Buschke–Ollendorff syndrome
| Buschke–Ollendorff sign | |
|---|---|
| Other names: Dermatofibrosis lenticularis disseminata[1] | |
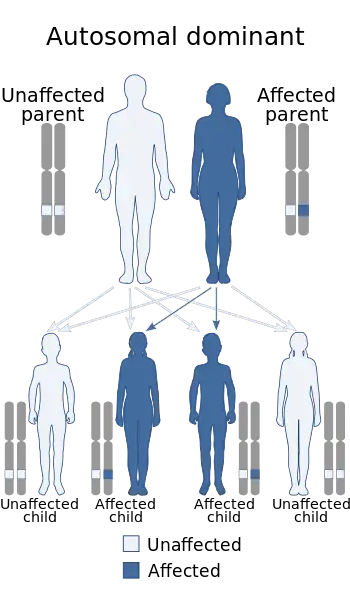 | |
| Buschke–Ollendorff syndrome has an autosomal dominant pattern of inheritance. | |
| Specialty | Dermatology |
| Symptoms | Widespread small bumps in skin[2] |
| Complications | Otosclerosis[1] |
| Usual onset | Children, adolescence[1] |
| Causes | Mutations in the LEMD3 gene.[3] |
| Diagnostic method | X-ray, ultrasound[4] |
| Differential diagnosis | Tuberous sclerosis, pseudoxanthoma elasticum, neurofibroma, lipoma[1] |
| Treatment | Surgery for hearing loss(or complications)[5] |
| Prognosis | Typically benign[1] |
| Frequency | Rare[1] |
Buschke–Ollendorff syndrome (BOS) is an inherited skin condition that presents with widespread small bumps, some of which merge to form thicker areas.[2] The trunk and limbs are most frequently affected.[2]
It is a genetic disorder associated with LEMD3.[6][7] It is inherited in an autosomal dominant manner.[2] In a very few, X-rays may show several areas of compact bone.[1] Conditions that may appear similar include tuberous sclerosis, pseudoxanthoma elasticum, neurofibroma, and lipoma, among others.[1]
The condition is rare.[7] Its frequency is almost 1 case per every 20,000 people, and it is equally found in both males and females.[5] It is named for Abraham Buschke and Helene Ollendorff Curth, who described it in 1928.[6][8]
Signs and symptoms
The signs and symptoms of this condition are consistent with the following (possible complications include aortic stenosis and hearing loss[3][5]):
- Osteopoikilosis
- Bone pain
- Connective tissue nevi
- Metaphysis abnormality
Pathogenesis
Buschke–Ollendorff syndrome is caused by one important factor: mutations in the LEMD3 gene (12q14), located on chromosome 12.
Among the important aspects of Buschke–Ollendorff syndrome condition, genetically speaking are:[9][10][11]
.jpg.webp)
- LEMD3 (protein) referred also as MAN1, is an important protein in inner nuclear membrane.
- LEMD3 gene gives instructions for producing protein that controls signaling for transforming growth factor-beta.
- LEMD3 gene helps in the bone morphogenic protein pathway
- Both of the above pathways help grow new bone cells
- BMP and TGF-β pathways controls SMADs proteins, which then bind to DNA
- LEMD3 once mutated, causes a reduction of the protein, which in turn causes excess of the above two pathways.
Diagnosis

The diagnosis of this condition can be ascertained via several techniques one such method is genetic testing, as well as:[3][4]
- X-ray
- Ultrasound
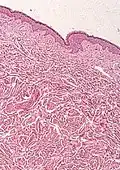
- Histological test
 Osteopoikilosis
Osteopoikilosis Osteopoikilosis
Osteopoikilosis Melorheostosis
Melorheostosis
Differential diagnosis
The differential diagnosis for an individual believed to have Buschke–Ollendorff syndrome is the following:[4]
- Melorheostosis
- Sclerotic bone metastases.
Treatment
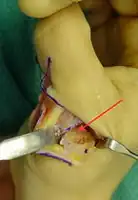
In terms of the treatment of Buschke–Ollendorff syndrome, should the complication of aortic stenosis occur then surgery may be required. [5]
Treatment for hearing loss may also require surgical intervention.[5]
 Note thickened sclerotic cortical bone
Note thickened sclerotic cortical bone
See also
References
- 1 2 3 4 5 6 7 8 Lacour, Marc (4 December 2019). "95. Buschke–Ollendorff syndrome, Marfan's syndrome and osteogenesis imperfecta". In Hoeger, Peter H.; Kinsler, Veronica; Yan, Albert C.; Bodemer, Christine; Larralde, Margarita; Luk, David; Mendiratta, Vibhu; Purvis, Diana (eds.). Harper's Textbook of Pediatric Dermatology. John Wiley & Sons. p. 1139. ISBN 978-1-119-14280-5.
- 1 2 3 4 James, William D.; Elston, Dirk; Treat, James R.; Rosenbach, Misha A.; Neuhaus, Isaac (2020). "28. Dermal and subcutaneous tumors". Andrews' Diseases of the Skin: Clinical Dermatology (13th ed.). Edinburgh: Elsevier. pp. 614–615. ISBN 978-0-323-54753-6. Archived from the original on 2023-07-30. Retrieved 2023-07-29.
- 1 2 3 "Buschke Ollendorff syndrome | Genetic and Rare Diseases Information Center (GARD) – an NCATS Program". rarediseases.info.nih.gov. Archived from the original on 31 July 2018. Retrieved 29 December 2017.
- 1 2 3 RESERVED, INSERM US14 -- ALL RIGHTS. "Orphanet: Buschke Ollendorff syndrome". www.orpha.net. Archived from the original on 31 July 2018. Retrieved 29 December 2017.
- 1 2 3 4 5 Lukasz Matusiak (2 July 2008), Dermatofibrosis Lenticularis (Buschke–Ollendorf Syndrome), eMedicine, archived from the original on 2019-07-27, retrieved 2009-09-05
- 1 2 Guzman, Anthony K.; James, William D. (September 2016). "Helen Ollendorff-Curth: A dermatologist's lasting legacy". International Journal of Women's Dermatology. 2 (3): 108–112. doi:10.1016/j.ijwd.2016.06.002. ISSN 2352-6475. PMID 28492020. Archived from the original on 2023-03-02. Retrieved 2023-07-29.
- 1 2 Online Mendelian Inheritance in Man (OMIM): 166700
- ↑ A. Buschke, H. Ollendorff-Curth. Ein Fall von Dermatofibrosis lenticularis disseminata und Osteopathia condensans disseminata. Dermatologische Wochenschrift, Hamburg, 1928, 86: 257–262.
- ↑ Reference, Genetics Home. "Buschke-Ollendorff syndrome". Genetics Home Reference. Archived from the original on 2019-04-11. Retrieved 2018-05-13.
- ↑ Worman, Howard J.; Fong, Loren G.; Muchir, Antoine; Young, Stephen G. (July 2009). "Laminopathies and the long strange trip from basic cell biology to therapy". The Journal of Clinical Investigation. 119 (7): 1825–1836. doi:10.1172/JCI37679. ISSN 1558-8238. PMC 2701866. PMID 19587457. Archived from the original on 13 December 2019. Retrieved 13 May 2018.
- ↑ Reference, Genetics Home. "LEMD3 gene". Genetics Home Reference. Archived from the original on 2018-07-02. Retrieved 2018-05-13.
- ↑ Hosen, Mohammad J.; Lamoen, Anouck; De Paepe, Anne; Vanakker, Olivier M. (2012). "Histopathology of Pseudoxanthoma Elasticum and Related Disorders: Histological Hallmarks and Diagnostic Clues". Scientifica. 2012: 1–15. doi:10.6064/2012/598262. ISSN 2090-908X. PMC 3820553. PMID 24278718.
-Creative Commons Attribution 3.0 Unported Archived 2011-02-23 at the Wayback Machine license
Further reading
- Pope, V.; Dupuis, L.; Kannu, P.; Mendoza-Londono, R.; Sajic, D.; So, J.; Yoon, G.; Lara-Corrales, I. (2016). "Buschke-Ollendorff syndrome: a novel case series and systematic review". The British Journal of Dermatology. 174 (4): 723–729. doi:10.1111/bjd.14366. ISSN 1365-2133. PMID 26708699. S2CID 24066368.
- Helander, Martti Kormano, Ilmari Lindgren; with the collaboration of Inkeri; Lindgren, Ilmari (1999). Radiological findings in skin diseases and related conditions. Stuttgart: Thieme. ISBN 9783131161215. Archived from the original on 29 August 2021. Retrieved 3 February 2018.
External links
| Classification | |
|---|---|
| External resources |
|