This article was co-authored by Robert Dhir, MD. Dr. Robert Dhir is a board certified Urologist, Urological Surgeon, and the Founder of HTX Urology in Houston, Texas. With over 10 years of experience, Dr. Dhir’s expertise includes minimally-invasive treatments for enlarged prostate (UroLift), kidney stone disease, surgical management of urological cancers, and men’s health (erectile dysfunction, low testosterone, and infertility). His practice has been named a Center of Excellence for the UroLift procedure, and is a pioneer in non-surgical procedures for ED using his patented Wave Therapy. He earned his undergraduate and medical degrees from Georgetown University and was awarded honors in pre-medical studies, urology, orthopedics, and ophthalmology. Dr. Dhir served as chief resident during his urological surgical residency at University of Texas at Houston / MD Anderson Cancer Center in addition to completing his internship in general surgery. Dr. Dhir was voted Top Doctor in Urology for 2018 to 2019, one of the top three Best Rated Urologists in 2019 & 2020 for Houston Texas, and Texas Monthly has named him to the 2019 & 2020 Texas Super Doctors Rising Stars list.
There are 14 references cited in this article, which can be found at the bottom of the page.
wikiHow marks an article as reader-approved once it receives enough positive feedback. In this case, 84% of readers who voted found the article helpful, earning it our reader-approved status.
This article has been viewed 503,243 times.
If you just had contact with another person's genitals, you may be at risk for contracting a sexually transmitted infection (STI), also sometimes called a sexually transmitted disease (STD). Male and female condoms can help reduce the risk of STI transmission, but are not foolproof methods. STI symptoms are not always obvious, but there are some things to be on the lookout for.
Steps
Checking for Signs of Gonorrhea and Chlamydia
-
1Know that the symptoms of gonorrhea and chlamydia may not be obvious. You or your partner may have all, some, or none of these symptoms. Gonorrhea and chlamydia are bacterial infections. Symptoms gonorrhea typically arise within 10 days after exposure; symptoms of chlamydia typically arise one to three weeks after exposure.[1] Gonorrhea and chlamydia can both infect the genital tract, eyes, mouth, pharynx, and anus.[2]
-
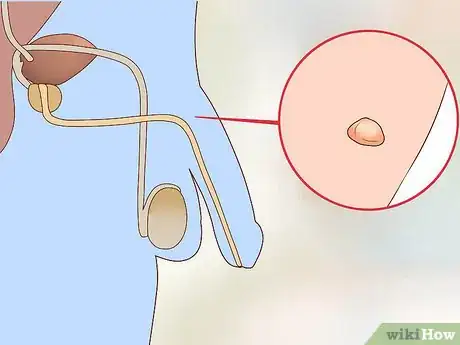
2Check your penis for signs of discharge. If you have chlamydia or gonorrhea, you may notice a lot of discharge coming from your urethra.[3] That discharge might be yellow, green, thick, bloody, or cloudy.[4] [5]
- Discharge from the penis is not a normal occurrence, but its presence does not necessarily mean you have an STI. The only way to find out for sure is to visit a healthcare provider and be tested.
-
3Notice if you have pain or a burning sensation while urinating. Infection of the urethra by gonorrhea bacteria can cause inflammation of the urethra.[6] This, in turn, can cause pain or a burning sensation.
-
4
-
5
-
6Have your partner check themselves for symptoms. If your partner has symptoms of gonorrhea or chlamydia (even if you do not show symptoms), you should both seek medical treatment. If your partner has a penis, follow the same checks as listed above. If your partner has a vagina, follow the guidance listed below:
- Check for increased vaginal discharge, or discharge that is not a typical color, odor, consistency, or appearance. This can be a symptom of gonorrhea or chlamydia infection. [11] [12]
- Check for pain or burning when urinating. This can be a sign of gonorrhea or chlamydia infection. [13] [14]
- Women can also get anal gonorrhea or anal chlamydia. The symptoms include itching of the anus, pain when having a bowel movement, anal soreness, anal bleeding, and anal discharge.[15] [16]
- Vaginal bleeding between periods can also be indicative of gonorrhea infection. [17]
-
7Seek medical care if you have any of the symptoms mentioned. Gonorrhea and chlamydia can cause permanent damage to your body if left untreated.
Checking for Signs of Syphilis
-
1Check your genitals, mouth, and anus for primary syphilis sores. (Have your partner check themselves as well.) The sores often appear as open, wet ulcers, or painless sores.[18] These sores, caused by infection with syphilis bacteria, typically appear between 10 days and three months after exposure.[19] They appear on the region of the body infected (such as the penis, vagina, tongue, lips, anus) and heal up, though the disease remains in the body. Secondary syphilis can reappear later on.[20]
-
2Evaluate yourself for signs of secondary syphilis. These symptoms begin three to six weeks after the disappearance of the primary syphilis sore and include: [21]
- Rash with ¾ inch red or brownish sores — This is the most classical sign of secondary syphilis. The rash is characterized as a rash (a flat, red area covered with bumps) over the trunk and extremities that includes the palms and soles of the hands and feet
- Fever
- Headache
- Sore throat
- Anorexia
- Muscle pain
- Weight loss
- Alopecia
- Gastrointestinal Findings
- Musculoskeletal Problems
- Neurological and Ocular Findings
- Swollen lymph nodes
- General feeling of malaise
-
3Be aware that syphilis may, at any point in the course of the infection, spread to the nervous system. This is dangerous and can cause neurological symptoms including uncoordinated movement and changes in behavior. In addition, secondary syphilis can lead to tertiary syphilis, which may spread to organs including and cause life-threatening complications.
- Neurosyphilis is difficult to diagnose and usually spinal fluid must be tested to confirm.
-
4Seek medical care if you have any of the symptoms listed above or suspect you may have syphilis. This is a dangerous disease that can cause permanent damage and even death if left untreated. Talk to your doctor immediately and get tested.
Checking for Signs of Genital Herpes
-
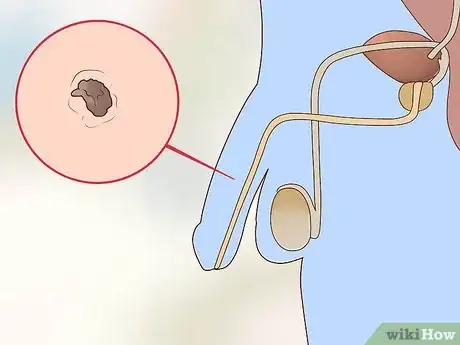
1Look for red, open sores; blisters; or small, red bumps in the genital or anal areas.[22] Sores can appear on the penis, scrotum, and even inside the urethra. Genital herpes is a viral infection caused by herpes simplex virus (HSV). This classically causes a painful sore on the penis or vagina.
- Though outbreaks of genital herpes can be managed with medication, once a person is infected, they will always carry the virus in their body.
-
2Note any pain or itching in the genital region, thighs, buttocks, or anus. Itching is typically the first symptoms of a herpes infection. Herpes sores are also painful, which can help you differentiate herpes from other conditions. [23]
-
3Be aware of discomfort when urinating. Herpes sores can occur inside the urethra, making urination painful.[24]
Checking for Signs of Human Papillomavirus (HPV) and Genital Warts
-
1Know that there are many types of HPV. The kinds that cause cancer are not the same kinds that cause genital warts.[25] There is also no way to test for the presence of HPV in men.
-
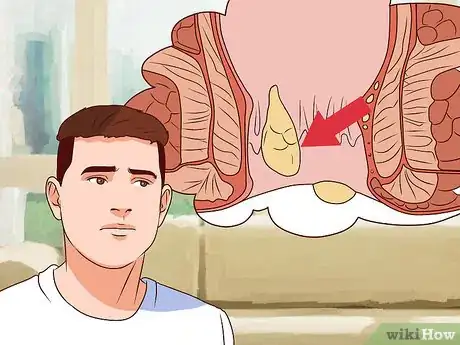
2Examine your penis for small flesh-colored or gray-colored wart-like lesions. Individual genital warts are often small — less than 1 millimeter in diameter; however, they may multiply and several can grow in close proximity to each other.[26] This can cause the warts to look like cauliflower.[27] The warts can be located in and around the genitals, anus, and in the mouth and the back of the throat.
-
3Note any bleeding after sexual intercourse.[28] This can be a sign of genital warts or another condition.
-
4Be aware of itching or pain in the genital region, on the buttocks, or in the mouth. These signs can point to genital warts or another STI.
-
5Understand that there are typically no symptoms from infection by the types of HPV that can cause cancer in men and in women. In men, these types of HPV can cause penile, anal, or oropharyngeal cancer.[29] In women, these types of HSV can cause cervical, anal, or oropharyngeal cancer.[30] There are vaccines that can prevent infection with some types of HPV that cause cancer or genital warts.[31]
- Men between the ages of nine and 26 are approved to receive HPV vaccines Gardasil and Gardasil.[32]
-
6Seek medical care if you have any of the symptoms listed above. Your healthcare provider can prescribe medications to treat genital warts, and can advise you about cancer risk if you have a cancer-causing type of HPV.
Following the Recommended Screening Guidelines
-
1Make sure that you and your partner are following the recommended screening guidelines for STIs. If your partner is a woman, there are certain tests she should get on a regular basis. If your partner is a man, he should be screened for certain STIs.[33] These tests can tell you if you or your partner have an STI, allowing you to take proper precautions and to seek treatment.
- Some STDs, including HIV, Hepatitis B, and Hepatitis C usually do not present with symptoms early on, so they must be detected on a blood test.[34]
- These guidelines are just that — a guide. You should discuss all testing and risk factors with your healthcare provider, and they will help you adjust screening accordingly.
- Make sure your partner is also tested and treated accordingly.
-
2Get tested for human immunodeficiency virus (HIV) at least once in your life between 13 – 64 years of age. Men who have sex with men should be tested at least yearly, if not more frequently.[35]
-
3Get tested for gonorrhea and chlamydia yearly if you are under 25 years old, or if you have new or multiple sex partners. [36] Having multiple sex partners puts you at an increased risk for STIs.
-
4
Expert Q&A
Did you know you can get expert answers for this article?
Unlock expert answers by supporting wikiHow
-
QuestionI have small rash under my penis I take medication but nothing changes. What should I do?
 Chris M. Matsko, MDDr. Chris M. Matsko is a retired physician based in Pittsburgh, Pennsylvania. With over 25 years of medical research experience, Dr. Matsko was awarded the Pittsburgh Cornell University Leadership Award for Excellence. He holds a BS in Nutritional Science from Cornell University and an MD from the Temple University School of Medicine in 2007. Dr. Matsko earned a Research Writing Certification from the American Medical Writers Association (AMWA) in 2016 and a Medical Writing & Editing Certification from the University of Chicago in 2017.
Chris M. Matsko, MDDr. Chris M. Matsko is a retired physician based in Pittsburgh, Pennsylvania. With over 25 years of medical research experience, Dr. Matsko was awarded the Pittsburgh Cornell University Leadership Award for Excellence. He holds a BS in Nutritional Science from Cornell University and an MD from the Temple University School of Medicine in 2007. Dr. Matsko earned a Research Writing Certification from the American Medical Writers Association (AMWA) in 2016 and a Medical Writing & Editing Certification from the University of Chicago in 2017.
Family Medicine Physician
-
QuestionI have a little stain or liquid on my underwear, but I don't have any warts, pain when I urinate, and I don't feel sick. What should I do?
 Chris M. Matsko, MDDr. Chris M. Matsko is a retired physician based in Pittsburgh, Pennsylvania. With over 25 years of medical research experience, Dr. Matsko was awarded the Pittsburgh Cornell University Leadership Award for Excellence. He holds a BS in Nutritional Science from Cornell University and an MD from the Temple University School of Medicine in 2007. Dr. Matsko earned a Research Writing Certification from the American Medical Writers Association (AMWA) in 2016 and a Medical Writing & Editing Certification from the University of Chicago in 2017.
Chris M. Matsko, MDDr. Chris M. Matsko is a retired physician based in Pittsburgh, Pennsylvania. With over 25 years of medical research experience, Dr. Matsko was awarded the Pittsburgh Cornell University Leadership Award for Excellence. He holds a BS in Nutritional Science from Cornell University and an MD from the Temple University School of Medicine in 2007. Dr. Matsko earned a Research Writing Certification from the American Medical Writers Association (AMWA) in 2016 and a Medical Writing & Editing Certification from the University of Chicago in 2017.
Family Medicine Physician
-
QuestionWhat are some common symptoms of STDs in males?
 Robert Dhir, MDDr. Robert Dhir is a board certified Urologist, Urological Surgeon, and the Founder of HTX Urology in Houston, Texas. With over 10 years of experience, Dr. Dhir’s expertise includes minimally-invasive treatments for enlarged prostate (UroLift), kidney stone disease, surgical management of urological cancers, and men’s health (erectile dysfunction, low testosterone, and infertility). His practice has been named a Center of Excellence for the UroLift procedure, and is a pioneer in non-surgical procedures for ED using his patented Wave Therapy. He earned his undergraduate and medical degrees from Georgetown University and was awarded honors in pre-medical studies, urology, orthopedics, and ophthalmology. Dr. Dhir served as chief resident during his urological surgical residency at University of Texas at Houston / MD Anderson Cancer Center in addition to completing his internship in general surgery. Dr. Dhir was voted Top Doctor in Urology for 2018 to 2019, one of the top three Best Rated Urologists in 2019 & 2020 for Houston Texas, and Texas Monthly has named him to the 2019 & 2020 Texas Super Doctors Rising Stars list.
Robert Dhir, MDDr. Robert Dhir is a board certified Urologist, Urological Surgeon, and the Founder of HTX Urology in Houston, Texas. With over 10 years of experience, Dr. Dhir’s expertise includes minimally-invasive treatments for enlarged prostate (UroLift), kidney stone disease, surgical management of urological cancers, and men’s health (erectile dysfunction, low testosterone, and infertility). His practice has been named a Center of Excellence for the UroLift procedure, and is a pioneer in non-surgical procedures for ED using his patented Wave Therapy. He earned his undergraduate and medical degrees from Georgetown University and was awarded honors in pre-medical studies, urology, orthopedics, and ophthalmology. Dr. Dhir served as chief resident during his urological surgical residency at University of Texas at Houston / MD Anderson Cancer Center in addition to completing his internship in general surgery. Dr. Dhir was voted Top Doctor in Urology for 2018 to 2019, one of the top three Best Rated Urologists in 2019 & 2020 for Houston Texas, and Texas Monthly has named him to the 2019 & 2020 Texas Super Doctors Rising Stars list.
Board Certified Urologist & Urological Surgeon For chlamydia and gonorrhea, copious urethral discharge is noted. HPV looks like small warts or cauliflower-looking lesions on the genitals; herpes (HSV) looks more like a target sign with a whitish inner pustule and tends to be quite itchy. HIV, Hepatitis B, and Hepatitis C usually do not present with symptoms early on and are detected via blood test.
For chlamydia and gonorrhea, copious urethral discharge is noted. HPV looks like small warts or cauliflower-looking lesions on the genitals; herpes (HSV) looks more like a target sign with a whitish inner pustule and tends to be quite itchy. HIV, Hepatitis B, and Hepatitis C usually do not present with symptoms early on and are detected via blood test.
Warnings
- Many STIs do not cause obvious symptoms. If you or your partner are worried that you might have an STI, see a medical professional for testing.⧼thumbs_response⧽
- There are a number of STIs, including Hepatitis (A, B, and C) and HIV, that do not usually cause symptoms in the genital region, so they have not been discussed here.⧼thumbs_response⧽
References
- ↑ http://www.mayoclinic.org/diseases-conditions/sexually-transmitted-diseases-stds/in-depth/std-symptoms/art-20047081
- ↑ http://www.mayoclinic.org/diseases-conditions/sexually-transmitted-diseases-stds/in-depth/std-symptoms/art-20047081
- ↑ Robert Dhir, MD. Board Certified Urologist & Urological Surgeon. Expert Interview. 12 October 2020.
- ↑ http://www.cdc.gov/std/gonorrhea/stdfact-gonorrhea.htm
- ↑ http://www.cdc.gov/std/Chlamydia/STDFact-Chlamydia.htm
- ↑ https://www.nlm.nih.gov/medlineplus/ency/article/000439.htm
- ↑ http://www.cdc.gov/std/gonorrhea/stdfact-gonorrhea.htm
- ↑ http://www.cdc.gov/std/Chlamydia/STDFact-Chlamydia.htm
- ↑ http://www.cdc.gov/std/gonorrhea/stdfact-gonorrhea.htm
- ↑ http://www.cdc.gov/std/Chlamydia/STDFact-Chlamydia.htm
- ↑ http://www.cdc.gov/std/gonorrhea/stdfact-gonorrhea.htm
- ↑ http://www.cdc.gov/std/Chlamydia/STDFact-Chlamydia.htm
- ↑ http://www.cdc.gov/std/gonorrhea/stdfact-gonorrhea.htm
- ↑ http://www.cdc.gov/std/Chlamydia/STDFact-Chlamydia.htm
- ↑ http://www.cdc.gov/std/gonorrhea/stdfact-gonorrhea.htm
- ↑ http://www.cdc.gov/std/Chlamydia/STDFact-Chlamydia.htm
- ↑ http://www.cdc.gov/std/gonorrhea/stdfact-gonorrhea.htm
- ↑ http://www.plannedparenthood.org/learn/stds-hiv-safer-sex/syphilis
- ↑ http://www.mayoclinic.org/diseases-conditions/sexually-transmitted-diseases-stds/in-depth/std-symptoms/art-20047081?pg=2
- ↑ http://www.cdc.gov/std/syphilis/STDFact-Syphilis.htm
- ↑ http://www.mayoclinic.org/diseases-conditions/sexually-transmitted-diseases-stds/in-depth/std-symptoms/art-20047081?pg=2
- ↑ http://www.mayoclinic.org/diseases-conditions/sexually-transmitted-diseases-stds/in-depth/std-symptoms/art-20047081?pg=2
- ↑ http://www.mayoclinic.org/diseases-conditions/sexually-transmitted-diseases-stds/in-depth/std-symptoms/art-20047081?pg=2
- ↑ http://www.mayoclinic.org/diseases-conditions/sexually-transmitted-diseases-stds/in-depth/std-symptoms/art-20047081?pg=2
- ↑ http://www.cdc.gov/STD/HPV/STDFact-HPV.htm
- ↑ http://www.mayoclinic.org/diseases-conditions/sexually-transmitted-diseases-stds/in-depth/std-symptoms/art-20047081?pg=2
- ↑ Robert Dhir, MD. Board Certified Urologist & Urological Surgeon. Expert Interview. 12 October 2020.
- ↑ http://www.publichealth.va.gov/infectiondontpassiton/womens-health-guide/stds/hpv.asp
- ↑ http://www.cdc.gov/std/hpv/stdfact-hpv-and-men.htm
- ↑ http://www.cdc.gov/std/hpv/stdfact-hpv-and-men.htm
- ↑ http://www.cdc.gov/std/hpv/stdfact-hpv-and-men.htm
- ↑ http://www.webmd.com/vaccines/adult-hpv-vaccine-guidelines#1
- ↑ http://www.cdc.gov/std/prevention/screeningreccs.htm
- ↑ Robert Dhir, MD. Board Certified Urologist & Urological Surgeon. Expert Interview. 12 October 2020.
- ↑ http://www.cdc.gov/std/prevention/screeningreccs.htm
- ↑ http://www.cdc.gov/std/prevention/screeningreccs.htm
- ↑ http://www.cdc.gov/std/prevention/screeningreccs.htm
- ↑ http://www.cdc.gov/std/prevention/screeningreccs.htm
About This Article
To check a penis for signs of an STI, look for odd-colored discharge or pain while urinating. You can also palpate your testicles to see if they are tender or swollen, as this may be a sign of chlamydia or gonorrhea. If you think you have an STI, talk to your previous sexual partners to see if they have experienced any unusual symptoms as well. Make a doctors appointment to get tested if you are still unsure. To understand the symptoms of syphilis and genital warts, read more from our reviewer.


















-Step-10.webp)





















-Step-10.webp)



































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...