Osteopoikilosis
| Osteopoikilosis | |
|---|---|
 | |
| Osteopoikilosis on an X-ray of the hands | |
Osteopoikilosis is a benign, autosomal dominant sclerosing dysplasia of bone characterized by the presence of numerous bone islands in the skeleton.[1]
Signs and symptoms
Osteopoikilosis is usually asymptomatic, though pain is possible[2]
Cause
The etiology of Osteopoikilosis finds it is inherited in an autosomal dominant pattern, however osteopoikilosis can also happen in association with melorheostosis [2]
Diagnosis
In terms of the diagnosis Osteopoikilosis is radiographically evaluated via the presence of multiple symmetrical circular sclerotic opacities [2]
The radiographic appearance of osteopoikilosis on an X-ray is characterized by a pattern of numerous white densities of similar size spread throughout all the bones. This is a systemic condition. It must be differentiated from blastic metastasis, which can also present radiographically as white densities interspersed throughout bone. Blastic metastasis tends to present with larger and more irregular densities in less of a uniform pattern. Another differentiating factor is age, with blastic metastasis mostly affecting older people, and osteopoikilosis being found in people 20 years of age and younger.
The distribution is variable, though it does not tend to affect the ribs, spine, or skull.[3]
 a-c)Osteopoikilosis in feet, hand, knee
a-c)Osteopoikilosis in feet, hand, knee Osteopoikilosis of the hips on CT.
Osteopoikilosis of the hips on CT. Osteopoikilosis
Osteopoikilosis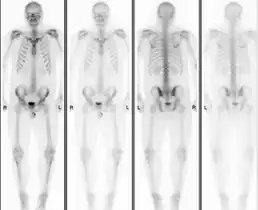 Normal bone scan in a person with osteopoikilosis
Normal bone scan in a person with osteopoikilosis
Treatment
The management of Osteopoikilosis is done via NSAIDs when needed[4]
Epidemiology
Men and women are affected in equal number,[5] reflecting the fact that osteopoikilosis attacks indiscriminately. Additionally, the disease is often associated with melorheostosis,[6] despite the apparent lack of correlation between melorheostosis and genetic heritability. It has been tied to LEMD3.[7] Buschke–Ollendorff syndrome is a similar condition,[8] which is also associated with LEMD3.[9]
See also
References
- ↑ Bull M, Calderbank P, Ramachandran N (2007). "A cause for concern? Osteopoikilosis found incidentally in the emergency department: a case report". Emerg Med J. 24 (5): e29. doi:10.1136/emj.2006.045765. PMC 2658513. PMID 17452689.
- 1 2 3 Stark, Z; Savarirayan, R (20 February 2009). "Osteopetrosis". Orphanet journal of rare diseases. 4: 5. doi:10.1186/1750-1172-4-5. PMID 19232111. Archived from the original on 8 March 2023. Retrieved 31 July 2023.
- ↑ Balan, Nisha Sharma, Anu (2008). Get through FRCR part 2B : rapid reporting of plain radiographs. London: Royal Society of Medicine. ISBN 978-1853157547.
- ↑ Jain, Anil K. (1 January 2016). Turek’s Orthopaedics Principles and Their Applications. Wolters kluwer india Pvt Ltd. p. 412. ISBN 978-93-5129-510-5. Archived from the original on 2 August 2023. Retrieved 31 July 2023.
- ↑ Serdaroğlu M, Capkin E, Uçüncü F, Tosun M (2007). "Case report of a patient with osteopoikilosis". Rheumatol. Int. 27 (7): 683–6. doi:10.1007/s00296-006-0262-9. PMID 17106662. S2CID 20299738.
- ↑ Nevin NC, Thomas PS, Davis RI, Cowie GH (1999). "Melorheostosis in a family with autosomal dominant osteopoikilosis". Am. J. Med. Genet. 82 (5): 409–14. doi:10.1002/(SICI)1096-8628(19990219)82:5<409::AID-AJMG10>3.0.CO;2-2. PMID 10069713.
- ↑ Hellemans J, Preobrazhenska O, Willaert A, et al. (2004). "Loss-of-function mutations in LEMD3 result in osteopoikilosis, Buschke–Ollendorff syndrome and melorheostosis". Nat. Genet. 36 (11): 1213–8. doi:10.1038/ng1453. PMID 15489854.
- ↑ synd/1803 at Who Named It?
- ↑ Mumm S, Wenkert D, Zhang X, McAlister WH, Mier RJ, Whyte MP (2007). "Deactivating germline mutations in LEMD3 cause osteopoikilosis and Buschke–Ollendorff syndrome, but not sporadic melorheostosis". J. Bone Miner. Res. 22 (2): 243–50. doi:10.1359/jbmr.061102. PMID 17087626. S2CID 28338454.
External links
| Classification | |
|---|---|
| External resources |