This article was co-authored by Lisa Grossman, RN, BSN, PHN, IBCLC, CLC, CLEC and by wikiHow staff writer, Jessica Gibson. Lisa Grossman is a Lactation Consultant, Registered Nurse, and the Owner of South Bay Baby Care, a business focused on prenatal, breastfeeding, lactation, and CPR classes and services. Using years of experience working with mothers and babies, Lisa started South Bay Baby Care in 2018 with the goal of sharing her knowledge and expertise with expectant and new parents in the areas of newborn care, breastfeeding & lactation, sleep routines, postpartum care, and CPR + First Aid. Lisa holds a BSN from Mount St. Mary's University, is a board certified Registered Nurse (BRN RN-BSN), an International board certified Lactation Consultant (IBCLC), a Certified Lactation Counselor (ALPP), a Certified Lactation Educator Counselor (CLEC - UCSD), and a Member of the American Academy of Pediatrics (AAP).
There are 29 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 276,145 times.
Breastfeeding helps to guarantee that your baby gets a healthy start to life. Breast milk contains all the nutrients your baby needs, it's perfectly suited to their sensitive digestive systems, and it's crucial for the development of your infant's immune system since immunities pass from you to your baby through breastmilk.[1] Breastfed babies have a lower rate of infant mortality and experience better health throughout childhood. You may face obstacles to breastfeeding, so it's helpful to plan in advance. A little planning is well worth the benefits of breastfeeding your baby.[2]
Steps
Preparing to Breastfeed
-
1Learn to breastfeed before your baby arrives. While you and your baby will learn a lot about breastfeeding together, it's helpful to learn as much as you can in advance. Talk to other people in your family who may have breastfed and the wider community to get support. If you don't know many other people who have breastfed, don't let that stop you. There are many resources-both online and locally-that can help you.[3]
- Groups such as the La Leche League offer in-person meetings across the globe as well as social media groups to connect new and expectant mothers: https://www.llli.org
- Seek out a breastfeeding class either before or after your baby is born. You can find classes online or ask your medical provider or hospital for more information.
- Talk to the men in your life about breastfeeding, so they understand the health benefits, know what to expect, and can learn how to support you.
-
2Set up a nursing area. Create a space in your home where you can quietly and comfortably breastfeed your baby. Consider whether you'd prefer to nurse in a large chair, recliner, or sofa. If you can, set up the breastfeeding space near your baby's crib or bassinet, so you can feed and return the baby to the crib or bassinet, especially in the middle of the night. Stock your breastfeeding station with: [4]
- Breast pads and lanolin-based nipple cream
- Changes of clothes for the baby and a clean shirt for you
- Blankets and pillows
- Burp cloths
- Unscented baby wipes
- Healthy drinks such as water and unsweetened fruit juice.
- Nutritious snacks that can be held with one hand like a protein bar or fruit.
Advertisement -
3Talk to your employer about your rights as a breastfeeding mother. If you work away from your home and choose to pump breast milk, you will want to make arrangements to pump milk while at work. US Federal Law mandates that all employers provide both a time and space for breastfeeding mothers to pump milk while at work.
- Many other countries have similar laws. Research your rights before approaching your employer.
- Try to discuss the issue as far in advance as possible, so your employer will have time to make the necessary accommodations.
-
4Get comfortable clothes for nursing. Since you'll be breastfeeding often in the first weeks and months of your baby's life, you'll need to wear clothes that allow you to comfortably access your breasts. Purchase nursing bras, tanks, or comfortable button-down shirts. Keep in mind that skin to skin contact can encourage your baby to breastfeed.[5]
- You can also look for wrap-around dresses or cross-over tops.
- It's also possible to tailor regular bras to create nursing bras. The retailer, Nordstrom, offers this service for a small fee to mothers who buy a bra at their location.
-
5Prepare to overcome common obstacles to breastfeeding. A lack of community understanding and support poses one of the biggest challenges to breastfeeding. If you foresee resistance from those around you, seek out a support group to help educate those around you about your choice.[6]
- Mom's Rising has multiple resources that can you help advocate for your right to breastfeed: https://www.momsrising.org
Guaranteeing Optimal Nutrition
-
1Eat a healthy diet. Your baby is relying on you for nutrition, and your body has to sustain another person, so it's important for you to eat a balanced diet. You'll need about 500 extra calories a day while your body is making milk. Eat a diet rich in whole grains, fruits, vegetables, protein, and healthy fats to maximize your intake of vitamins and minerals.[7]
- Remember to keep taking your prenatal vitamins as long as you're breastfeeding.
- Since breastfeeding will actually burn a lot of calories, avoid cutting calories or dieting to lose weight.
-
2Talk to your doctor about vitamin D supplementation. Breastfeeding provides infants with the best nutrition possible, but recent studies have shown that breastfeeding babies would benefit from vitamin D supplement. It's recommended that infants receive a daily intake of 400 IU of vitamin D. Talk to your doctor about administering vitamin D drops to your infant.
- Most vitamin D supplements can be purchased over the counter at grocery stores. Make sure you are selecting the appropriate dose and only give infants the liquid-based form.[8]
-
3Stay hydrated. Plan on drinking water at regular intervals throughout the day and don't wait until you feel thirsty. Since staying hydrated can be difficult when you're busy caring for the baby, keep drinks nearby and drink throughout the day. A good way to ensure that you drink enough is to connect your water drinking to a task-such as drinking half a glass every time you nurse or change a diaper.[9]
- Drink primarily water, milk, decaffeinated teas, or juices-preferably juices with no added sugar.
- While you can have a little caffeine every day (about 300 mg or 1 to 2 cups of coffee, or 2 to 4 ounces of espresso), you should limit your intake while breastfeeding because caffeine can be passed to your baby through your breast milk.[10] If you notice that your baby is irritated after you drink caffeine and breastfeed, try having your coffee after breastfeeding and then waiting 4 hours to breastfeed again.[11]
-
4Avoid consuming alcohol 2 hours before you breastfeed. While you can have a drink or 2 a week while you're breastfeeding, you should plan on having the drink 2 to 3 hours before you breastfeed.
- A single (25 mL) shot of spirits (25 mL), an 8-ounce glass of beer, or a small (125 mL) glass of wine each count as one drink.[12]
- If you know you'll be drinking and your baby will need to breastfeed, consider pumping in advance.
- You should also avoid smoking for your and your baby's health. Smoking can lower nutrients in breastmilk, and it can change the way your breast milk tastes, causing your baby to refuse it.[13]
-
5Check with your doctor about medications. If you take medication, ask your doctor if it's safe to take while you're breastfeeding since some medications can be transferred through breast milk. In some cases, your doctor may be able to recommend different medications that are safe to take while breastfeeding.[14]
- Remember to ask your doctor about herbal supplements too. Many of these aren't regulated or tested, and some can actually reduce milk supply.
Positioning a Good Latch with a Cradle Hold
-
1Bring the baby into a cradle position. Your baby should be laying on their side and your forearm should support the baby. Rest the baby's head on the crook of that arm while your other arm wraps around and supports the baby's bottom.[15]
- The baby's ear, shoulder, and hip should form a straight line if you're in the correct cradle position.
-
2Support the baby. Once you're holding the baby in a basic cradle position, bring them close to you so the baby is on their side and your bellies are touching. Place a pillow behind the baby's back to bring the baby up towards you and prevent you from hunching over them. You should be sitting up and comfortable.[16]
- Consider placing a pillow underneath your arms or behind your back to provide extra support to you.
- Cradling your baby close to you should also prevent you from needing to hunch over towards the baby.
-
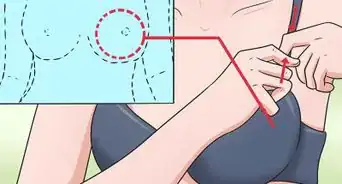
3Hold your breast and support the baby's head. Move your hand that had been supporting the baby's bottom to the breast you're going to feed from. Hold the breast with your thumb and fingers near the areola. Use your other hand to support and tilt your baby's head back a little.[17]
-
4Brush the baby's mouth with your nipple. Gently brush or tickle the baby's lips with your nipple. This will encourage the baby to open their mouth wide so you can begin breastfeeding.[18]
-
5Aim and insert the nipple towards the top of the baby's mouth. As soon as the baby opens their mouth wide, point your nipple towards the top of their mouth and bring the baby towards it. Your baby should have a mouthful of your areola. If your baby is latched on correctly, you should feel a gentle pulling, not pinching.[19]
- If the baby doesn't have enough of the areola in their mouth, your nipples may feel sore or painful. Remove the baby from your breast by inserting a finger into their mouth. Latch the baby on again so they can take more of your breast in their mouth.
Breastfeeding a Newborn
-
1Breastfeed as soon as you can. Try to breastfeed your baby as soon after the delivery as possible. Although your milk won't come in for several days, your body will produce a small amount of nutritious milk called colostrum.[20] Let your newborn breastfeed as long as they want to on one breast before you encourage the baby to breastfeed from the other breast.[21]
- Try to alternate which breast you begin feeding from when you start a new breastfeeding session. This will establish a good milk supply and prevent engorgement in the early weeks of breastfeeding.
-
2Breastfeed your newborn on demand. Watch for your baby's early hunger cues. Feed the baby when you see that the baby is more alert or active, when they're mouthing, or when they search for your nipple. Try to breastfeed the baby before they begin crying, since crying is a late sign of hunger. You'll probably need to breastfeed 8 to 12 times for every 24 hours.[22] [23]
- You should hear rhythmic, regular sucking if your baby is breastfeeding well.
-
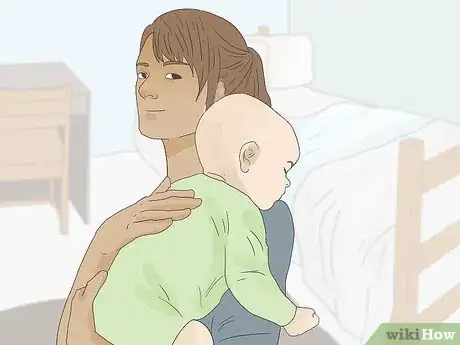
3Burp your baby. Consider burping your baby after breastfeeding to release any air your baby might have swallowed. If your baby is arching her back, squirming around, or looking uncomfortable, she might need to be burped. Try to burp your baby in one of these ways:[24]
- Lift your baby toward your shoulder, with your hand on their head and neck for support. The baby should be facing the area behind you. Rub your baby's back with a firm and open hand to release the trapped air.
- Sit your baby on your lap and lean it forward, supporting their chest with the base of your hand and their chin and neck with your fingers. Massage their stomach with your front hand and gently pat their back with your other hand.
- Lay your baby on your lap with their head raised higher than its stomach. Gently pat the baby's back until they burp.
-
4Pay attention to how often your newborn breastfeeds. A newborn baby will mostly alternate breastfeeding with sleeping. If your baby goes a long time without breastfeeding very much, you might need to wake them up every 2 or 3 hours to nurse. If your newborn baby is making 5 to 6 wet disposable diapers or 6 to 8 wet cloth diapers a day, they're getting enough breast milk.
- If you need to wake your baby to breastfeed, change their diaper first. This will wake the baby so they're alert and ready to breastfeed.
-
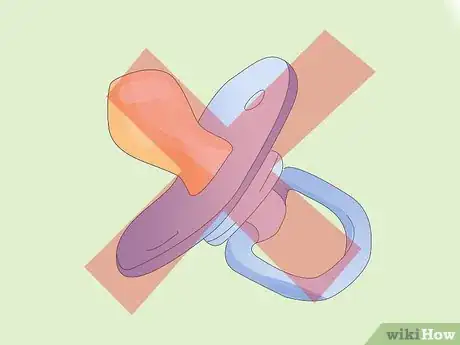
5Wait to give your baby a pacifier. If you want to offer your baby a pacifier, wait 1 month until breastfeeding is well established. This can prevent nipple confusion and give your baby a chance to develop sucking reflexes while they're breastfeeding.[25]
-
6Get help if you're struggling. If you're concerned about your milk supply, are struggling with the baby's latch, become engorged, or have any questions about breastfeeding, talk with a lactation consultant or your doctor. Many board-certified lactation consultants can be reached by phone at any time of day or night. Some even make house calls.
- You can also call the hospital or birth center where you delivered for help or lactation recommendations.
- For personal support, consider joining your local La Leche League chapter where you can meet and talk with other breastfeeding mothers.
Breastfeeding an Older Baby
-
1Breastfeed a baby that's teething. Your baby might want to breastfeed more because it comforts them. If you're worried that your baby will bite you, keep in mind that if your baby is actively nursing, they can't bite you. To prevent biting in a teething baby, take your baby off of the breast if they lose interest in nursing, begin to fall asleep, start to fidget, or tense their jaw.[26]
- Babies cut teeth at different ages, but generally you can expect your baby to begin teething around 6 months old.
-
2Handle fidgeting during breastfeeding. As your baby gets older, they'll become better at breastfeeding and will also become curious about their surroundings. Your baby may suddenly seem squirmy or wiggly while they're eating. To help your baby focus on breastfeeding, breastfeed in a quiet space that's free from distractions. Consider wearing a breastfeeding necklace that has large, textured beads for your baby to focus on while they nurse.[27]
- If your baby continues to wiggle to the point that you can't successfully breastfeed, stop the breastfeeding session. Try to breastfeed later once your baby is a little calmer.
-
3Follow your baby's lead. Your breastfeeding relationship with your baby is unique, so it's important to follow your baby's lead when it comes to nursing positions, breast preferences, and length of breastfeeding sessions.[28]
- For example, your baby might spend more time breastfeeding from the right breast than the left breast. This is fine as long as your baby is getting enough breast milk.
-
4Prepare for nursing strikes. Occasionally, older babies will refuse to breastfeed for a few days. This break, or nursing strike, can be caused by teething, illness, low milk supply, or separation anxiety. During a nursing strike, pump to maintain your milk supply, try to breastfeed frequently, try different breastfeeding positions, and breastfeed when your baby is drowsy and relaxed.[29]
- If your baby doesn't breastfeed for more than 2 days, contact the baby's doctor. The doctor can check for an underlying medical condition that might be making nursing uncomfortable.
-
5Breastfeed as long as you're comfortable. Don't feel pressured to breastfeed for a specific amount of time. Instead, breastfeed as long as you and your baby wish to continue. Your baby will begin eating soft, solid foods and will naturally cut back on the amount of breast milk they're getting from you.[30]
- The American Academy of Pediatrics recommends exclusive breastfeeding for the first six months after birth - and breastfeeding in combination with solid foods until at least age 1.[31] [32]
- The World Health Organization recommends exclusive breastfeeding for infants up to six months as well as breastfeeding for a minimum of 2 years along with solids.[33]
- Don't feel pressure to stop or start breastfeeding based on these guidelines. You and your baby-along with your healthcare provider-will decide how long to continue your breastfeeding relationship.
- Some babies prefer to keep breastfeeding, even just a little for several years. Others might prefer solids to breast milk and may only want to nurse for comfort.
Expert Q&A
Did you know you can get expert answers for this article?
Unlock expert answers by supporting wikiHow
-
QuestionWhat foods should I avoid when I'm breastfeeding?
 Sarah Siebold, IBCLC, MASarah Siebold is an International board certified Lactation Consultant (IBCLC) and Certified Lactation Educator Counselor (CLEC) based in Los Angeles, California. She runs her own lactation consulting practice called IMMA, where she specializes in emotional support, clinical care, and evidence-based breastfeeding practices. Her editorial work about new motherhood and breastfeeding has been featured in VoyageLA, The Tot, and Hello My Tribe. She completed her clinical lactation training in both private practice and outpatient settings through the University of California, San Diego. She also earned her M.A. in English and American Literature from New York University.
Sarah Siebold, IBCLC, MASarah Siebold is an International board certified Lactation Consultant (IBCLC) and Certified Lactation Educator Counselor (CLEC) based in Los Angeles, California. She runs her own lactation consulting practice called IMMA, where she specializes in emotional support, clinical care, and evidence-based breastfeeding practices. Her editorial work about new motherhood and breastfeeding has been featured in VoyageLA, The Tot, and Hello My Tribe. She completed her clinical lactation training in both private practice and outpatient settings through the University of California, San Diego. She also earned her M.A. in English and American Literature from New York University.
International Board Certified Lactation Consultant You don't need to avoid any foods! Old wives tales tell us that certain foods will make our babies gassy, but what we know scientifically is that that's just not true. A very small percentage of babies will have slight food intolerances based on the mother's diet, but more often than not, we really recommend moms eat everything in their diet. You should be eating a very nutrient-dense, rich array of foods. Spicy foods, cruciferous veggies, and other foods that were considered bad for lactation are really just myths.
You don't need to avoid any foods! Old wives tales tell us that certain foods will make our babies gassy, but what we know scientifically is that that's just not true. A very small percentage of babies will have slight food intolerances based on the mother's diet, but more often than not, we really recommend moms eat everything in their diet. You should be eating a very nutrient-dense, rich array of foods. Spicy foods, cruciferous veggies, and other foods that were considered bad for lactation are really just myths. -
QuestionWhen should I start breastfeeding a newborn?
 Mor Levy Volner, IBCLC, RDNMor Levy Volner is an International Board Certified Lactation Consultant based in Southern California. She earned a BS in Clinical Nutrition from the University of California, Davis in 2009 and finished her Lactation Consultant course from the University of California, San Diego Extension Program in 2013, which included 300 hours of lactation consulting experience from Kaiser Permanente. She also has an MS in Dietetics/Nutrition from the California State University - Northridge in 2014.
Mor Levy Volner, IBCLC, RDNMor Levy Volner is an International Board Certified Lactation Consultant based in Southern California. She earned a BS in Clinical Nutrition from the University of California, Davis in 2009 and finished her Lactation Consultant course from the University of California, San Diego Extension Program in 2013, which included 300 hours of lactation consulting experience from Kaiser Permanente. She also has an MS in Dietetics/Nutrition from the California State University - Northridge in 2014.
International Board Certified Lactation Consultant
-
QuestionHow do I bond with my baby while breastfeeding?
 Rebecca Nguyen, MARebecca Nguyen is a Certified Lactation Consultant and Childbirth Educator. She runs Family Picnic in Chicago, Illinois with her mother Sue Gottschall, where they teach new parents about childbirth, breastfeeding and child development and education. Rebecca taught preschool through 3rd grade for 10 years, and she received her Master’s Degree in Early Childhood Education from the University of Illinois in 2003.
Rebecca Nguyen, MARebecca Nguyen is a Certified Lactation Consultant and Childbirth Educator. She runs Family Picnic in Chicago, Illinois with her mother Sue Gottschall, where they teach new parents about childbirth, breastfeeding and child development and education. Rebecca taught preschool through 3rd grade for 10 years, and she received her Master’s Degree in Early Childhood Education from the University of Illinois in 2003.
International Board Certified Lactation Consultant Skin contact with your baby can help improve the breastfeeding experience. With a very new baby, we recommend as much skin-to-skin contact as possible, which means the baby's in a diaper and mom is topless from the waist up. Not only does it promote bonding, but it also improves breast milk production and ejection.
Skin contact with your baby can help improve the breastfeeding experience. With a very new baby, we recommend as much skin-to-skin contact as possible, which means the baby's in a diaper and mom is topless from the waist up. Not only does it promote bonding, but it also improves breast milk production and ejection.
Warnings
- Consult a lactation consultant, midwife or doctor if your baby is still fussy after nursing, isn't urinating or having regular bowel movements, isn't gaining weight, or has yellowish skin or nails.⧼thumbs_response⧽
- You should also contact medical providers if your breasts are sore, or your nipples are cracked and bleeding.⧼thumbs_response⧽
References
- ↑ https://www.cdc.gov/breastfeeding/faq/
- ↑ https://my.clevelandclinic.org/health/articles/15274-the-benefits-of-breastfeeding-for-baby--for-mom
- ↑ https://www.womenshealth.gov/breastfeeding/learning-breastfeed/preparing-breastfeed
- ↑ http://thebirthhour.com/breastfeeding-tips-setting-up-a-nursing-station/
- ↑ https://www.mom365.com/baby/breastfeeding/clothes-to-wear-for-breastfeeding/
- ↑ https://www.cdc.gov/breastfeeding/resources/us-breastfeeding-rates.html
- ↑ http://www.chop.edu/pages/diet-breastfeeding-mothers
- ↑ https://www.cdc.gov/breastfeeding/recommendations/index.htm
- ↑ https://www.ncbi.nlm.nih.gov/pubmed/1525748?dopt=AbstractPlus
- ↑ https://www.babycenter.com/0_caffeine-and-the-nursing-mom_4488.bc
- ↑ https://www.ncbi.nlm.nih.gov/pubmed/27129353
- ↑ http://www.nhs.uk/Conditions/pregnancy-and-baby/Pages/breastfeeding-alcohol.aspx
- ↑ https://www.ncbi.nlm.nih.gov/pubmed/392766
- ↑ https://kellymom.com/hot-topics/med-risks/
- ↑ https://www.fitpregnancy.com/baby/breastfeeding/how-breastfeed-step-by-step-guide
- ↑ https://www.fitpregnancy.com/baby/breastfeeding/how-breastfeed-step-by-step-guide
- ↑ https://www.fitpregnancy.com/baby/breastfeeding/how-breastfeed-step-by-step-guide
- ↑ http://www.marchofdimes.org/materials/how-to-breastfeed.pdf
- ↑ http://www.marchofdimes.org/materials/how-to-breastfeed.pdf
- ↑ https://www.babycenter.com/404_whats-colostrum_8896.bc
- ↑ http://www.babies.sutterhealth.org/breastfeeding/bf_frequency.html
- ↑ Lisa Grossman, RN, BSN, PHN, IBCLC, CLC, CLEC. International Board Certified Lactation Consultant. Expert Interview. 13 May 2020.
- ↑ http://www.babies.sutterhealth.org/breastfeeding/bf_frequency.html
- ↑ http://m.kidshealth.org/en/parents/burping.html
- ↑ https://www.breastfeedingbasics.com/articles/introducing-bottles-and-pacifiers-to-a-breastfed-baby
- ↑ https://www.breastfeedingbasics.com/articles/teething-and-biting
- ↑ https://kellymom.com/ages/older-infant/toddlernursing/#positioning
- ↑ https://www.essentialparent.com/lesson/how-long-should-each-feed-be-5957/
- ↑ http://www.motherandchildhealth.com/breastfeeding/surviving-a-nursing-breastfeeding-strike-my-baby-wont-nurse/
- ↑ Lisa Grossman, RN, BSN, PHN, IBCLC, CLC, CLEC. International Board Certified Lactation Consultant. Expert Interview. 13 May 2020.
- ↑ Lisa Grossman, RN, BSN, PHN, IBCLC, CLC, CLEC. International Board Certified Lactation Consultant. Expert Interview. 13 May 2020.
- ↑ https://www.mayoclinic.org/healthy-lifestyle/infant-and-toddler-health/in-depth/breast-feeding/art-20047898
- ↑ http://www.who.int/topics/breastfeeding/en/
- ↑ https://www.mayoclinic.org/healthy-lifestyle/infant-and-toddler-health/in-depth/breast-milk-storage/art-20046350?pg=2
- ↑ https://www.thebump.com/a/breastfeeding-laws
- ↑ https://www.thebump.com/a/breastfeeding-laws
About This Article
To breastfeed your baby, hold them in a cradle position with one arm supporting their head and the other under their bottom. You should also place a pillow behind your baby’s back to bring them up towards your body. Once you’re in position, hold your breast between the thumb and fingers of your hand that was supporting the baby’s bottom, and tilt their head back slightly with your other hand. Then, brush their mouth with your nipple, which will encourage them to open their mouth wide. As soon as they open their mouth, point your nipple towards the top of their mouth and bring your baby towards you. If they’re latched on correctly, you’ll feel a tugging sensation as they feed. For tips from our Medical co-author, including how often to breastfeed a newborn, read on!