Shigella
| Shigella | |
|---|---|
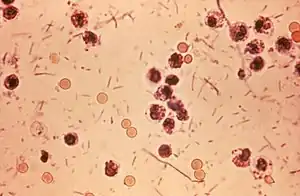 | |
| Photomicrograph of Shigella sp. in a stool specimen | |
| Scientific classification | |
| Domain: | Bacteria |
| Phylum: | Pseudomonadota |
| Class: | Gammaproteobacteria |
| Order: | Enterobacterales |
| Family: | Enterobacteriaceae |
| Genus: | Shigella Castellani & Chalmers 1919 |
| Species | |
Shigella is a genus of bacteria that is Gram-negative, facultative anaerobic, non-spore-forming, nonmotile, rod-shaped, and genetically closely related to E. coli. The genus is named after Kiyoshi Shiga, who first discovered it in 1897.[1]
The causative agent of human shigellosis, Shigella causes disease in primates, but not in other mammals.[2] It is only naturally found in humans and gorillas.[3][4] During infection, it typically causes dysentery.[5]
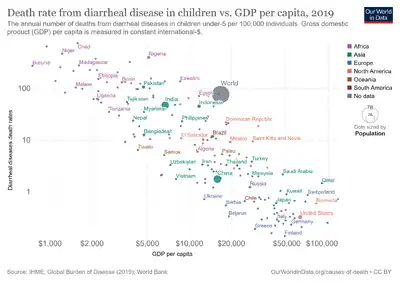
Shigella is one of the leading bacterial causes of diarrhea worldwide, causing an estimated 80–165 million cases.[6] The number of deaths it causes each year is estimated at between 74,000 and 600,000.[6][7] It is one of the top four pathogens that cause moderate-to-severe diarrhea in African and South Asian children.[8]
Classification
Shigella species are classified by three serogroups and one serotype:
- Serogroup A: S. dysenteriae (15 serotypes)[9]
- Serogroup B: S. flexneri (9 serotypes)[10]
- Serogroup C: S. boydii (19 serotypes)[11]
- Serogroup D: S. sonnei (one serotype)
Groups A–C are physiologically similar; S. sonnei (group D) can be differentiated on the basis of biochemical metabolism assays.[12] Three Shigella groups are the major disease-causing species: S. flexneri is the most frequently isolated species worldwide, and accounts for 60% of cases in the developing world; S. sonnei causes 77% of cases in the developed world, compared to only 15% of cases in the developing world; and S. dysenteriae is usually the cause of epidemics of dysentery, particularly in confined populations such as refugee camps.[13]
Each of the Shigella genomes includes a virulence plasmid that encodes conserved primary virulence determinants. The Shigella chromosomes share most of their genes with those of E. coli K12 strain MG1655.[14] Phylogenetic studies indicate Shigella is more appropriately treated as subgenus of Escherichia, and that certain strains generally considered E. coli—such as E. coli O157:H7—are better placed in Shigella (see Escherichia coli#Diversity for details).
Pathogenesis
Shigella infection is typically by ingestion. Depending on the health of the host, fewer than 100 bacterial cells can be enough to cause an infection.[15] Shigella species generally invade the epithelial lining of the colon, causing severe inflammation and death of the cells lining the colon. This inflammation results in the diarrhea and even dysentery that are the hallmarks of Shigella infection.[12] Some strains of Shigella produce toxins which contribute to disease during infection. S. flexneri strains produce ShET1 and ShET2, which may contribute to diarrhea.[12] S. dysenteriae strains produce Shiga toxin, which is hemolytic similar to the verotoxin produced by enterohemorrhagic E. coli. Both Shiga toxin and verotoxin are associated with hemolytic-uremic syndrome.[12]
Shigella species invade the host through the M-cells interspersed in the gut epithelia of the small intestine, as they do not interact with the apical surface of epithelial cells, preferring the basolateral side.[16] Shigella uses a type-III secretion system, which acts as a biological syringe to translocate toxic effector proteins to the target human cell. The effector proteins can alter the metabolism of the target cell, for instance leading to the lysis of vacuolar membranes or reorganization of actin polymerization to facilitate intracellular motility of Shigella bacteria inside the host cell. For instance, the IcsA effector (which is an autotransporter instead of type III secretion system effector) protein triggers actin reorganization by N-WASP recruitment of Arp2/3 complexes, helping cell-to-cell spread.[17]
After infection, Shigella cells multiply intracellularly and spread to neighboring epithelial cells, resulting in tissue destruction and characteristic pathology of shigellosis.[18][19] The most common symptoms are diarrhea, fever, nausea, vomiting, stomach cramps, and flatulence. It is also commonly known to cause large and painful bowel movements. The stool may contain blood, mucus, or pus. Hence, Shigella cells may cause dysentery. In rare cases, young children may have seizures. Symptoms can take as long as a week to appear, but most often begin two to four days after ingestion. Symptoms usually last for several days, but can last for weeks. Shigella is implicated as one of the pathogenic causes of reactive arthritis worldwide.[20]
History
The Shigella genus is named after Japanese physician Kiyoshi Shiga, who researched the cause of dysentery. Shiga entered the Tokyo Imperial University School of Medicine in 1892, during which he attended a lecture by Shibasaburo Kitasato. Shiga was impressed by Kitasato's intellect and confidence, so after graduating, he went to work for him as a research assistant at the Institute for Infectious Diseases. In 1897, Shiga focused his efforts on what the Japanese referred to as a sekiri (dysentery) outbreak. These epidemics were detrimental to the Japanese people and occurred often in the late 19th century. The 1897 sekiri epidemic affected >91,000, with a mortality rate of >20%.[21]
Shiga studied 32 dysentery patients and used Koch's postulates to successfully isolate and identify the bacterium causing the disease. He continued to study and characterize the bacterium, identifying its methods of toxin production i.e Shiga toxin, and worked tirelessly to create a vaccine for the disease.
See also
References
- ↑ Yabuuchi, Eiko (2002). "Bacillus dysentericus (sic) 1897 was the first taxonomic rather than Bacillus dysenteriae 1898". International Journal of Systematic and Evolutionary Microbiology. 52 (Pt 3): 1041. doi:10.1099/00207713-52-3-1041. PMID 12054222.
- ↑ Ryan, Kenneth James; Ray, C. George, eds. (2004). Sherris medical microbiology: an introduction to infectious diseases (4th ed.). McGraw-Hill Professional Med/Tech. ISBN 978-0-8385-8529-0.
- ↑ Pond, Kathy (2005). "Shigella". Water recreation and disease. Plausibility of associated infections: Acute effects, sequelae and mortality. WHO. pp. 113–8. ISBN 978-92-4-156305-5. Archived from the original on June 30, 2013.
- ↑ "Shigellosis" (PDF). European Association of Zoo and Wildlife Veterinarians. Archived from the original (PDF) on 2015-09-27.
- ↑ Mims, Cedric; Dockrell, Hazel; Goering, Richard; Roitt, Ivan; Wakelin, Derek; Zuckerman, Mark, eds. (2004). Medical Microbiology (3rd ed.). Mosby. p. 287. ISBN 978-0-7234-3259-3.
- 1 2 Bowen A (2016). "Chapter 3: Infectious Diseases Related to Travel". The Yellow Book: Health Information for International Travel. CDC. ISBN 978-0-19-937915-6. Archived from the original on 11 June 2016. Retrieved 22 June 2016.
- ↑ Mani, Sachin; Wierzba, Thomas; Walker, Richard I (2016). "Status of vaccine research and development for Shigella". Vaccine. 34 (26): 2887–2894. doi:10.1016/j.vaccine.2016.02.075. PMID 26979135.
- ↑ Kotloff, Karen L; Nataro, James P; Blackwelder, William C; et al. (2013). "Burden and aetiology of diarrhoeal disease in infants and young children in developing countries (the Global Enteric Multicenter Study, GEMS): a prospective, case-control study". The Lancet. 382 (9888): 209–222. doi:10.1016/S0140-6736(13)60844-2. PMID 23680352. S2CID 205969172. Archived from the original on 2021-04-23. Retrieved 2023-03-23.
- ↑ Ansaruzzaman, M; Kibriya, AK; Rahman, A; Neogi, PK; Faruque, AS; Rowe, B; Albert, MJ (1995). "Detection of provisional serovars of Shigella dysenteriae and designation as S. dysenteriae serotypes 14 and 15". Journal of Clinical Microbiology. 33 (5): 1423–5. doi:10.1128/JCM.33.5.1423-1425.1995. PMC 228185. PMID 7615772.
- ↑ Knirel, Y. A.; Sun, Q; Senchenkova, SN; Perepelov, AV; Shashkov, AS; Xu, J (2015). "O-Antigen Modifications Providing Antigenic Diversity of Shigella flexneri and Underlying Genetic Mechanisms". Biochemistry (Moscow). 80 (7): 901–914. doi:10.1134/S0006297915070093. PMID 26542003. S2CID 7360433.
- ↑ Yang, Z; Hu, C; Chen, J; Chen, G; Liu, Z (1990). "A new serotype of Shigella boydii". Wei Sheng Wu Xue Bao (in 中文). 30 (4): 284–95. PMID 2251827.
- 1 2 3 4 Hale, Thomas L.; Keusch, Gerald T. (1996). "Shigella". In Baron, Samuel (ed.). Medical microbiology (4th ed.). Galveston, Texas: University of Texas Medical Branch. ISBN 978-0-9631172-1-2. PMID 21413292. Archived from the original on 2019-12-15. Retrieved 2023-03-23.
- ↑ "Shigellosis" (PDF). State of the art of new vaccine research and development. Immunization, Vaccines and Biologicals. World Health Organization. 2006. pp. 10–2. Archived (PDF) from the original on 2015-09-27.
- ↑ Yang, Fan; Yang, Jian; Zhang, Xiaobing; Chen, Lihong; Jiang, Yan; Yan, Yongliang; Tang, Xudong; Wang, Jing; Xiong, Zhaohui; Dong, Jie; Xue, Ying; Zhu, Yafang; Xu, Xingye; Sun, Lilian; Chen, Shuxia; Nie, Huan; Peng, Junping; Xu, Jianguo; Wang, Yu; Yuan, Zhenghong; Wen, Yumei; Yao, Zhijian; Shen, Yan; Qiang, Boqin; Hou, Yunde; Yu, Jun; Jin, Qi (2005). "Genome dynamics and diversity of Shigella species, the etiologic agents of bacillary dysentery". Nucleic Acids Research. 33 (19): 6445–58. doi:10.1093/nar/gki954. PMC 1278947. PMID 16275786.
- ↑ Levinson, Warren E (2006). Review of Medical Microbiology and Immunology (9th ed.). McGraw-Hill Medical Publishing Division. p. 30. ISBN 978-0-07-146031-6.
- ↑ Mounier, Joëlle; Vasselon, T; Hellio, R; Lesourd, M; Sansonetti, PJ (January 1992). "Shigella flexneri Enters Human Colonic Caco-2 Epithelial Cells through the Basolateral Pole". Infection and Immunity. 60 (1): 237–248. doi:10.1128/IAI.60.1.237-248.1992. PMC 257528. PMID 1729185.
- ↑ Snapper, Scott B.; Takeshima, Fuminao; Antón, Inés; Liu, Ching-Hui; Thomas, Sheila M.; Nguyen, Deanna; Dudley, Darryll; Fraser, Hunter; Purich, Daniel (October 2001). "N-WASP deficiency reveals distinct pathways for cell surface projections and microbial actin-based motility". Nature Cell Biology. 3 (10): 897–904. doi:10.1038/ncb1001-897. ISSN 1476-4679. PMID 11584271. S2CID 23962367.
- ↑ Todar, Kenneth. "Shigella and Shigellosis". Todar's Online Textbook of Bacteriology. Archived from the original on 2022-08-20. Retrieved 2023-03-23.
- ↑ Suzuki, Toshihiko; Sasakawa, Chihiro (2001). "Molecular basis of the intracellular spreading of Shigella". Infection and Immunity. 69 (10): 5959–66. doi:10.1128/IAI.69.10.5959-5966.2001. PMC 98722. PMID 11553531.
- ↑ Hill Gaston, J (2003). "Arthritis associated with enteric infection". Best Practice & Research Clinical Rheumatology. 17 (2): 219–39. doi:10.1016/S1521-6942(02)00104-3. PMID 12787523.
- ↑ Trofa, Andrew F.; Ueno-Olsen, Hannah; Oiwa, Ruiko; Yoshikawa, Masanosuke (1999-11-01). "Dr. Kiyoshi Shiga: Discoverer of the Dysentery Bacillus". Clinical Infectious Diseases. 29 (5): 1303–1306. doi:10.1086/313437. ISSN 1058-4838. PMID 10524979.
External links
- Shigella Archived 2022-09-13 at the Wayback Machine genomes and related information at PATRIC Archived 2011-07-27 at the Wayback Machine, a Bioinformatics Resource Center funded by NIAID Archived 2021-08-26 at the Wayback Machine
- Vaccine Resource Library: Shigellosis and enterotoxigenic Escherichia coli (ETEC) Archived 2012-05-05 at the Wayback Machine
- US Centers for Disease Control and Prevention. Shigella - Shigellosis Archived 2016-02-08 at the Wayback Machine