This article was co-authored by Lyssandra Guerra. Lyssandra Guerra is a Certified Nutrition & Wellness Consultant and the Founder of Native Palms Nutrition based in Oakland, California. She has over five years of nutrition coaching experience and specializes in providing support to overcome digestive issues, food sensitivities, sugar cravings, and other related dilemmas. She received her holistic nutrition certification from the Bauman College: Holistic Nutrition and Culinary Arts in 2014.
There are 18 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 14,987 times.
If you have diabetes or another blood sugar disorder, you know how difficult it can be to control your blood sugar levels. The good news is it doesn't have to be that hard. If you keep an eye on your blood sugar levels through careful monitoring, your doctor can help you get on a plan that works for you and includes medications and a healthy diet. You can also make lifestyle changes to help maintain better control of your health.
Steps
Stabilizing Blood Sugar with Food
-
1Eat or drink sugary foods if you're at 70 mg/dl or below. If you feel dizzy, sweaty, shaky, or weak, check your blood sugar. If you’re at 70 mg/dl or lower, you may need to eat or drink something with a high sugar content to bring it up.[1] After eating something, wait 15 minutes, then check your blood sugar again. If you’re still below 100 mg/dl, consume something else sugary. Try either taking 3-4 glucose tablets or drinking or eating one of the following to bring your blood sugar back up when it’s low:
- 1⁄2 cup (120 mL) of apple juice or soda
- ½ a banana
- 1 apple
- 4-5 saltine crackers,
- 2 tablespoons (30 ml) of raisins
- 1 tablespoon (15 ml) of honey
- Candies (e.g. lifesavers, skittles, gummy bears, or starbursts)
-
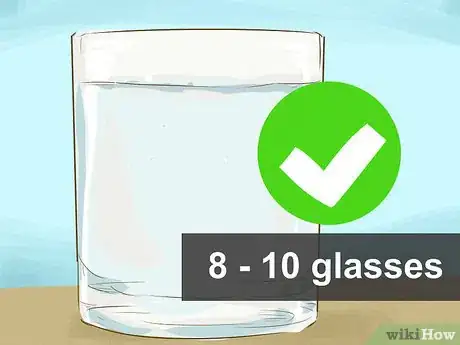
2Drink 10 to 15 cups (2.4 to 3.5 L) of water a day to stabilize blood sugar. When you're dehydrated, your blood doesn't have as much liquid to work with, which can throw your blood sugar off balance. Make sure you're getting 10 to 15 cups (2.4 to 3.5 L) of water each day to replenish what you lose.[2]Advertisement
-
3Talk to your doctor about your carbohydrate needs. Carbohydrates help keep your blood sugar levels high enough, and they provide your body with energy. However, too many carbs can significantly elevate your blood sugar and also cause weight gain, so try to keep careful track of how many carbohydrates you eat.[3]
- First, talk to your doctor or nutritionist about how many carbohydrates you need in a day. Then, use that information to portion out your carbohydrates throughout the day. In general, 15 grams (0.53 oz) of carbohydrates counts as one serving.
- Generally, men need 4 to 5 servings per meal, or 12-15 servings each day, while women need 3 to 4 servings per meal, or 9-12 servings each day.
- Remember that this increases or decreases depending on the amount of energy you’re exerting. Sitting in the office requires fewer servings, while climbing a mountain may require many more. Remember to adjust accordingly, as each day is different.
-
4Read food labels to determine the carbohydrate level. When counting carbohydrates, pay careful attention to labels. They will tell you how many carbs are in a certain food, so you don't have to guess. If the food doesn't have a label, look it up on the internet or in a nutrition app to find out.[4]
- For reference, one slice of bread is often a serving of carbohydrates, as is one small to medium piece of fruit, 0.5 cups (120 ml) of ice cream, and 1 cup (240 ml) of milk.
-
5Measure out food to determine servings. It's generally a good idea to measure out foods when you can. Most people underestimate how much they are eating, which often leads to weight gain. Measure out your food so that you stay aware of the true amount of carbs you’re consuming.
- If you aren’t sure how much food to measure out, consider scheduling a meeting with a dietician. They should be able to show you what portion sizes look like.
-
6Choose whole grains over refined grains to help control your blood sugar. Grains are one source of carbohydrates. Whole grains can help steady your blood sugars, so try to get at least half of your grains from whole grains. Choose whole-wheat bread and whole-wheat pasta, for instance, as well as foods like bulgur, oatmeal, and quinoa.[5]
-
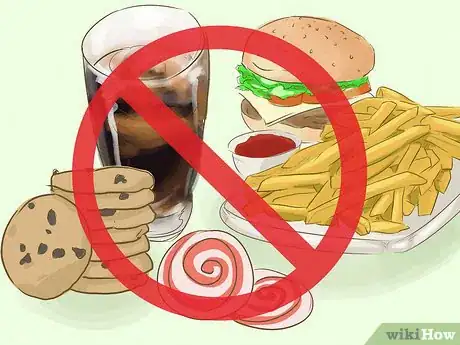
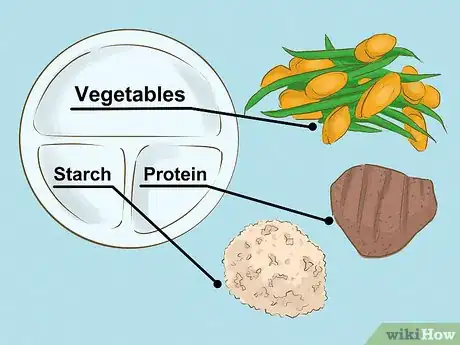
7Balance your meals with protein and vegetables. Eating balanced meals consistently can be significantly helpful in keeping your blood sugar levels steady.[6] When planning out your meals, choose a balance of protein, fruits, vegetables, starches, and fats.[7]
- Opt for lean proteins, such as chicken breast, fish, and beans. Try to limit your intake of fats, particularly trans fats, which are often found in processed foods. Focus mainly on good fats. Monounsaturated fats and polyunsaturated fats are good fats, and they are found in foods like nuts, sunflower oil, olive oil, fatty fish, flaxseeds, and canola oil. Avocados and peanut oil contain good fats as well, but they’re also calorie-heavy.[8]
- Carbohydrates quickly metabolize, meaning they are digested and absorbed quickly. Because of this, they’re able to give your body the quick energy it needs. Protein takes longer to metabolize, so it helps sustain energy. Fruits and vegetables give you fiber, which slows digestion, adds bulk to your diet, and helps stabilize your blood sugar.
Using Insulin to Control Your Blood Sugar
-
1Bring up oral medications with your doctor. The first choice of treatment for both type 1 and type 2 diabetes is an oral medication, though severe type 1 diabetics sometimes take insulin in addition to their oral medication. These medications work in different ways, but all help to lower your blood sugar levels overall.[9]
- One type of medication helps your body produce more insulin.
- Another type keep your stomach from breaking down sugars, meaning not as much enters your bloodstream.
- Other types stop your liver from releasing as much glucose to your blood, lowering your blood sugar levels.
-
2Talk about long-acting insulin with your doctor. Many diabetics need to be on long-acting insulin, no matter whether your type 1 or type 2. Long-acting insulin provides a steady flow of insulin throughout the day, and you typically take it by injection 2 times a day.[10]
- Remember that once you have been prescribed long-acting insulin, you’ll need to follow up continuously with your doctor to see if you still need the insulin or if the dosages need to be changed.
-
3Discuss short-acting insulin with your doctor if you're not on it. If you're not on short-acting or rapid-acting insulin and you're having trouble controlling your blood sugar, have a conversation with your doctor about it. You take short-acting or rapid-acting insulin before each meal to give your body the spike of insulin it needs.[11]
- Ask your doctor if this option is a good one for you. They may think so, or they may suggest changing your current morning and evening doses before adding short-acting or rapid-acting insulin into the equation.
- Also talk to your doctor about how your short-acting needs to be adjusted in coordination with your blood sugar readings. If your reading is too low, you may give yourself less or none at all. If your reading is too high, you may need to give yourself more short-acting insulin. Your doctor will likely give you a sliding scale, which will tell you how much short-acting insulin to take when your blood sugar is at certain levels.
- It may be a good idea to consider the different factors, such as eating or drinking alcohol, that may have caused your blood sugar level to rise before you resort to taking the short-acting insulin.
- Short-acting or rapid-acting insulin is especially beneficial for those that often exercise strenuously.
Testing and Regulating Blood Sugar
-
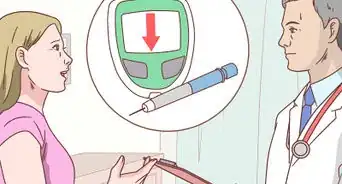
1Ask your doctor how often you should be checking your blood sugar. There's no set number for how many times a day a diabetic should check their sugar. The number of times you should use your meter is based on your individual needs, so talk to your doctor about it.[12]
- For instance, if you have type 1 diabetes, your doctor may recommend checking before each meal, as well as before bedtime and before and after exercising.
- If you have type 2 diabetes, your doctor may decide you don't need to check it as much. Often, they'll want you to check it before meals.
- If you're on insulin, you may have to check it before you give yourself the shot, as you may need to adjust your insulin intake based on your blood sugar levels for short-acting insulin.
-
2Test your blood sugar with a blood sugar meter. To test your blood sugar, begin by washing your hands. You're creating a small puncture wound, so you want to be as clean as possible! Turn your meter on and insert a test strip if that's how your meter works. Use the lancet to puncture the side of your fingertip, drawing up a drop of blood. Place the drop on the test strip and wait for your meter to read it.[13]
- You can squeeze your finger a bit if you're not getting enough blood.
- Some older meters require that you put the blood on the strip before inserting it into the meter.
- Typically, you want your results to be 70 mg/dl to 100 mg/dl before a meal and under 140 mg/dl after a meal.[14] However, talk to your doctor about your target range.
-
3Keep track of your results with an app for easy tracking. Tracking your blood sugar levels can help you see trends, which in turn can help you figure out how to better control your blood sugar. You'll also find plenty of apps that will keep track of your blood sugar readings for you.[15]
-
4Track your blood sugar with a pen and paper if you’d prefer the traditional approach. You can track your blood sugar levels the old fashioned way with a pen and paper. Just keep it with your meter so you can jot it down each time.[16] This may be very helpful when you have doctor’s appointments, as you can just bring it to the doctor’s office with you.
Making Lifestyle Changes
-
1Exercise regularly to regulate your blood sugar. Exercise helps you lose weight, which is good for diabetes management. It also burns off sugar from your blood, and it helps stimulate your body's production of insulin, both of which are helpful.[17]
- Aim for at least 30 minutes of exercise 5 times a week.
-
2Work on your stress levels. Stress can wreak havoc with your blood sugar levels, so keeping your stress in check is a good idea. Try to limit stress levels by saying "no" when you can, and incorporate stress-beating routines into your daily life.[18]
- Try adding yoga or meditation to your week, both of which can help stress levels.
- Use deep breathing when you find yourself getting stressed. Close your eyes, and breathe in to the count of 8. Hold the breath for 4 counts, then breathe out to the count of 8. Keep focusing on your breathing until you feel yourself calming down.
-
3Keep your alcohol consumption moderate. Check with your doctor first to make sure you can drink alcohol safely. If your doctor okays it, stick to moderate drinking, meaning no more than 1 drink a day for men who are over 65 and women and 2 drinks a day for men under 65.[19] .
- One drink equals 5 fluid ounces (150 ml) of beer, 12 fluid ounces (350 ml) of wine, or 1.5 fluid ounces (44 ml) of liquor.
- Eat something before you drink, and always count the carbohydrates you drank when tallying up your carbs for the day
-
4Quit smoking. If you smoke, you'll have a harder time controlling your blood sugars than if you quit. In addition, smoking puts you at a higher risk of complications from diabetes. Talk to your doctor about options to help you quit.[20]
References
- ↑ https://www.ucsfhealth.org/education/treating_low_blood_sugar/
- ↑ https://www.diabetesselfmanagement.com/blog/water-for-diabetes/
- ↑ https://my.clevelandclinic.org/health/articles/carbohydrates-and-blood-sugar-control-for-people-with-diabetes
- ↑ https://my.clevelandclinic.org/health/articles/carbohydrates-and-blood-sugar-control-for-people-with-diabetes
- ↑ https://www.hsph.harvard.edu/nutritionsource/what-should-you-eat/whole-grains/
- ↑ Lyssandra Guerra. Certified Nutrition & Wellness Consultant. Expert Interview. 25 March 2020.
- ↑ https://www.mayoclinic.org/diseases-conditions/diabetes/in-depth/diabetes-management/art-20047963
- ↑ https://www.health.harvard.edu/staying-healthy/the-truth-about-fats-bad-and-good
- ↑ https://my.clevelandclinic.org/health/diseases/7104-diabetes-mellitus-an-overview
- ↑ https://www.aafp.org/pubs/afp/issues/1999/0801/p649.html
- ↑ https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/diabetes-and-insulin
- ↑ https://www.niddk.nih.gov/health-information/diabetes/overview/managing-diabetes
- ↑ https://www.diabetes.org/healthy-living/medication-treatments/blood-glucose-testing-and-control/checking-your-blood-sugar
- ↑ https://www.diabetesselfmanagement.com/blog/what-is-a-normal-blood-sugar-level/
- ↑ https://www.cdc.gov/diabetes/managing/managing-blood-sugar/bloodglucosemonitoring.html
- ↑ https://www.cdc.gov/diabetes/managing/managing-blood-sugar/bloodglucosemonitoring.html
- ↑ https://health.clevelandclinic.org/exercise-and-your-glucose-levels-does-timing-make-a-difference/
- ↑ https://dtc.ucsf.edu/types-of-diabetes/type2/understanding-type-2-diabetes/how-the-body-processes-sugar/blood-sugar-stress/
- ↑ https://pubs.niaaa.nih.gov/publications/aa26.htm
- ↑ https://www.cdc.gov/tobacco/campaign/tips/diseases/diabetes.html
- ↑ Lyssandra Guerra. Certified Nutrition & Wellness Consultant. Expert Interview. 25 March 2020.
About This Article
To control your blood sugar with food, you’ll need to monitor your levels and work with your doctor so you can adjust your diet properly. If your blood sugar levels drop below 70 milligrams per deciliter, eat something sweet, like half a banana, to bring them up. Once you get your levels where you want them, drink 10 to 15 cups of water daily to keep them stable. You can also control your blood sugar levels by eating a balanced diet of whole grains, lean proteins, and vegetables. For more advice from our Medical co-author, including how to control your blood sugar levels with insulin, scroll down!



































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...