Pilocytic astrocytoma
| Pilocytic astrocytoma | |
|---|---|
| Other names: Juvenile pilocytic astrocytoma or Cystic cerebellar astrocytoma | |
 | |
| Micrograph of a pilocytic astrocytoma, showing characteristic bipolar cells with long pilocytic (hair-like) processes. Smear preparation. H&E stain. | |
| Specialty | Neuro-oncology |
Pilocytic astrocytoma (and its variant pilomyxoid astrocytoma) is a brain tumor that occurs most commonly in children and young adults (in the first 20 years of life). They usually arise in the cerebellum, near the brainstem, in the hypothalamic region, or the optic chiasm, but they may occur in any area where astrocytes are present, including the cerebral hemispheres and the spinal cord. These tumors are usually slow growing and benign, corresponding to WHO malignancy grade 1.[1]
Signs and symptoms
Children affected by pilocytic astrocytoma can present with different symptoms that might include failure to thrive (lack of appropriate weight gain/ weight loss), headache, nausea, vomiting, irritability, torticollis (tilt neck or wry neck), difficulty to coordinate movements, and visual complaints (including nystagmus). The complaints may vary depending on the location and size of the neoplasm. The most common symptoms are associated with increased intracranial pressure due to the size of the tumor mass.[2]
Causes
Pilocytic astrocytoma can be associated with the genetic condition neurofibromatosis type 1 (NF1), and optic nerve gliomas are among the most frequently encountered tumors in patients with this disorder. The majority of pilocytic astrocytomas, however, arise sporadically - with no evidence of a link to an underlying hereditary predisposition or lifestyle factor. They are associated with genetic alterations in the MAPK/ERK pathway, most frequently a characteristic KIAA1549-BRAF fusion gene.[3][4]
Diagnosis
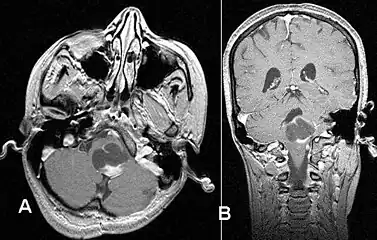 Stereotactic MRI brain scan showing a recurrent postoperative brain stem cystic pilocytic astrocytoma.
Stereotactic MRI brain scan showing a recurrent postoperative brain stem cystic pilocytic astrocytoma. Pilocytic astrocytoma in the hypothalamic region.
Pilocytic astrocytoma in the hypothalamic region.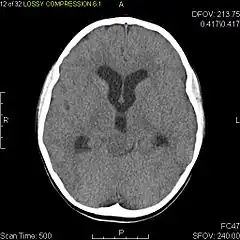 Axial non-contrast CT in a nine-year-old girl showing a slightly hypodense mass in the tectum of the brainstem, compressing the aqueduct of Sylvius and causing obstructive hydrocephalus
Axial non-contrast CT in a nine-year-old girl showing a slightly hypodense mass in the tectum of the brainstem, compressing the aqueduct of Sylvius and causing obstructive hydrocephalus Sagittal T1-weighted MRI showing a well-circumscribed hypointense mass in the tectum (presumably a tectal plate glioma). These lesions are a distinct subset of pilocytic astrocytoma which present with hydrocephalus typically in 6 to 10 year-olds and are rarely progressive lesions. When imaging is characteristic, a biopsy is usually not performed because of the risks to adjacent structures, often shunting to relieve intracranial pressure is the only treatment required.
Sagittal T1-weighted MRI showing a well-circumscribed hypointense mass in the tectum (presumably a tectal plate glioma). These lesions are a distinct subset of pilocytic astrocytoma which present with hydrocephalus typically in 6 to 10 year-olds and are rarely progressive lesions. When imaging is characteristic, a biopsy is usually not performed because of the risks to adjacent structures, often shunting to relieve intracranial pressure is the only treatment required. T1-weighted coronal MRI image postcontrast showing heterogeneous contrast enhancement within the presumed tectal plate glioma
T1-weighted coronal MRI image postcontrast showing heterogeneous contrast enhancement within the presumed tectal plate glioma
Usually – depending on the interview of the patient and after a clinical exam which includes a neurological exam and an ophthalmological exam – a CT scan and/or an MRI scan will be performed to confirm the presence of a tumor. They are usually easily distinguishable from normal brain structures using these imaging techniques. A special dye may be injected into a vein before these scans to provide contrast and make tumors easier to identify. Pilocytic astrocytomas are typically clearly visible on such scans, but it is often difficult to say based on imaging alone what type of tumor is present.
If a tumor is found, it will be necessary for a neurosurgeon to perform a biopsy of it. This involves the removal of a small amount of tumorous tissue, which is then sent to a (neuro)pathologist for examination and staging.[5] The biopsy may take place before surgical removal of the tumor, or the sample may be taken during surgery to remove the bulk of the tumor.
Microscopic appearance
Pilocytic astrocytomas are often cystic tumors, and, if solid, tend to be well-circumscribed.
Under the microscope, the tumor is seen to be composed of bipolar cells with long "hair-like" GFAP-positive processes, giving the designation "pilocytic" (that is, made up of cells that look like fibers when viewed under a microscope[6]). Some pilocytic astrocytomas may be more fibrillary and dense in composition. The presence of Rosenthal fibers,[7] eosinophilic granular bodies, and microcysts can often be seen. Myxoid foci and oligodendroglioma-like cells may also be present, though these are not specific to pilocytic astrocytoma. Long-standing lesions may show hemosiderin-laden macrophages and calcifications.
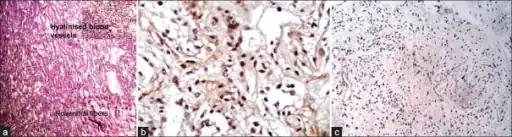 a-c) Photomicrograph shows microcystic areas in pilocytic astrocytoma
a-c) Photomicrograph shows microcystic areas in pilocytic astrocytoma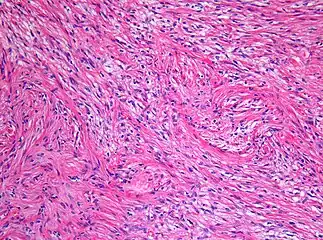 Histopathology of pilocytic astrocytoma (grade I WHO).
Histopathology of pilocytic astrocytoma (grade I WHO).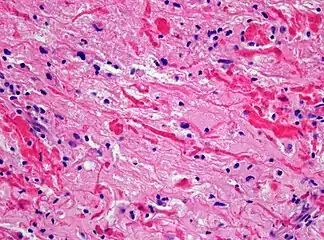 Histopathology of Rosenthal-fibres. H&E staining showing these elongated eosinophilic structures in the case of pilocytic astrocytoma.
Histopathology of Rosenthal-fibres. H&E staining showing these elongated eosinophilic structures in the case of pilocytic astrocytoma.
Treatment
The most common form of treatment is having the tumor surgically removed. Complete removal of the tumor will generally allow functional survival for many years.[8] In particular for pilocytic astrocytomas (commonly indolent masses that may permit normal neurologic function), surgeons may decide to monitor the neoplasm's evolution and postpone surgical intervention for some time. However, total resection is often not possible. The location could prohibit access to the neoplasm and lead to incomplete or no resection at all. Left unattended, these tumors may eventually lead to further symptoms due to continued slow growth. Extremely rarely, they may also undergo malignant transformation.
If surgery is not possible, recommendations such as chemotherapy or radiation may be suggested. However, side effects from these treatments can be extensive and long term, resulting in some cases in life-long difficulties.[9][10]
Side effects
After treatment, children with pilocytic astrocytoma may experience an improvement of symptoms related to the tumor itself depending on the location, but may also experience side effects related to the treatment:
- Symptoms related to increased pressure in the brain often disappear after surgical removal of the tumor.
- Effects on coordination and balance may improve and might progressively (to completely) disappear as recovery progresses.
- Steroid treatment is often used to control tissue swelling that may occur pre-and post-operatively.
- Patients can, however, also develop long-term side effects due to the type of treatment they may receive.
Prognosis
In keeping with their assignment as WHO grade 1, pilocytic astrocytoma is not usually associated with recurrence after complete resection. The pilomyxoid astrocytoma variant may behave more aggressively than classic pilocytic astrocytoma, but this might also be associated with the younger age at presentation and their more frequent midline location.
In cases of progressive/recurrent disease or when maximal surgical removal has been achieved but some residual tumor remains, chemotherapy and/or radiation therapy may be considered by the medical team.[11]
Incidence
Regularly updated statistics about the incidence, epidemiology, and survival outcomes of brain tumors can be found in the annual reports of the Central Brain Tumor Registry of the United States (CBTRUS).[12] These figures suggest that an average of just over 1,000 pilocytic astrocytomas are diagnosed per year in the US, representing about 1% of all CNS tumors. In children, however, the proportion is much higher. Pilocytic astrocytoma is the single most common childhood brain tumor, accounting for almost 20% of brain tumors diagnosed in 0-14 year-olds, with a peak incidence between 5–14 years of age.[13]
References
- ↑ Louis, David N.; Ohgaki, Hiroko; Wiestler, Otmar D.; Cavenee, Webster K. (2016). WHO classification of tumours of the central nervous system (Revised 4th ed.). Lyon. ISBN 978-92-832-4492-9.
- ↑ "Pilocytic astrocytoma". National Center For Advancing Translational Sciences. Archived from the original on 11 July 2021. Retrieved 2 July 2021.
- ↑ Jones DT, Kocialkowski S, Liu L, Pearson DM, Bäcklund LM, Ichimura K, Collins VP (November 2008). "Tandem duplication producing a novel oncogenic BRAF fusion gene defines the majority of pilocytic astrocytomas". Cancer Research. 68 (21): 8673–8677. doi:10.1158/0008-5472.CAN-08-2097. PMC 2577184. PMID 18974108.
- ↑ Sadighi Z, Slopis J (May 2013). "Pilocytic astrocytoma: a disease with evolving molecular heterogeneity". Journal of Child Neurology. 28 (5): 625–632. doi:10.1177/0883073813476141. PMID 23439714. S2CID 8437596.
- ↑ "College of American Pathologists". Archived from the original on 2017-07-25. Retrieved 2022-10-21.
- ↑ National Cancer Institute > Dictionary of Cancer Terms > pilocytic Archived 2015-04-25 at the Wayback Machine Retrieved on July 16, 2010
- ↑ Wippold FJ, Perry A, Lennerz J (May 2006). "Neuropathology for the neuroradiologist: Rosenthal fibers". AJNR. American Journal of Neuroradiology. 27 (5): 958–961. PMC 7975751. PMID 16687524. Archived from the original on 2019-12-14. Retrieved 2022-10-21.
- ↑ Dodgshun AJ, Maixner WJ, Hansford JR, Sullivan MJ (May 2016). "Low rates of recurrence and slow progression of pediatric pilocytic astrocytoma after gross-total resection: justification for reducing surveillance imaging". Journal of Neurosurgery. Pediatrics. 17 (5): 569–572. doi:10.3171/2015.9.PEDS15449. PMID 26722760.
- ↑ Armstrong GT, Conklin HM, Huang S, Srivastava D, Sanford R, Ellison DW, et al. (February 2011). "Survival and long-term health and cognitive outcomes after low-grade glioma". Neuro-Oncology. 13 (2): 223–234. doi:10.1093/neuonc/noq178. PMC 3064628. PMID 21177781.
- ↑ Ris MD, Leisenring WM, Goodman P, Di C, Noll J, Levy W, et al. (September 2019). "Neuropsychological and socioeconomic outcomes in adult survivors of pediatric low-grade glioma". Cancer. 125 (17): 3050–3058. doi:10.1002/cncr.32186. PMC 6690772. PMID 31231797.
- ↑ "Astrocytoma". The Lecturio Medical Concept Library. Archived from the original on 9 July 2021. Retrieved 1 July 2021.
- ↑ "Central Brain Tumor Registry of the United States". CBTRUS. Archived from the original on 2022-10-13. Retrieved 2022-10-21.
- ↑ Ostrom QT, Patil N, Cioffi G, Waite K, Kruchko C, Barnholtz-Sloan JS (October 2020). "CBTRUS Statistical Report: Primary Brain and Other Central Nervous System Tumors Diagnosed in the United States in 2013-2017". Neuro-Oncology. 22 (12 Suppl 2): iv1–iv96. doi:10.1093/neuonc/noaa200. PMC 7596247. PMID 33123732.
External links
| Classification | |
|---|---|
| External resources |