syndrome, and fibrocystic breast changes | In areas where there is little iodine in the diet, typically remote inland areas where no marine foods are eaten, iodine deficiency is common. It is also common in mountainous regions of the world where food is grown in iodine-poor soil. Prevention includes adding small amounts of iodine to table salt, a product known as iodized salt. Iodine compounds have also been added to other foodstuffs, such as flour, water and milk, in areas of deficiency.[14] |
| Manganese deficiency | Skeletal deformation and inhibits the production of collagen in wound healing.[15] | Manganese is a vital element of nutrition in very small quantities (adult male daily intake 2.3 milligrams). |
| Magnesium deficiency | Tiredness, generalized weakness, muscle cramps, abnormal heart rhythms, increased irritability of the nervous system with tremors, paresthesias, palpitations, low potassium levels in the blood, hypoparathyroidism which might result in low calcium levels in the blood, chondrocalcinosis, spasticity and tetany, migraines,[16] epileptic seizures,[17] The diagnosis is typically based on finding low blood magnesium levels (hypomagnesemia).[18] basal ganglia calcifications[19] and in extreme and prolonged cases coma, intellectual disability or death.[20] Magnesium plays an important role in carbohydrate metabolism and its deficiency may worsen insulin resistance, a condition that often precedes diabetes, or may be a consequence of insulin resistance.[21] Normal magnesium levels are between 0.6 and 1.1 mmol/L (1.46–2.68 mg/dL) with levels less than 0.6 mmol/L (1.46 mg/dL) defining hypomagnesemia.[22] Specific electrocardiogram (ECG) changes may be seen.[22] | Causes include low dietary intake, alcoholism, diarrhea, increased urinary loss, poor absorption from the intestines, and diabetes mellitus.[23][24][25] A number of medications may also cause low magnesium, including proton pump inhibitors (PPIs) and furosemide.[26] |
| Molybdenum deficiency | High blood methionine, low blood uric acid, and low urinary uric acid and sulfate concentrations. | The amount of molybdenum required is relatively small, and molybdenum deficiency usually does not occur in natural settings.[27] |
| Potassium deficiency | Mild low potassium does not typically cause symptoms.[28] Symptoms may include feeling tired, leg cramps, weakness, and constipation.[22] Low potassium also increases the risk of an abnormal heart rhythm, which is often too slow and can cause cardiac arrest.[22][28] | Causes of potassium deficiencyinclude vomiting, diarrhea, medications like furosemide and steroids, dialysis, diabetes insipidus, hyperaldosteronism, hypomagnesemia, and not enough intake in the diet.[22] Normal potassium levels are between 3.5 and 5.0 mmol/L (3.5 and 5.0 mEq/L) with levels below 3.5 mmol/L defined as hypokalemia.[22][29] It is classified as severe when levels are less than 2.5 mmol/L.[22] Low levels may also be suspected based on an electrocardiogram (ECG).[22] Hyperkalemia is a high level of potassium in the blood serum.[22] |
| Selenium deficiency | Significant negative results,[30] affecting the health of the heart and the nervous system; contributing to depression, anxiety, and dementia; and interfering with reproduction and gestation. | People dependent on food grown from selenium-deficient soil may be at risk for deficiency.[31] |
| Sodium deficiency | Mild symptoms include a decreased ability to think, headaches, nausea, and poor balance.[32][33] Severe symptoms include confusion, seizures, and coma.[32][34][35] | The causes of hyponatremia are typically classified by a person's body fluid status into low volume, normal volume, or high volume.[36] Low volume hyponatremia can occur from diarrhea, vomiting, diuretics, and sweating.[36] Normal volume hyponatremia is divided into cases with dilute urine and concentrated urine.[36] Cases in which the urine is dilute include adrenal insufficiency, hypothyroidism, and drinking too much water or too much beer.[36] Cases in which the urine is concentrated include syndrome of inappropriate antidiuretic hormone secretion (SIADH).[36] High volume hyponatremia can occur from heart failure, liver failure, and kidney failure.[36] Conditions that can lead to falsely low sodium measurements include high blood protein levels such as in multiple myeloma, high blood fat levels, and high blood sugar.[37][38] |
| Zinc deficiency | Common symptoms include increased rates of diarrhea. Zinc deficiency affects the skin and gastrointestinal tract; brain and central nervous system, immune, skeletal, and reproductive systems. | Zinc deficiency in humans is caused by reduced dietary intake, inadequate absorption, increased loss, or increased body system use. The most common cause is reduced dietary intake. In the U.S., the Recommended Dietary Allowance (RDA) is 8 mg/day for women and 11 mg/day for men.[39] |
See also
References
- ↑ "Introduction: Mineral Deficiency and Toxicity: Merck Manual Professional". Archived from the original on 2009-02-01. Retrieved 2008-11-29.
- 1 2 Murphy, E; Williams (2009). "Hypocalcemia". Medicine. 37 (9): 465–468. doi:10.1016/j.mpmed.2009.06.003.
- ↑ Freund, Herbert; Atamian, Susan; Fischer, Josef E. (February 1979). "Chromium deficiency during total parenteral nutrition". JAMA. 241 (5): 496–498. doi:10.1001/jama.1979.03290310036012. PMID 104057.
- 1 2 "Chromium". NCBI Bookshelf. 2022-03-15. Archived from the original on 2021-01-24. Retrieved 2022-03-15.
- ↑ "Overview on Dietary Reference Values for the EU population as derived by the EFSA Panel on Dietetic Products, Nutrition and Allergies" (PDF). 2017. Archived (PDF) from the original on 2017-08-28. Retrieved 2022-04-23.
- ↑ Costello, Rebecca B.; Dwyer, Johanna T.; Bailey, Regan L. (2022-01-27). "Chromium supplements for glycemic control in type 2 diabetes: limited evidence of effectiveness". Nutrition Reviews. 74 (7). doi:10.1093/nutrit/nuw011. PMID 27261273. Archived from the original on 2022-03-15. Retrieved 2022-03-15.
- ↑ Onakpoya I, Posadzki P, Ernst E (2013). "Chromium supplementation in overweight and obesity: a systematic review and meta-analysis of randomized clinical trials". Obes Rev. 14 (6): 496–507. doi:10.1111/obr.12026. PMID 23495911.
- ↑ Scheiber, Ivo; Dringen, Ralf; Mercer, Julian F. B. (2013). "Chapter 11. Copper: Effects of Deficiency and Overload". In Astrid Sigel, Helmut Sigel and Roland K. O. Sigel (ed.). Interrelations between Essential Metal Ions and Human Diseases. Metal Ions in Life Sciences. Vol. 13. Springer. pp. 359–387. doi:10.1007/978-94-007-7500-8_11. PMID 24470097.
- ↑ Halfdanarson, Thorvardur R.; Kumar, Neeraj; Li, Chin-Yang; Phyliky, Robert L.; Hogan, William J. (2008-02-13). "Hematological manifestations of copper deficiency: a retrospective review". European Journal of Haematology. Wiley. 80 (6): 523–531. doi:10.1111/j.1600-0609.2008.01050.x. ISSN 0902-4441.
- ↑ Olivares M, Uauy R (2004). "Essential nutrients in drinking-water (Draft)" (PDF). WHO. Archived from the original (PDF) on 2012-10-19. Retrieved 2008-12-30.
- ↑ Pizzo G, Piscopo MR, Pizzo I, Giuliana G (September 2007). "Community water fluoridation and caries prevention: a critical review". Clin Oral Investig. 11 (3): 189–93. doi:10.1007/s00784-007-0111-6. PMID 17333303. S2CID 13189520.
- ↑ Rangarajan S, D'Souza GA (April 2007). "Restless legs syndrome in Indian patients having iron deficiency anemia in a tertiary care hospital". Sleep Medicine. 8 (3): 247–51. doi:10.1016/j.sleep.2006.10.004. PMID 17368978.
- ↑ "What We Eat In America, NHANES 2013–2014" (PDF). National Health and Nutrition Examination Survey (NHANES). US Department of Agriculture, Agricultural Research Service. Archived (PDF) from the original on 2017-02-24. Retrieved 2022-04-23.
- ↑ Creswell J. Eastman; Michael Zimmermann (12 February 2014). "The Iodine Deficiency Disorders". Thyroid Disease Manager. Archived from the original on 2016-12-12. Retrieved 2016-12-11.
- ↑ Keen, C.L.; Zidenberg-Cherr, S. (1996). "Manganese". In Ziegler, E.E.; Filer, L.J. (eds.). Present Knowledge in Nutrition (7th ed.). ILSI Press. pp. 334–343. ISBN 9780944398722.
- ↑ "Finding the Best Magnesium Supplements for Migraine". Migraine Again. 2021-04-26. Archived from the original on 2021-06-03. Retrieved 2021-06-03.
- ↑ Yuen, Alan W.C.; Sander, Josemir W. (2012-06-01). "Can magnesium supplementation reduce seizures in people with epilepsy? A hypothesis". Epilepsy Research. 100 (1–2): 152–156. doi:10.1016/j.eplepsyres.2012.02.004. ISSN 0920-1211. PMID 22406257. S2CID 23147775. Archived from the original on 2022-03-15. Retrieved 2022-04-23.
- ↑ Goldman, Lee; Schafer, Andrew I. (2015). Goldman-Cecil Medicine E-Book. Elsevier Health Sciences. p. 775. ISBN 9780323322850. Archived from the original on 2022-03-18. Retrieved 2022-04-23.
- ↑ "Basal Ganglia Calcification with Hypomagnesemia". www.japi.org. Archived from the original on 2022-06-30. Retrieved 2021-06-03.
- ↑ Viering, Daan H. H. M.; Baaij, Jeroen H. F. de; Walsh, Stephen B.; Kleta, Robert; Bockenhauer, Detlef (2016-05-27). "Genetic causes of hypomagnesemia, a clinical overview". Pediatric Nephrology. 32 (7): 1123–1135. doi:10.1007/s00467-016-3416-3. ISSN 0931-041X. PMC 5440500. PMID 27234911.
- ↑ Kobrin, SM; Goldfarb, S (Nov 1990). "Magnesium deficiency". Seminars in Nephrology. 10 (6): 525–35. PMID 2255809.
- 1 2 3 4 5 6 7 8 9 Soar, J; Perkins, GD; Abbas, G; Alfonzo, A; Barelli, A; Bierens, JJ; Brugger, H; Deakin, CD; Dunning, J; Georgiou, M; Handley, AJ; Lockey, DJ; Paal, P; Sandroni, C; Thies, KC; Zideman, DA; Nolan, JP (October 2010). "European Resuscitation Council Guidelines for Resuscitation 2010 Section 8. Cardiac arrest in special circumstances: Electrolyte abnormalities, poisoning, drowning, accidental hypothermia, hyperthermia, asthma, anaphylaxis, cardiac surgery, trauma, pregnancy, electrocution". Resuscitation. 81 (10): 1400–33. doi:10.1016/j.resuscitation.2010.08.015. PMID 20956045.
- ↑ Soar, J; Perkins, GD; Abbas, G; Alfonzo, A; Barelli, A; Bierens, JJ; Brugger, H; Deakin, CD; Dunning, J; Georgiou, M; Handley, AJ; Lockey, DJ; Paal, P; Sandroni, C; Thies, KC; Zideman, DA; Nolan, JP (October 2010). "European Resuscitation Council Guidelines for Resuscitation 2010 Section 8. Cardiac arrest in special circumstances: Electrolyte abnormalities, poisoning, drowning, accidental hypothermia, hyperthermia, asthma, anaphylaxis, cardiac surgery, trauma, pregnancy, electrocution". Resuscitation. 81 (10): 1400–33. doi:10.1016/j.resuscitation.2010.08.015. PMID 20956045.
- ↑ de Baaij JH, Hoenderop JG, Bindels RJ (January 2015). "Magnesium in man: implications for health and disease". Physiol. Rev. 95 (1): 1–46. CiteSeerX 10.1.1.668.9777. doi:10.1152/physrev.00012.2014. PMID 25540137.
- ↑ Gommers LM, Hoenderop JG, Bindels RJ, de Baaij JH (January 2016). "Hypomagnesemia in Type 2 Diabetes: A Vicious Circle?". Diabetes. 65 (1): 3–13. doi:10.2337/db15-1028. PMID 26696633.
- ↑ III, James L. Lewis (2021-09-29). "Hypomagnesemia - Endocrine and Metabolic Disorders". Merck Manuals Professional Edition (in Deutsch). Archived from the original on 2018-10-19. Retrieved 2022-03-15.
- ↑ "Molybdenum". Linus Pauling Institute. Oregon State University. Archived from the original on 2015-03-23. Retrieved 2008-11-29.
- 1 2 Zieg, J; Gonsorcikova, L; Landau, D (July 2016). "Current views on the diagnosis and management of hypokalaemia in children". Acta Paediatrica. 105 (7): 762–72. doi:10.1111/apa.13398. PMID 26972906. S2CID 19579505.
- ↑ Pathy, M.S. John (2006). "Appendix 1: Conversion of SI Units to Standard Units". Principles and Practice of Geriatric Medicine. Vol. 2 (4. ed.). Chichester: Wiley. p. Appendix. doi:10.1002/047009057X.app01. ISBN 9780470090558.
- ↑ Kieliszek, Marek (3 April 2019). "Selenium–Fascinating Microelement, Properties and Sources in Food". Molecules. 24 (7). doi:10.3390/molecules24071298. PMC 6480557. PMID 30987088.
- ↑ "Selenium Deficiency". Healthline. Archived from the original on 26 May 2020. Retrieved 10 May 2020.
- 1 2 Babar, S. (October 2013). "SIADH Associated With Ciprofloxacin" (PDF). The Annals of Pharmacotherapy. 47 (10): 1359–63. doi:10.1177/1060028013502457. ISSN 1060-0280. PMID 24259701. S2CID 36759747. Archived from the original (PDF) on May 1, 2015. Retrieved November 18, 2013.
- ↑ Henry, DA (4 August 2015). "In The Clinic: Hyponatremia". Annals of Internal Medicine. 163 (3): ITC1–19. doi:10.7326/aitc201508040. PMID 26237763. S2CID 12434550.
- ↑ Williams, DM; Gallagher, M; Handley, J; Stephens, JW (July 2016). "The clinical management of hyponatraemia". Postgraduate Medical Journal. 92 (1089): 407–11. doi:10.1136/postgradmedj-2015-133740. PMID 27044859.
- ↑ Ball, S; De Groot, LJ; Beck-Peccoz, P; Chrousos, G; Dungan, K; Grossman, A; Hershman, JM; Koch, C; McLachlan, R; New, M; Rebar, R; Singer, F; Vinik, A; Weickert, MO (2000). "Hyponatremia". Endotext. PMID 25905359. Accessed 1 August 2016.
- 1 2 3 4 5 6 Lee, JJ; Kilonzo, K; Nistico, A; Yeates, K (13 May 2014). "Management of hyponatremia". CMAJ : Canadian Medical Association Journal. 186 (8): E281–86. doi:10.1503/cmaj.120887. PMC 4016091. PMID 24344146.
- ↑ Filippatos, TD; Liamis, G; Christopoulou, F; Elisaf, MS (April 2016). "Ten common pitfalls in the evaluation of patients with hyponatremia". European Journal of Internal Medicine. 29: 22–25. doi:10.1016/j.ejim.2015.11.022. PMID 26706473.
- ↑ Marx, John; Walls, Ron; Hockberger, Robert (2013). Rosen's Emergency Medicine – Concepts and Clinical Practice (8 ed.). Elsevier Health Sciences. pp. 1639–42. ISBN 978-1455749874. Archived from the original on 2016-08-15.
- ↑ "Zinc" Archived 19 September 2017 at the Wayback Machine, pp. 442–501 in Dietary Reference Intakes for Vitamin A, Vitamin K, Arsenic, Boron, Chromium, Copper, Iodine, Iron, Manganese, Molybdenum, Nickel, Silicon, Vanadium, and Zinc. National Academy Press. 2001.
External links
| Classification |
|---|
This article is issued from Offline. The text is licensed under Creative Commons - Attribution - Sharealike. Additional terms may apply for the media files.