This article was co-authored by Anthony Stark, EMR. Anthony Stark is a certified EMR (Emergency Medical Responder) in British Columbia, Canada. With over 11 years of experience, he has worked as an industrial medic and provided urban and rural paramedic services. He currently works for Mountain View Safety Services and previously worked for the British Columbia Ambulance Service. Anthony has a Bachelor of Engineering in Electrical, Electronics, and Communications Engineering from the Georgia Institute of Technology. He has completed the EMP Canada EMT Course and Swiftwater Awareness Training associated with the British Columbia Ambulance Service.
There are 9 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 129,230 times.
The proper application of a pressure dressing after a serious injury could save your life or someone else's. This important first-aid technique treats rapid blood loss; it provides compression to injured blood vessels which encourages blood clotting. A pressure dressing also can be used to treat venomous snake bites. The pressure on the blood vessels prevents the venom or poison in the bite site from progressing into the bloodstream and potentially throughout your entire body. The pressure dressing works best at stabilizing wounds on limbs, arms and legs.
Steps
Treating a Bleeding Wound
-
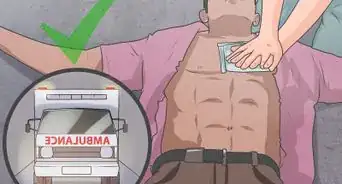
1Make treatment of the bleeding wound a priority. Time is of the essence when a deep wound is bleeding profusely. Call or send for help immediately, or come up with a plan to reach medical personnel if you are somewhere remote.[1]
- Stabilize the injured person as much as possible before you consider leaving him if it is just the two of you. Delegate duties if several people are present. Let someone call or go for help if there is another who can help with the pressure dressing.
- If the person is conscious, ask for his consent to treat the wound before you touch it.
-
2Expose the entire wound to see the full extent of the injury. Cut, tear, push, and/or lift any clothing away from the wound. If clothing is stuck to the wound, leave that portion in place and work around it. Do not try to wash the wound. Resist the impulse to remove any impaled objects from the wound.[2]
- If you have access to a sterile saline solution, you can add some of this to keep the wound moist and to lift away clothing gently.
- Help the wound to coagulate. Ripping off the portion of clothing stuck to the wound may disturb blood clots and cause more bleeding.[3]
- Do not remove objects because they may be having a tamponade or compression effect within the wound. Injured blood vessels, arteries, or veins can clot faster when any type of pressure is applied. Removing an object from the wound may lead to more rapid hemorrhage or blood loss.[4]
- If an impaled object is involved, take a triangular bandage and roll it into a cord. Wrap this cord around the object to keep it from moving. Try not to jostle the object as you do this. You can also use rolled up gauze on either side of the object as well. Tape the support dressing in place. In a pinch, use clothing or other materials that are as clean as you can find. It is important that the impaled object move as little as possible, so that it does not cause tissue/blood vessel damage or initiate new bleeding.
- Leave washing the wound to medical personnel. The gentlest cleansing could dislodge blood clots. Treat serious and deep wounds differently from everyday superficial wounds. Do not manipulate the wound more than necessary. It is okay to protect the wound from further contamination if the area around the victim is dirty or filled with chemicals.[5]
Advertisement -
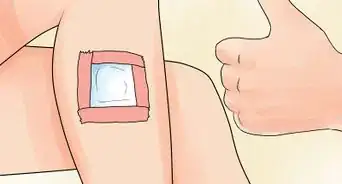
3Apply a regular dressing over the wound. Find the cleanest cloth available if you do not have a first-aid kit. Stabilize any impaled objects sticking out the wound with some of the bandage/cloth before you cover the wound. Secure the dressing in place.[6]
- If no impaled object is involved, make a dressing of sterile, nonstick gauze or the cleanest, most absorptive cloth available. Fold it into a dressing about 1 inch thick and apply it to wound.
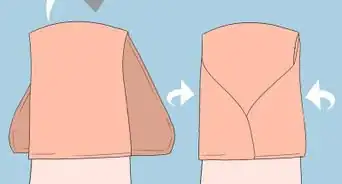
- Then, take a triangular bandage (or other length of cloth about 3 feet long). Fold it into a ribbon the width of your palm, then wrap it around the limb. Secure it with a firm but easily adjustable knot.
- Do not place the knot on the wound, but to the outside of the limb.
-
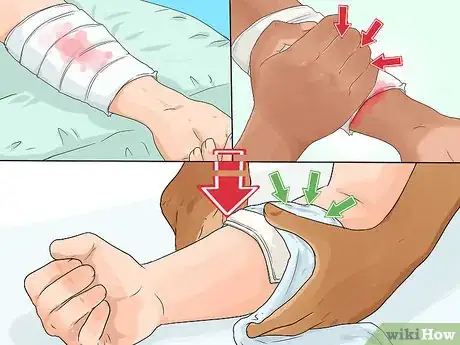
4Check the limb for signs of ischemia after securing the bandage. Make sure it has not turned blue or cool. This is a vital step if cloth has been tied around the limb. [7]
- Loosen the bandage slightly if you see signs of inadequate oxygen delivery to the limb or if you cannot find the pulse. Check the pulse below the bandage. Check on the inside of the wrist near the thumb or on top of the foot near the ankle.[8]
-
5Elevate the injured limb. The limb should be elevated above the level of the injured person’s heart. Do not elevate the limb before you splint any broken bones. [9]
- Elevate the leg by placing the foot or ankle on a pack, log, rock, or any other object; this works if the injured person is lying down or sitting. Elevate the arm by placing the forearm on the chest if the injured person is lying on her back or by placing the wrist on top of the head if she is sitting.[10]
- Splint a limb by finding straight objects (branches, foam, or cardboard) and wrapping material (clothing or climbing web). Use the wrapping material to first cover the objects that you will use as splints to avoid infection. Cut or rip sections so that you have at least three ties; use them to secure the objects on the limb to keep the fracture immobilized and to keep any injured joints straight. Do not compromise the blood flow to the limb by wrapping it too tightly.[11]
- Do not apply these bandage ties on top of the wound or the break. Apply them above and below the injury site. Remember to check the hand/foot beneath the splint for adequate blood flow.
-
6Apply manual pressure to the wound. Put direct pressure over the bandage with the hand. Maintain this for five to 10 minutes. Reassess for signs of uncontrolled hemorrhage like blood soaking the regular dressing or dripping from under the dressing.[12]
-
7Apply the pressure dressing only if manual pressure and elevation fail. If direct pressure fails to stem bleeding and the wound still bleeds through a second layer of bandage, then it is time to apply a pressure bandage. Pressure bandages prevent prolonged and excessive blood loss, which can cause a drop in blood volume (a decrease in the amount of blood flowing in your vessels), decreased blood pressure, loss of consciousness, and death.[13]
- Replace any blood volume losses and raise the victim’s blood pressure with liquids by mouth. Only do this if he is fully awake and the wound has been stabilized.[14]
-
8Make improvised bandages from strips of cloth. Use ripped or cut garments like T-shirts, pants, or socks. Place the pressure dressing on top of the regular dressing.
- Protect the wound and guard against making the bleeding worse. If you need to remove the pressure dressing for any reason, the regular dressing will be in place to prevent disturbing any clot which has formed in the wound.[15]
-
9Secure a wad of the improvised bandages over the wound. Take a longer piece of cloth and wrap it firmly around the wadded bandages. Tie the ends together. Apply enough pressure to help gain hemostasis, but do not create a tight tourniquet-like effect. One finger should be able to fit under the knot.[16]
- After you apply the securing bandage, check the fingers or toes past the bandage to ensure that they are still pink and warm. If not, loosen the bandages and try again.
-
10
-
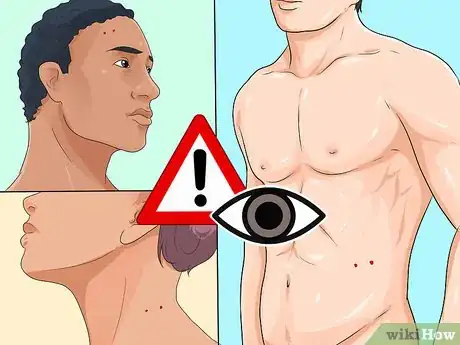
11Treat bleeding wounds on the torso and the head differently. Use the improvised bandages or bandages from a first-aid kit to apply manual pressure on the torso (chest and abdomen) and head in a very specific way. Use extreme caution when applying compression to these areas.[21] [22]
- Change your technique when applying a pressure dressing to the torso. The first steps are the same. Do not remove any objects from the wound. Apply the regular dressing. Tape this dressing, if you can. But, do not secure the dressing by wrapping cloth around the injured person. This could compromise the victim’s ability to breathe. Wad the cloth or bandages over the regular dressing on the wound. Apply enough manual pressure over the wad to stop the hemorrhage without interfering with the injured person’s breathing. Maintain this compression for 15 minutes. Continue the manual pressure if there are signs of continuing hemorrhage, such as a soaked dressing or blood dripping around the regular dressing.[23]
- You will have to continue this compression until medical personnel arrive or until the wound begins to clot.
- Do not apply any pressure to a head wound if the victim’s skull appears deformed. Look for sunken areas, visible bone fragments, or exposed brain tissue. Do not apply pressure to a wound which involves the eye or when an object in the wound clearly pierces the skull. Cover the wound gently with bandages, have the person lie down, and get him medical attention as soon as possible. Keep adding more bandages on top if the dressing gets soaked.[24]
- Assess the head wound and make sure pressure can be applied safely. Establish which dressing will be considered the regular dressing, even if it is not secured, and do not remove it.
- Apply manual pressure on wadded cloth or bandages over the regular dressing for 15 minutes. If the hemorrhage continues, reapply the manual pressure until medical personnel arrives.
- Wounds on the head bleed a lot because there are a lot of blood vessels close to the surface of the skin, so have plenty of extra dressings handy if you have them available.[25]
- Keep in mind that hair makes it hard to use tape and even long pieces of cloth wrapped around the head have a tendency to slip. Do not waste time trying to secure a regular dressing.
- Never wrap anything around the neck.
-
12Apply a tourniquet to a limb as a last resort. Use a tourniquet when no other technique (elevation, manual pressure, or a pressure dressing) has worked. A tourniquet compresses arteries and veins very firmly. There is very little blood flowing past the point of the tourniquet, thus preventing hemorrhage from the wound [26] [27]
- A tourniquet can be anything like a special device, a belt, or a long piece of cloth. It is used for limbs only. The best location to wrap the tourniquet is within 1-3" of the wound site, to minimize tissue death/damage. The tourniquet must be closer to the heart than the wound.[28] [29] Put something, a piece of cloth or the person’s clothing, under the tourniquet to protect the skin. Do not remove the tourniquet once it is placed.
- It does not take too much constant pressure to impede blood flow. However, a tourniquet is not a bandage like a pressure dressing. It is a very, very tight band around a limb. There is a definite risk of tissue loss and ischemia. Weigh the risk of loss of a limb versus the loss of life.[30]
Treating a Snake Bite
-
1Prioritize immobilizing the victim and applying a pressure dressing to the limb. The pressure immobilization technique is thought to hinder the movement of venom from the bite site into the circulation. Make plans to reach medical personnel while treating the bite wound.[31]
- Some research has shown that very little venom reaches the bloodstream if pressure is applied over the bite and the limb is immobilized, but this is still unproven.[32]
- Go to places known to have poisonous snakes with at least three people. One can call or go for help while another treats the bite wounds.
-
2Leave the victim’s clothing in place. Keep the person and the injured limb as still as possible. Do not promote movement of the venom into the bloodstream. [33]
-
3Allow the snake bite to bleed freely for 15 to 30 seconds. Let venom be evacuated from wound. Letting the wound bleed while keeping it still will help to keep the venom out of the circulatory system.
- During this expulsion phase, try to keep the limb lower than the heart to encourage the blood to expel the venom, rather than take it into the body.
-
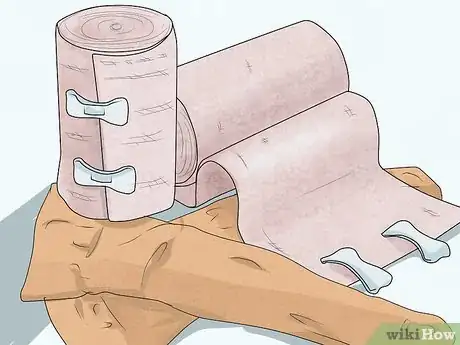
4Obtain a soft and flexible material for the pressure dressing. Use a flexible material like ace bandages or pantyhose, if available. Improvise and create a bandage by cutting or tearing something soft, like clothing or towels, into strips.[34]
-
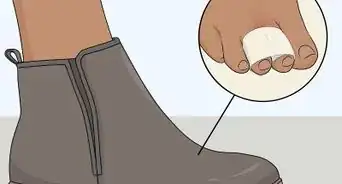
5Apply the pressure dressing upwards on the limb. Continue up the limb to cover the area of the bite, at minimum. Go up the limb as far as possible. Let only the amount of bandages limit you.[35]
- Start wrapping on the foot and cross the knee for bites anywhere on the leg. Start wrapping at the fingers and cross the elbow for bites anywhere on the arm. Bites located on the very upper arm and thigh will be challenging to cover; you may have treat them like they are on the torso.[36]
- This upward wrapping may squeeze a little venom towards the circulation. But it will be more comfortable and the injured person will tolerate it longer. The pressure dressing should be as tight as you would apply on a sprained ankle.[37]
-
6Immobilize the bitten limb with a splint. Take care to cross the joint to maximize the restriction of movement. Do not allow the victim to move the limb to help apply the splint.[38]
- Use any rigid object such as a branch, a tool with a handle, or rolled up newspaper. Wrap these objects with the same soft and flexible materials used to compress the limb before using them as splints.[39]
-
7Check for pulses in the bitten limb. Loosen the dressing if there are no pulses; the dressing is too tight. You want the pulse to be strong and normal.
- Check the pulse on top of the foot when the pressure dressing is on the leg. Check the pulse at the wrist near the thumb when the pressure dressing is on the arm.
-
8Keep the limb in a gravity-neutral position, if possible. Venom can travel into the circulation if the limb is kept above heart level. Swelling can occur if the limb hangs below heart level.
- Lie the victim flat on her back with her arms at the side. She should not be moving anyway.
-
9Treat snake bites to the torso, head, and neck differently. Wad cloth or bandages and apply manual pressure over a bite on the torso. Take care not to restrict breathing. Do not give any first aid if the bite is on the head or neck. Keep the patient still no matter the bite location and seek medical assistance immediately.[40]
-
10Initiate antivenin treatment as soon as possible. Do not remove the pressure dressing until right before the antivenin will be being given at a medical facility. Prompt treatment with antivenin will decrease the likelihood of morbidity (serious long-term side effects) and mortality (death) from the snake venom.
- Antivenin contains antibodies (the blood cells your body uses to destroy anything foreign) against specific poisons found in the venom of snakes. It is made from the blood of horses or sheep exposed to the specific venom.[41]
- Do not listen to old wives’ tales about how to treat a snake bite. Do not apply mouth suction. Do not cut into the bite site. Do not apply hot or cold packs. Do not apply a tourniquet. Do not delay treatment trying to kill and bring in the snake.[42]
- Treat the bite like it is from a venomous snake if you cannot identify the type of snake.[43]
-
11Provide supportive care to the victim. Help him deal with any symptoms as they arise. Encourage him to stay still. But, antivenin therapy is the definitive treatment which will combat the poison(s) in the snake venom and help the victim feel better.[44] [45]
- Expect general signs and symptoms such as swelling and redness around the bite, pain at the bite site, difficulty breathing, vomiting and nausea, blurred vision, sweating and salivating, numbness in the face and limbs, and decreased level of consciousness. Each snake venom has different side effects and you also could see convulsions, low blood pressure, and paralysis.[46]
References
- ↑ http://www.armystudyguide.com/content/powerpoint/First_Aid_Presentations/put-on-a-field-dressing-p-2.shtml
- ↑ http://www.armystudyguide.com/content/powerpoint/First_Aid_Presentations/put-on-a-field-dressing-p-2.shtml
- ↑ http://www.armystudyguide.com/content/powerpoint/First_Aid_Presentations/put-on-a-field-dressing-p-2.shtml
- ↑ http://www.armystudyguide.com/content/powerpoint/First_Aid_Presentations/put-on-a-field-dressing-p-2.shtml
- ↑ http://www.armystudyguide.com/content/powerpoint/First_Aid_Presentations/put-on-a-field-dressing-p-2.shtml
- ↑ http://www.armystudyguide.com/content/powerpoint/First_Aid_Presentations/put-on-a-field-dressing-p-2.shtml
- ↑ http://www.armystudyguide.com/content/Prep_For_Basic_Training/Prep_for_basic_first_aid/apply-a-pressure-dressing.shtml
- ↑ http://www.armystudyguide.com/content/powerpoint/First_Aid_Presentations/put-on-a-field-dressing-p-2.shtml
- ↑ http://www.armystudyguide.com/content/powerpoint/First_Aid_Presentations/put-on-a-field-dressing-p-2.shtml
- ↑ http://www.armystudyguide.com/content/powerpoint/First_Aid_Presentations/put-on-a-field-dressing-p-2.shtml
- ↑ http://www.emedicinehealth.com/wilderness_splinting/article_em.htm
- ↑ http://www.armystudyguide.com/content/powerpoint/First_Aid_Presentations/put-on-a-field-dressing-p-2.shtml
- ↑ http://www.armystudyguide.com/content/Prep_For_Basic_Training/Prep_for_basic_first_aid/apply-a-pressure-dressing.shtml
- ↑ http://www.armystudyguide.com/content/Prep_For_Basic_Training/Prep_for_basic_first_aid/apply-a-pressure-dressing.shtml
- ↑ http://www.armystudyguide.com/content/powerpoint/First_Aid_Presentations/put-on-a-field-dressing-p-2.shtml
- ↑ http://www.armystudyguide.com/content/Prep_For_Basic_Training/Prep_for_basic_first_aid/apply-a-pressure-dressing.shtml
- ↑ http://www.armystudyguide.com/content/Prep_For_Basic_Training/Prep_for_basic_first_aid/apply-a-pressure-dressing.shtml
- ↑ http://www.armystudyguide.com/content/powerpoint/First_Aid_Presentations/put-on-a-field-dressing-p-2.shtml
- ↑ http://www.armystudyguide.com/content/Prep_For_Basic_Training/Prep_for_basic_first_aid/apply-a-pressure-dressing.shtml
- ↑ http://www.armystudyguide.com/content/powerpoint/First_Aid_Presentations/put-on-a-field-dressing-p-2.shtml
- ↑ http://www.webmd.com/first-aid/tc/how-to-stop-bleeding-from-a-minor-head-wound-topic-overview
- ↑ http://www.armystudyguide.com/content/Prep_For_Basic_Training/Prep_for_basic_first_aid/apply-a-pressure-dressing.shtml
- ↑ http://www.armystudyguide.com/content/Prep_For_Basic_Training/Prep_for_basic_first_aid/apply-a-pressure-dressing.shtml
- ↑ http://www.webmd.com/first-aid/tc/how-to-stop-bleeding-from-a-minor-head-wound-topic-overview
- ↑ http://www.webmd.com/first-aid/tc/how-to-stop-bleeding-from-a-minor-head-wound-topic-overview
- ↑ http://medical-dictionary.thefreedictionary.com/tourniquet
- ↑ http://www.armystudyguide.com/content/Prep_For_Basic_Training/Prep_for_basic_first_aid/apply-a-pressure-dressing.shtml
- ↑ http://medical-dictionary.thefreedictionary.com/tourniquet
- ↑ http://www.armystudyguide.com/content/powerpoint/First_Aid_Presentations/put-on-a-field-dressing-p-2.shtml
- ↑ http://www.armystudyguide.com/content/powerpoint/First_Aid_Presentations/put-on-a-field-dressing-p-2.shtml
- ↑ https://www.health.qld.gov.au/poisonsinformationcentre/bites_stings/bs_pressure.asp
- ↑ https://www.health.qld.gov.au/poisonsinformationcentre/bites_stings/bs_pressure.asp
- ↑ https://www.health.qld.gov.au/poisonsinformationcentre/bites_stings/bs_pressure.asp
- ↑ https://www.health.qld.gov.au/poisonsinformationcentre/bites_stings/bs_pressure.asp
- ↑ https://www.health.qld.gov.au/poisonsinformationcentre/bites_stings/bs_pressure.asp
- ↑ https://www.health.qld.gov.au/poisonsinformationcentre/bites_stings/bs_pressure.asp
- ↑ https://www.health.qld.gov.au/poisonsinformationcentre/bites_stings/bs_pressure.asp
- ↑ https://www.health.qld.gov.au/poisonsinformationcentre/bites_stings/bs_pressure.asp
- ↑ https://www.health.qld.gov.au/poisonsinformationcentre/bites_stings/bs_pressure.asp
- ↑ https://www.health.qld.gov.au/poisonsinformationcentre/bites_stings/bs_pressure.asp
- ↑ http://www.medicinenet.com/script/main/art.asp?articlekey=40547
- ↑ http://www.healthline.com/health/snake-bites#Types&Symptoms2
- ↑ https://www.health.qld.gov.au/poisonsinformationcentre/bites_stings/bs_pressure.asp
- ↑ http://www.medicinenet.com/script/main/art.asp?articlekey=40547
- ↑ http://www.healthline.com/health/snake-bites#Types&Symptoms2
- ↑ http://www.healthline.com/health/snake-bites#Types&Symptoms2










































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...