Pseudoathletic appearance
| Pseudoathletic appearance | |
|---|---|
| Other names | Herculean appearance, Bodybuilder-like appearance |
 | |
Pseudoathletic appearance is a medical sign meaning to have the false appearance of a well-trained athlete due to pathology instead of true athleticism.[1][2] It is also referred to as a Herculean or bodybuilder-like appearance.[3] The pathology may be the result of muscle inflammation (swelling), muscle hyperplasia, muscle hypertrophy, muscle pseudohypertrophy (muscle atrophy with infiltration of fat or other tissue), or symmetrical subcutaneous (under the skin) deposits of fat or other tissue.
The mechanism resulting in this sign may stay consistent or may change, while the sign itself remains. For instance, some individuals with Duchenne and Becker muscular dystrophy may start with true muscle hypertrophy, but later develop into pseudohypertrophy.[4]
In healthy individuals, resistance training and heavy manual labour creates muscle hypertrophy through signalling from mechanical stimulation (mechanotransduction) and from sensing available energy reserves (such as AMP through AMP-activated protein kinase); however, in the absence of a sports or vocational explanation for muscle hypertrophy, especially with accompanying muscle symptoms such as myalgia, cramping, or exercise intolerance, then a neuromuscular disorder should be suspected.[5][6]
As muscle hypertrophy is a response to strenuous anaerobic activity, ordinary everyday activity would become strenuous in diseases that result in premature muscle fatigue (neural or metabolic), or disrupt the excitation-contraction coupling in muscle, or cause repetitive or sustained involuntary muscle contractions (fasciculations, myotonia, or spasticity).[5][6] In some forms of lipodystrophy, an abnormal deficit of subcutaneous fat accentuates the appearance of the muscles, though the muscles are quantifiably hypertrophic (possibly due to a metabolic abnormality).[7][8]
Diseases
Skeletal muscle
| Disease grouping | Disease | Muscle(s) typically affected | Age of onset | Biopsy, ultrasonography, CT scan or MRI |
|---|---|---|---|---|
| Hyperplasia | Myostatin-related muscle hypertrophy
(MSTN gene) |
General | Prenatal-onset | Myofibre hyperplasia and decreased adipose tissue. |
| Beckwith–Wiedemann syndrome | Macroglossia/ hemihypertrophy of limb or body | Prenatal to infantile-onset | Wide phenotypic variability. Macroglossia (enlarged tongue) and hemihyperplasia (enlargement on one side of the body) in general or an isolated limb.[9][10] | |
| Parasitic | Disseminated muscular cysticercosis syndrome[11] | General | Variable | Pork tapeworm cysts[11] |
| Trichinosis[10] | General | Variable | Skeletal muscle inflammation (myositis) secondary to roundworm cysts and larvae. | |
| Inflammation | Inflammatory myopathies
(Focal myositis, polymyositis, granulomatous myositis, inclusion body myositis) |
Calf muscle[12][13]/general | ||
| Sarcoid granulomas/Sarcoidosis | Calf muscle[12]/general | Inflammatory cells and deposits of sarcoid granulomas | ||
| Amyloid deposits/Amyloidosis
(Inflammatory protein serum amyloid A, or in association with inflammatory diseases) |
Calf muscle[12]/general[14] | Amyloid deposits[14] | ||
| Ossification | Fibrodysplasia ossificans progressiva
(formerly known as myositis ossificans progressiva) |
General | Episodic inflammatory flare-ups involving skeletal muscle (myositis) secondary to muscle tissue turning into bone (ossification)[10][15] | |
| Non-heriditary myositis ossificans | General | Episodic inflammatory flare-ups involving skeletal muscle (myositis) secondary to muscle tissue turning into bone (ossification) | ||
| Muscular dystrophy | Duchenne muscular dystrophy | Calf muscle/general[4] | Childhood-onset | Muscle hypertrophy may precede pseudohypertrophy by infiltration of fatty tissue[4] |
| Becker muscular dystrophy | Calf muscle/general[4][16] | Variable | Muscle hypertrophy may precede pseudohypertrophy by infiltration of fatty tissue[4] | |
| Facioscapulohumeral muscular dystrophy | Calf muscle[13] | |||
| Limb-girdle muscular dystrophy (LGMD) | Calf muscle[16][17] | Variable | Classic dystrophic changes include myonecrosis and regeneration, variations in muscle fibre size, myofibrosis, fatty infiltration (pseudohypertrophy).[17] LGMD1H shows histochemical evidence of defective oxidative phosphorylation and ragged red fibres, suggestive of a mitochondrial myopathy and since 2017 was excluded from LGMD (see below under metabolic myopathy).[18][19] | |
| Congenital muscular dystrophy-dystroglycanopathy types A, B, & C
(types A2, A4, B1, B2, B5, B6, C2, C3, C4, C5, C7, C8, C9, C12) |
Hypertrophy and/or pseudohypertrophy by fatty infiltration of muscle.[20][21][22] | |||
| Myopathy, X-linked, with postural muscle atrophy
(formerly Emery-Dreifuss muscular dystrophy 6, X-linked) |
Proximal muscles | Variable (late childhood to adult-onset) | Muscle hypertrophy precedes muscle atrophy. Biopsy shows myopathic or dystrophic changes, rimmed vacuoles, cytoplasmic bodies, and granulofilamentous material.[23] | |
| Miyoshi muscular dystrophy 3 | Calf muscles/extensor digitorum brevis muscles | Adult-onset | Muscle hypertrophy and/or pseudohypertrophy by infiltration of fatty tissue. Muscle hypertrophy precedes muscle atrophy.[24] | |
| Myopathy, vacuolar, with CASQ1 aggregates | Calf muscles | Adolescence to adult-onset | Calf muscle hypertrophy in some.[25] Muscle biopsy shows vacuoles predominantly in type II (fast-twitch/glycolytic) fibres, rare necrotic fibres, CASQ1-immunopositive inclusions, decreased density of calcium release units, abnormal sarcoplasmic reticulum elements, enlarged terminal cisternae of the sarcoplasmic reticulum, and enlarged vesicles of sarcoplasmic reticulum origin.[26] | |
| Myofibrillar myopathy 10 | Trapezius and latissimus dorsi muscles | Childhood to young adult-onset | Hypertrophic neck and shoulder girdle muscles. Muscle biopsy shows structural abnormalities, lobulated type I (slow-twitch/oxidative) muscle fibres, irregular intermyofibrillar network, autophagic vacuoles with lipoprotein deposits, and sarcolemmal abnormalities.[27] | |
| Non-dystrophic myotonias and pseudomyotonias
(delayed muscle relaxation) |
Myotonia congenita
(Chloride channelopathy, CLCN1 gene) |
Calf muscle/general[28][29] | ||
| Potassium-aggravated myotonia, paramyotonia congenita
(Sodium channelopathy, SCN4A gene) |
Calf muscle/general[28][29] | |||
| Brody disease | Calf muscle[28][30] | Variable[30] Commonly marked variability of muscle fibre size, type II (fast-twitch/glycolytic) muscle fibres may be abnormally increased or decreased, usually increased internal nuclei, rarely nuclear centralization or nuclear clumping. Muscle activity is electrically silent on EMG.[30] | ||
| Rippling muscle disease | Muscle hypertrophy. Muscle activity is electrically silent on EMG.[31][32] | |||
| Lipodystrophy | Familial partial lipodystrophy
(Köbberling–Dunnigan syndrome) |
Calf muscle/general[33][7] | Adolescence-onset | Hypertrophy of calf muscles[33][7] |
| Congenital generalized lipodystrophy
(Berardinelli-Seip syndrome) |
General[8] | Infantile-onset | Muscle hypertrophy[8] | |
| Spasticity | Spastic cerebral palsy | Calf muscle[34] | Childhood-onset | accumulation of hydroxyproline (aminoacid exclusive to collagen) in calf muscles[34] |
| Stiff-person syndrome | Torso/limbs | Muscle hypertrophy and EMG demonstrates co-contraction of agonist and antagonist muscles and/or continuous motor unit activity in affected muscles.[35][36] | ||
| Denervation (pseudo)hypertrophy | Peripheral nerve traumatic injury | Calf muscle[37] | Variable | |
| Disorders of the anterior horn cells (such as poliomyelitis, spinal muscular atrophy, and Charcot-Marie-Tooth disease) | Calf muscle[37] | |||
| Radiculopathy
(pinched nerve) |
Calf muscle[37]/thigh muscle[38] | Adult-onset | Variable. Fatty infiltration of calf muscle (pseudohypertrophy),[37] true hypertrophy of thigh muscle.[38] | |
| Endocrine myopathies | Kocher–Debre–Semelaigne syndrome | Calf muscle[12]/general | Childhood-onset | Muscle hypertrophy, abnormal glycogen accumulation (impaired glycogenolysis), mucopolysaccharide deposits, atrophy of type II (fast-twitch/glycolytic) muscle fibres. EMG normal or myopathic low amplitude and short MUAPs (motor unit action potentials),[39] decrease in muscle carnitine.[40] |
| Hoffmann syndrome | Calf muscle[12]/general | Adult-onset | Variable (with or without mucoid deposits).[12][41][42] Muscle hypertrophy, abnormal glycogen accumulation (impaired glycogenolysis), mucopolysaccharide deposits, atrophy of type II (fast-twitch/glycolytic) muscle fibres, damaged mitochondria. EMG may be normal, neuropathic, myopathic, or mixed type.[12][41][42] Decrease in muscle carnitine.[40] | |
| Denervation pseudohypertrophy of calf muscles secondary to diabetic neuropathy | Calf muscle[43] | Adult-onset | Fatty infiltration of calf muscles (pseudohypertrophy) and myofibrosis.[43] | |
| Acromegaly/Gigantism | General[10] | Muscle hypertrophy | ||
| Metabolic myopathies | Late-onset Pompe disease (Glycogen storage disease type II) | Calf muscle[44] | Variable (childhood to adulthood, but not infantile-onset) | Muscle hypertrophy, abnormal glycogen accumulation within the lysosomes of muscle cells due to impaired glycogenolysis.[44] |
| Cori/Forbes disease (Glycogen storage disease type III) | Sternocleidomastoid, trapezius and quadriceps muscles[45]/thigh muscles[5] | Variable | Hypertrophy[46] and pseudohypertrophy.[45][47] Abnormal glycogen accumulation within the cytosol of muscle cells due to impaired glycogenolysis.[47] | |
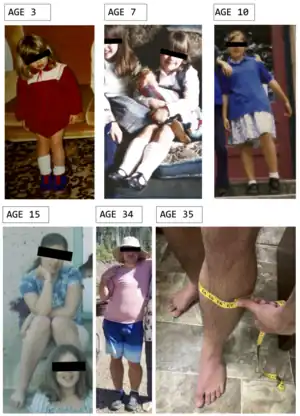
| McArdle disease (Glycogen storage disease type V) | Calf muscle[48][49]/deltoid and bicep muscles[49] | Childhood-onset | Muscle hypertrophy, lean calf muscles, abnormal glycogen accumulation within the cytosol of muscle cells due to impaired glycogenolysis.[48] | |
| Muscular dystrophy, limb-girdle, type 1H
(As of 2017 was excluded from LGMD, but not yet assigned new nomenclature)[19] |
Calf muscle[18] | Variable | Muscle hypertrophy, muscle fibre type variation, ragged red fibres, absence of cytochrome c oxidase staining, evidence of mtDNA deletions, defective oxidative phosphorylation suggestive of mitochondrial myopathy.[18] | |
| Malnutrition
(poor diet, malabsorption diseases, or drug side effect such as lipase inhibitor Orlistat)[50] |
Vitamin D deficiency myopathy
(also known as osteomalacic myopathy) |
Calf muscle[34] | Adult-onset (no rickets) | Muscle hypertrophy in rare cases.[34][13] Commonly abnormal glycogen accumulation (impaired glycogenolysis), atrophy of type II (fast-twitch/glycolytic) muscle fibres, enlarged inter-fibrillar spaces;[51][52] rarely infiltration of fat (pseudohypertrophy), and fibrosis.[51] EMG myopathic low amplitude, short duration polyphasic MUAPs (motor unit action potentials).[52] |
| Vitamin D deficiency myopathy secondary to Celiac disease | Calf muscle[34] | Adult-onset
(no rickets) |
||
| Congenital myopathies | Central core disease | Calf muscle[13] | ||
| Centronuclear myopathy | Calf muscle[13] | |||
| Congenital myopathy 9B, proximal, with minicore lesions | Calf muscle[53] | Infantile-onset | Pseudohypertrophy due to fatty infiltration. Biopsy shows type I (slow-twitch/oxidative) fibre predominance, increased internal nuclei, Z-band streaming, and minicores that disrupt the myofibrillar striation pattern.[53] | |
| Tubular aggregate myopathy types 1 & 2
(genes STIM1, ORAI1) |
Calf muscle[54] | Typically childhood-onset | Hypertrophy of type I and type II muscle fibres, type I (slow-twitch/oxidative) fibre predominance, fatty infiltration of affected muscles, tubular aggregates (TAs) mainly in type I fibres arranged in honeycomb-like structures (transversal sections) or aligned in parallel (longitudinal sections), internal nuclei, particulate glycogen scattered between tightly packed tubules, occasional lipofuscin granules within large TAs, EMG normal to myopathic.[55][54] Muscle oedema and fibrosis may accompany fatty infiltration.[56] | |
| Myosin myopathies and Laing distal myopathy
(gene MYH7) |
Laing distal myopathy
(Myopathy, distal, 1; MPD1) |
Calf muscle[57][58] | Variable. Typically childhood-onset | Wide phenotypic variability. Typically hypertrophic calf muscles, atrophy of anterior compartment tibial muscles, predominance of type I fibres and numerous small type I fibres. Common are internal nuclei, structural abnormalities (especially minicores), and mitochondrial abnormalities (ragged red fibres). Rarely muscle necrosis, protein aggregates, rimmed vacuoles, filamentous inclusions, muscle atrophy with fat or connective tissue replacement (pseudohypertrophy), cytoplasmic bodies, and myofibrillar alterations. EMG myopathic or neurogenic.[57][58] |
| Myosin storage myopathy
(Congenital myopathy 7A, myosin storage; CMYP7A) |
Calf muscle[57][59] | Variable. Typically childhood-onset | Wide phenotypic variability. Typically fatty infiltration of calf muscles (pseudohypertrophy), type I (slow-twitch/oxidative) fibre predominance, type I fibres have abnormalities (hyaline bodies and myosin protein aggregates), and generalized muscle atrophy. Other variable muscle biopsy findings may be seen in addition. EMG is myopathic.[57][59] | |
| Tumours | Infiltrating lipoma | Calf muscle[43] | Pseudohypertrophy | |
| Short stature | Myhre syndrome
(chronic denervation hypertrophy secondary to primary disease) |
General[10] | Childhood-onset | Muscle hypertrophy |
| Schwartz-Jampel syndrome | Infantile-onset | Muscle hypertrophy[60] | ||
| Uruguay faciocardiomusculoskeletal syndrome | Early childhood-onset | Muscle hypertrophy[61] | ||
| Nivelon-Nivelon-Mabille syndrome | Prenatal-onset | Muscle hypertrophy in some[62] | ||
| Satoyoshi syndrome | General | Childhood to early adolescence-onset | Muscle hypertrophy[63] | |
| Stormorken syndrome
(gene STIM1) |
Calf muscle[54] | Childhood-onset | Fatty infiltration of affected muscles, tubular aggregates (TAs) mainly in type I (slow-twitch/oxidative) fibres arranged in honeycomb-like structures (transversal sections) or aligned in parallel (longitudinal sections), type I (slow-twitch/oxidative) muscle fibre predominance, internal nuclei, [54] | |
| Face muscles | Masseter muscle hypertrophy | Masticatory muscles | Adolescence-onset | Muscle hypertrophy of the masticatory muscles (used for chewing food)[64] |
| Hemifacial myohyperplasia (HMH) | Unilateral facial expression muscles and/or masticatory muscles | Prenatal-onset | Unilateral (one side of the face) hyperplasia in the muscles controlling facial expression and/or mastication (chewing)[65][10] | |
| Other | Syringomyelia
(cyst or cavity within spinal cord) |
Upper limbs/calf muscle[66] | Muscle hypertrophy[66] | |
| Peripheral nerve hyperexcitability syndromes
(Neuromyotonia, Morvan syndrome, Benign fasciculation syndrome, Cramp fasciculation syndrome) |
Upper limbs/calf muscle[66] | Muscle hypertrophy[66] | ||
| Strongman syndrome
(Muscle hypertrophy syndrome, myalgic) |
General | Childhood-onset | Muscle hypertrophy[67][68] | |
| Hypertrophia musculorum vera
(Latin for true muscle hypertrophy) |
Calf muscle/masseter muscle[69][70] | Variable. Typically adult-onset (early 20s) | Calf muscle hypertrophy, there may also be hypertrophy of masseter muscles (used for chewing food). Muscle biopsy of affected muscles shows hypertrophy of muscle fibres with occasional central migration of sarcolemmal nuclei. EMG of affected muscles is myopathic.[69][70] | |
| Habitual toe walking secondary to autism spectrum disorder | Calf muscle[34] | Childhood-onset | Muscle hypertrophy |
Skin and other non-muscle tissue
| Disease grouping | Disease | Body part(s) typically affected | Age of onset | Biopsy, ultrasonography, CT scan or MRI |
|---|---|---|---|---|
| Lipomatosis | Madelung disease | Upper trunk | Adult-onset | Subcutaneous adipose tissue |
| Parasitic | Disseminated cysticercosis | Skin/General | Variable | Pork tapeworm cysts |
| Inflammation of the joint | Amyloidosis | shoulders "shoulder pad sign"[71] | Adult-onset | Amyloid deposits, significant thickening of the subdeltoid bursa[71] |
See also
References
- ↑ "pseudoathletic", Wiktionary, 2016-06-02, retrieved 2023-06-12
- ↑ Cheng, Chun-Yu (2023-01-11). "Pseudo-athletic appearance from excess alcohol use". BMJ. 380: e072885. doi:10.1136/bmj-2022-072885. ISSN 1756-1833. S2CID 255570540.
- ↑ "Myotonia Congenita - Symptoms, Causes, Treatment | NORD". rarediseases.org. Retrieved 2023-06-12.
- 1 2 3 4 5 Kornegay, Joe N.; Childers, Martin K.; Bogan, Daniel J.; Bogan, Janet R.; Nghiem, Peter; Wang, Jiahui; Fan, Zheng; Howard, James F.; Schatzberg, Scott J.; Dow, Jennifer L.; Grange, Robert W.; Styner, Martin A.; Hoffman, Eric P.; Wagner, Kathryn R. (February 2012). "The Paradox of Muscle Hypertrophy in Muscular Dystrophy". Physical Medicine and Rehabilitation Clinics of North America. 23 (1): 149–xii. doi:10.1016/j.pmr.2011.11.014. ISSN 1047-9651. PMC 5951392. PMID 22239881.
- 1 2 3 Walters, Jon (October 2017). "Muscle hypertrophy and pseudohypertrophy". Practical Neurology. 17 (5): 369–379. doi:10.1136/practneurol-2017-001695. ISSN 1474-7766. PMID 28778933.
- 1 2 Nadaj-Pakleza, Aleksandra (2022-07-01). "Muscle hypertrophy: indicative of good health or disease? / Hypertrophie musculaire: signe de bonne santé ou de maladie ?". Les Cahiers de Myologie (in French and English) (25): 10–15. doi:10.1051/myolog/202225004. ISSN 2108-2219.
- 1 2 3 Ji, Hongzhao; Weatherall, Paul; Adams-Huet, Beverley; Garg, Abhimanyu (August 2013). "Increased skeletal muscle volume in women with familial partial lipodystrophy, Dunnigan variety". The Journal of Clinical Endocrinology and Metabolism. 98 (8): E1410–1413. doi:10.1210/jc.2013-1297. ISSN 1945-7197. PMC 3733861. PMID 23783098.
- 1 2 3 El-Darouti, Mohammad Ali; Al-Ali, Faiza Mohamed (2019), El-Darouti, Mohammad Ali; Al-Ali, Faiza Mohamed (eds.), "Loss of Subcutaneous Fat, Muscle Hypertrophy, Diabetes and Hyperlipidemia", Challenging Cases in Dermatology Volume 2: Advanced Diagnoses and Management Tactics, Cham: Springer International Publishing, pp. 7–11, doi:10.1007/978-3-030-21855-3_2, ISBN 978-3-030-21855-3, S2CID 202826748, retrieved 2023-10-12
- ↑ "BECKWITH-WIEDEMANN SYNDROME; BWS". www.omim.org. Retrieved 2023-09-01.
- 1 2 3 4 5 6 "Large Muscles". neuromuscular.wustl.edu. Retrieved 2023-07-03.
- 1 2 Kumar, Sunil; Jain, Shraddha; Kashikar, Shivali (December 2012). "Herculean appearance due to disseminated cysticercosis: case report". Asian Pacific Journal of Tropical Medicine. 5 (12): 1007–1008. doi:10.1016/S1995-7645(12)60192-8. ISSN 2352-4146. PMID 23199724.
- 1 2 3 4 5 6 7 Mangaraj, Swayamsidha; Sethy, Ganeswar (2014). "Hoffman's syndrome – A rare facet of hypothyroid myopathy". Journal of Neurosciences in Rural Practice. 5 (4): 447–448. doi:10.4103/0976-3147.140025. ISSN 0976-3147. PMC 4173264. PMID 25288869.
- 1 2 3 4 5 Reimers, C. D.; Schlotter, B.; Eicke, B. M.; Witt, T. N. (November 1996). "Calf enlargement in neuromuscular diseases: a quantitative ultrasound study in 350 patients and review of the literature". Journal of the Neurological Sciences. 143 (1–2): 46–56. doi:10.1016/s0022-510x(96)00037-8. ISSN 0022-510X. PMID 8981297. S2CID 25971689.
- 1 2 Lawson, Thomas M.; Bevan, Martin A.; Williams, Bryan D. (August 2002). "Clinical images: Skeletal muscle pseudo-hypertrophy in myeloma-associated amyloidosis". Arthritis and Rheumatism. 46 (8): 2251. doi:10.1002/art.10422. ISSN 0004-3591. PMID 12209535.
- ↑ Pignolo, Robert J.; Shore, Eileen M.; Kaplan, Frederick S. (2011-12-01). "Fibrodysplasia ossificans progressiva: clinical and genetic aspects". Orphanet Journal of Rare Diseases. 6: 80. doi:10.1186/1750-1172-6-80. ISSN 1750-1172. PMC 3253727. PMID 22133093.
- 1 2 de Visser, Marianne (2020-12-01). "Late-onset myopathies: clinical features and diagnosis". Acta Myologica. 39 (4): 235–244. doi:10.36185/2532-1900-027. ISSN 1128-2460. PMC 7783434. PMID 33458579.
- 1 2 Chu, Mary Lynn; Moran, Ellen (October 2018). "The Limb–Girdle Muscular Dystrophies: Is Treatment on the Horizon?". Neurotherapeutics. 15 (4): 849–862. doi:10.1007/s13311-018-0648-x. ISSN 1933-7213. PMC 6277288. PMID 30019308.
- 1 2 3 Bisceglia, Luigi; Zoccolella, Stefano; Torraco, Alessandra; Piemontese, Maria Rosaria; Dell'Aglio, Rosa; Amati, Angela; De Bonis, Patrizia; Artuso, Lucia; Copetti, Massimiliano; Santorelli, Filippo Maria; Serlenga, Luigi; Zelante, Leopoldo; Bertini, Enrico; Petruzzella, Vittoria (June 2010). "A new locus on 3p23–p25 for an autosomal-dominant limb-girdle muscular dystrophy, LGMD1H". European Journal of Human Genetics. 18 (6): 636–641. doi:10.1038/ejhg.2009.235. ISSN 1018-4813. PMC 2987336. PMID 20068593.
- 1 2 Straub, Volker; Murphy, Alexander; Udd, Bjarne; LGMD workshop study group (August 2018). "229th ENMC international workshop: Limb girdle muscular dystrophies - Nomenclature and reformed classification Naarden, the Netherlands, 17-19 March 2017". Neuromuscular Disorders. 28 (8): 702–710. doi:10.1016/j.nmd.2018.05.007. hdl:10138/305127. ISSN 1873-2364. PMID 30055862. S2CID 51865029.
- ↑ "Phenotypic Series - PS236670 - OMIM". omim.org. Retrieved 2023-09-30.
- ↑ "Phenotypic Series - PS613155 - OMIM". www.omim.org. Retrieved 2023-07-03.
- ↑ "Phenotypic Series - PS609308 - OMIM". omim.org. Retrieved 2023-09-30.
- ↑ "#300696 - MYOPATHY, X-LINKED, WITH POSTURAL MUSCLE ATROPHY; XMPMA". omim.org. Retrieved 2023-07-03.
- ↑ "#613319 - MIYOSHI MUSCULAR DYSTROPHY 3; MMD3". omim.org. Retrieved 2023-07-03.
- ↑ Di Blasi, Claudia; Sansanelli, Serena; Ruggieri, Alessandra; Moriggi, Manuela; Vasso, Michele; D'Adamo, Adamo Pio; Blasevich, Flavia; Zanotti, Simona; Paolini, Cecilia; Protasi, Feliciano; Tezzon, Frediano; Gelfi, Cecilia; Morandi, Lucia; Pessia, Mauro; Mora, Marina (September 2015). "A CASQ1 founder mutation in three Italian families with protein aggregate myopathy and hyperCKaemia". Journal of Medical Genetics. 52 (9): 617–626. doi:10.1136/jmedgenet-2014-102882. ISSN 1468-6244. PMID 26136523. S2CID 24276340.
- ↑ "#616231 - MYOPATHY, VACUOLAR, WITH CASQ1 AGGREGATES; VMCQA". omim.org. Retrieved 2023-07-03.
- ↑ "#619040 - MYOFIBRILLAR MYOPATHY 10; MFM10". omim.org. Retrieved 2023-07-03.
- 1 2 3 Stunnenberg, Bas C.; LoRusso, Samantha; Arnold, W. David; Barohn, Richard J.; Cannon, Stephen C.; Fontaine, Bertrand; Griggs, Robert C.; Hanna, Michael G.; Matthews, Emma; Meola, Giovanni; Sansone, Valeria A.; Trivedi, Jaya R.; van Engelen, Baziel G.M.; Vicart, Savine; Statland, Jeffrey M. (October 2020). "Guidelines on clinical presentation and management of nondystrophic myotonias". Muscle & Nerve. 62 (4): 430–444. doi:10.1002/mus.26887. ISSN 0148-639X. PMC 8117169. PMID 32270509.
- 1 2 Trivedi, Jaya R.; Bundy, Brian; Statland, Jeffrey; Salajegheh, Mohammad; Rayan, Dipa Raja; Venance, Shannon L.; Wang, Yunxia; Fialho, Doreen; Matthews, Emma; Cleland, James; Gorham, Nina; Herbelin, Laura; Cannon, Stephen; Amato, Anthony; Griggs, Robert C. (July 2013). "Non-dystrophic myotonia: prospective study of objective and patient reported outcomes". Brain. 136 (7): 2189–2200. doi:10.1093/brain/awt133. ISSN 0006-8950. PMC 3692030. PMID 23771340.
- 1 2 3 Molenaar, Joery P.; Verhoeven, Jamie I.; Rodenburg, Richard J.; Kamsteeg, Erik J.; Erasmus, Corrie E.; Vicart, Savine; Behin, Anthony; Bassez, Guillaume; Magot, Armelle; Péréon, Yann; Brandom, Barbara W.; Guglielmi, Valeria; Vattemi, Gaetano; Chevessier, Frédéric; Mathieu, Jean (2020-02-01). "Clinical, morphological and genetic characterization of Brody disease: an international study of 40 patients". Brain: A Journal of Neurology. 143 (2): 452–466. doi:10.1093/brain/awz410. ISSN 1460-2156. PMC 7009512. PMID 32040565.
- ↑ "600332 - RIPPLING MUSCLE DISEASE 1; RMD1". omim.org. Retrieved 2023-07-03.
- ↑ "#606072 - RIPPLING MUSCLE DISEASE 2; RMD2". omim.org. Retrieved 2023-07-03.
- 1 2 Wildermuth, Susanne; Spranger, Stephanie; Spranger, Matthias; Raue, Friedhelm; Meinck, Hans-Michael (July 1996). "Köbberling-Dunnigan syndrome: A rare cause of generalized muscular hypertrophy". Muscle & Nerve. 19 (7): 843–847. doi:10.1002/(SICI)1097-4598(199607)19:7<843::AID-MUS5>3.0.CO;2-9. ISSN 0148-639X. PMID 8965837. S2CID 46022844 – via Wiley Online Library.
- 1 2 3 4 5 6 Hassan, Ijas; Bhanudeep, Singanamalla; Madaan, Priyanka; Chhajed, Monika; Saini, Lokesh (2021). "Bilateral Calf Hypertrophy and Isolated Motor Delay: Think Beyond Muscular Dystrophy". Journal of Pediatric Neurosciences. 16 (2): 173–174. doi:10.4103/jpn.JPN_171_20. ISSN 1817-1745. PMC 8706592. PMID 35018192.
- ↑ "Stiff-Person Syndrome - Neurologic Disorders". Merck Manuals Professional Edition. Retrieved 2023-07-03.
- ↑ Newsome, Scott D.; Johnson, Tory (2022-08-15). "Stiff person syndrome spectrum disorders; more than meets the eye". Journal of Neuroimmunology. 369: 577915. doi:10.1016/j.jneuroim.2022.577915. ISSN 1872-8421. PMC 9274902. PMID 35717735.
- 1 2 3 4 Hynes, John P.; Glynn, David; Eustace, Stephen J. (2022-03-22). "Denervation pseudo hypertrophy of the calf: An important cause of lower limb swelling". Radiology Case Reports. 17 (5): 1702–1704. doi:10.1016/j.radcr.2022.02.066. ISSN 1930-0433. PMC 8956883. PMID 35345565.
- 1 2 Shields, Lisa B.E.; Iyer, Vasudeva; Bhupalam, Rukmaiah C.; Zhang, Yi Ping; Shields, Christopher B. (2021-10-19). "Hypertrophy of the tensor fascia lata: A pseudotumor due to lumbar radiculopathy". Surgical Neurology International. 12: 522. doi:10.25259/SNI_857_2021. ISSN 2229-5097. PMC 8571211. PMID 34754572.
- ↑ Rajvanshi, Satyam; Philip, Rajeev; Rai, Gopal K.; Gupta, K. K. (May 2012). "Kocher-Debre-Semelaigne syndrome". Thyroid Research and Practice. 9 (2): 53. doi:10.4103/0973-0354.96047. ISSN 0973-0354.
- 1 2 Sinclair, Christopher; Gilchrist, James M.; Hennessey, James V.; Kandula, Manju (September 2005). "Muscle carnitine in hypo- and hyperthyroidism". Muscle & Nerve. 32 (3): 357–359. doi:10.1002/mus.20336. ISSN 0148-639X. PMID 15803480. S2CID 41839983.
- 1 2 Rodolico, Carmelo; Bonanno, Carmen; Pugliese, Alessia; Nicocia, Giulia; Benvenga, Salvatore; Toscano, Antonio (2020-09-01). "Endocrine myopathies: clinical and histopathological features of the major forms". Acta Myologica. 39 (3): 130–135. doi:10.36185/2532-1900-017. ISSN 1128-2460. PMC 7711326. PMID 33305169.
- 1 2 Qureshi, Waseem; Hassan, Ghulam; Khan, Ghulam Qadir; Kadri, Syed Manzoor; Kak, Manish; Ahmad, Manzoor; Tak, Shahid; Kundal, Darshan Lal; Hussain, Showkat; Rather, Abdul Rashid; Masoodi, Ibrahim; Sikander, Sabia (2005-07-20). "Hoffmann's syndrome: a case report". GMS German Medical Science. 3: Doc05. ISSN 1612-3174. PMC 2703243. PMID 19675722.
- 1 2 3 Wong, Kin Hoi; Chow, Maria Bernadette Che Ying; Lui, Tun Hing; Cheong, Yue Kew; Tam, Kwok Fai (2017-07-25). "Denervation pseudohypertrophy of calf muscles associated with diabetic neuropathy". Radiology Case Reports. 12 (4): 815–820. doi:10.1016/j.radcr.2017.06.011. ISSN 1930-0433. PMC 5823303. PMID 29484078.
- 1 2 Menon, M. Suraj; Roopch, P. Sreedharan; Kabeer, K. Abdulkhayar; Shaji, C. Velayudhan (July 2016). "Calf Muscle Hypertrophy in Late Onset Pompe's Disease". Archives of Medicine and Health Sciences. 4 (2): 251. doi:10.4103/2321-4848.196188. ISSN 2321-4848. S2CID 58424073.
- 1 2 Marbini, A.; Gemignani, F.; Saccardi, F.; Rimoldi, M. (October 1989). "Debrancher deficiency neuromuscular disorder with pseudohypertrophy in two brothers". Journal of Neurology. 236 (7): 418–420. doi:10.1007/BF00314902. ISSN 0340-5354. PMID 2809644. S2CID 21158814.
- ↑ Hokezu, Y.; Nagamatsu, K.; Nakagawa, M.; Osame, M.; Ohnishi, A. (June 1983). "[Glycogenosis type III with peripheral nerve disorder and muscular hypertrophy in an adult]". Rinsho Shinkeigaku = Clinical Neurology. 23 (6): 473–479. ISSN 0009-918X. PMID 6317246.
- 1 2 Kishnani, Priya S.; Austin, Stephanie L.; Arn, Pamela; Bali, Deeksha S.; Boney, Anne; Case, Laura E.; Chung, Wendy K.; Desai, Dev M.; El-Gharbawy, Areeg; Haller, Ronald; Smit, G. Peter A.; Smith, Alastair D.; Hobson-Webb, Lisa D.; Wechsler, Stephanie Burns; Weinstein, David A. (July 2010). "Glycogen Storage Disease Type III diagnosis and management guidelines". Genetics in Medicine. 12 (7): 446–463. doi:10.1097/GIM.0b013e3181e655b6. ISSN 1530-0366. PMID 20631546. S2CID 4609175.
- 1 2 Rodríguez-Gómez, I.; Santalla, A.; Díez-Bermejo, J.; Munguía-Izquierdo, D.; Alegre, L. M.; Nogales-Gadea, G.; Arenas, J.; Martín, M. A.; Lucía, A.; Ara, I. (November 2018). "Non-osteogenic muscle hypertrophy in children with McArdle disease". Journal of Inherited Metabolic Disease. 41 (6): 1037–1042. doi:10.1007/s10545-018-0170-7. hdl:10578/19657. ISSN 1573-2665. PMID 29594644. S2CID 4394513.
- 1 2 Pietrusz, Aleksandra; Scalco, Renata S.; Quinlivan, Ros (2018). "Resistance Exercise Training in McArdle Disease: Myth or Reality?". Case Reports in Neurological Medicine. 2018: 9658251. doi:10.1155/2018/9658251. ISSN 2090-6668. PMC 6186374. PMID 30363996Patient 1 had hypertrophy of calf, deltoid and bicep muscles before resistance training commenced, while living a sedentary lifestyle with an office job, walking short distances was difficult as was everyday tasks like vacuuming and cutting the grass. After four years of resistance training, pre-existing hypertrophy in deltoid muscles increased further and muscle bulk was gained in additional muscle groups (quadriceps, gluteus, pectoralis, and trapezius muscles).
{{cite journal}}: CS1 maint: postscript (link) - ↑ Rasheed, Khalid; Sethi, Pooja; Bixby, Eric (May 2013). "Severe vitamin d deficiency induced myopathy associated with rhabydomyolysis". North American Journal of Medical Sciences. 5 (5): 334–336. doi:10.4103/1947-2714.112491. ISSN 2250-1541. PMC 3690793. PMID 23814767.
- 1 2 Polly, Patsie; Tan, Timothy C. (2014-04-16). "The role of vitamin D in skeletal and cardiac muscle function". Frontiers in Physiology. 5: 145. doi:10.3389/fphys.2014.00145. ISSN 1664-042X. PMC 3995052. PMID 24782788.
- 1 2 Yoshikawa, S.; Nakamura, T.; Tanabe, H.; Imamura, T. (June 1979). "Osteomalacic myopathy". Endocrinologia Japonica. 26 (Suppl): 65–72. doi:10.1507/endocrj1954.26.supplement_65. ISSN 0013-7219. PMID 467350.
- 1 2 "#618823 - CONGENITAL MYOPATHY 9B, PROXIMAL, WITH MINICORE LESIONS; CMYP9B". omim.org. Retrieved 2023-07-03.
- 1 2 3 4 Morin, Gilles; Biancalana, Valérie; Echaniz‐Laguna, Andoni; Noury, Jean‐Baptiste; Lornage, Xavière; Moggio, Maurizio; Ripolone, Michela; Violano, Raffaella; Marcorelles, Pascale; Maréchal, Denis; Renaud, Florence; Maurage, Claude‐Alain; Tard, Céline; Cuisset, Jean‐Marie; Laporte, Jocelyn (January 2020). "Tubular aggregate myopathy and Stormorken syndrome: Mutation spectrum and genotype/phenotype correlation". Human Mutation. 41 (1): 17–37. doi:10.1002/humu.23899. ISSN 1059-7794. PMID 31448844. S2CID 201753610.
- ↑ Cameron, C. H. Stuart; Allen, Ingrid V.; Patterson, Victor; Avaria, Maria A. (December 1992). "Dominantly inherited tubular aggregate myopathy". The Journal of Pathology. 168 (4): 397–403. doi:10.1002/path.1711680410. ISSN 0022-3417. PMID 1484321. S2CID 3241237.
- ↑ Lupi, Amalia; Spolaor, Simone; Favero, Alessandro; Bello, Luca; Stramare, Roberto; Pegoraro, Elena; Nobile, Marco Salvatore (2023-05-08). "Muscle magnetic resonance characterization of STIM1 tubular aggregate myopathy using unsupervised learning". PLOS ONE. 18 (5): e0285422. Bibcode:2023PLoSO..1885422L. doi:10.1371/journal.pone.0285422. ISSN 1932-6203. PMC 10166478. PMID 37155641.
- 1 2 3 4 Tajsharghi, Homa; Oldfors, Anders (January 2013). "Myosinopathies: pathology and mechanisms". Acta Neuropathologica. 125 (1): 3–18. doi:10.1007/s00401-012-1024-2. ISSN 1432-0533. PMC 3535372. PMID 22918376.
- 1 2 "MYOPATHY, DISTAL, 1; MPD1". www.omim.org. Retrieved 2023-09-23.
- 1 2 "CONGENITAL MYOPATHY 7A, MYOSIN STORAGE, AUTOSOMAL DOMINANT; CMYP7A". www.omim.org. Retrieved 2023-09-23.
- ↑ "#255800 - SCHWARTZ-JAMPEL SYNDROME, TYPE 1; SJS1". omim.org. Retrieved 2023-07-03.
- ↑ "#300280 - URUGUAY FACIOCARDIOMUSCULOSKELETAL SYNDROME; FCMSU". www.omim.org. Retrieved 2023-07-03.
- ↑ "#600092 - NIVELON-NIVELON-MABILLE SYNDROME; NNMS". omim.org. Retrieved 2023-07-03.
- ↑ "SATOYOSHI SYNDROME". www.omim.org. Retrieved 2023-09-01.
- ↑ "154850 - MASTICATORY MUSCLES, HYPERTROPHY OF". www.omim.org. Retrieved 2023-07-03.
- ↑ "606773 - HEMIFACIAL MYOHYPERPLASIA; HMH". www.omim.org. Retrieved 2023-07-03.
- 1 2 3 4 Kathait, Aparna; Dhar, Siddharth; Garg, Divyani; Chatterjee, Atri; Chandan, Shishir K. (2022). "Syringomyelia: An Unusual Cause of Pronounced Calf Hypertrophy". Annals of Indian Academy of Neurology. 25 (6): 1182–1183. doi:10.4103/aian.aian_486_22. ISSN 0972-2327. PMC 9996497. PMID 36911462.
- ↑ Conte, Talita C.; et al. "A Missense Mutation in DCST2 Causes the Strongman Syndrome". The Canadian Institutes of Health Research - Institute of Genetics (CIHR-IG).
- ↑ Brais, B.; Conte, T.; Dicaire, M.; Tetreault, M.; O'Ferrall, E.; Ravenscroft, G.; Laing, N.; Lamont, P.; Taivasssalo, T.; Hepple, R.; Mathieu, J. (October 2016). "A missense mutation in the putative sarcoplasmic reticulum transmembrane protein DCST2 causes dominant strongman syndrome". Neuromuscular Disorders. 26: S95. doi:10.1016/j.nmd.2016.06.038. ISSN 0960-8966. S2CID 54367645.
- 1 2 "HYPERTROPHIA MUSCULORUM VERA". omim.org. Retrieved 2023-09-23.
- 1 2 Poch, G. F.; Sica, E. P.; Taratuto, A.; Weinstein, I. H. (January 1971). "Hypertrophia musculorum vera. Study of a family". Journal of the Neurological Sciences. 12 (1): 53–61. doi:10.1016/0022-510x(71)90251-6. ISSN 0022-510X. PMID 5100002.
- 1 2 Uzunoğlu, Ceren; Toptaş, Tayfur; İpek, Yıldız; Arıkan, Fatma; Yılmaz, Fergün; Tuğlular, Tülin (September 2021). "Shoulder-Pad Sign in a Case of Amyloidosis Associated with Myeloma". Turkish Journal of Hematology. 38 (3): 233–234. doi:10.4274/tjh.galenos.2021.2021.0630. ISSN 1300-7777. PMC 8386310. PMID 34014054.
Further reading
Neuromuscular disease centre, Washington University - Large or prominent muscles
National Center for Biotechnology Information (NCBI) - Skeletal muscle hypertrophy, generalized muscle hypertrophy, calf muscle hypertrophy, thigh hypertrophy
The Human Phenotype Ontology (HPO) project - Skeletal muscle hypertrophy, calf muscle hypertrophy, muscle hypertrophy of the lower extremities, upper limb muscle hypertrophy