This article was co-authored by Roy Nattiv, MD. Dr. Roy Nattiv is a Board-Certified Pediatric Gastroenterologist in Los Angeles, California. With over 20 years of experience he specializes in a broad range of pediatric gastrointestinal and nutritional illnesses such as constipation, diarrhea, reflux, food allergies, poor weight gain, SIBO, IBD, and IBS. He completed his pediatric residency at the Children’s Hospital at Montefiore, Albert Einstein College of Medicine in New York, and his fellowship at the University of California, San Francisco (UCSF). While at UCSF, he was a California Institute of Regenerative Medicine (CIRM) fellowship trainee and was awarded the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition (NASPGHAN) Fellow to Faculty Award in Pediatric IBD Research. Dr. Nattiv received his undergrad degree from the University of California, Berkeley, and his medical degree (MD) from the Sackler School of Medicine in Tel Aviv, Israel.
There are 13 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 93,112 times.
Acid reflux, also known as gastroesophageal reflux disease (GERD), is a common stomach problem that can happen to anyone and at any age. Your esophagus is the tube that connects your mouth and throat to your stomach. The foods and beverages you consume pass through your esophagus and into your stomach, then continue to work their way through your digestive tract. Sometimes, the muscle at the bottom of your esophagus does not work properly, which allows for stomach acid and food particles to find their way back up into your esophagus and throat area. This causes the symptoms associated with acid reflux or GERD. The only way to be certain that you have acid reflux is to see your doctor for an evaluation and diagnosis.
Steps
Recognizing the Problem
-
1Identify the symptoms of acid reflux disease. The common signs of acid reflux disease include heartburn, chest pain, trouble swallowing, a chronic dry cough or hoarseness, sore throat, a sour taste in your mouth, regurgitation of food or sour tasting stomach juices, and a sensation of a lump in your throat.[1]
- ”Heartburn” is a term that is commonly used to describe some of these symptoms grouped together. The accepted definition of heartburn is indigestion involving a burning sensation in your mid chest area that can spread into your throat, often accompanied by a bitter taste.
- Less common symptoms of acid reflux include nausea, vomiting, wheezing, ear pain, laryngitis, persistent need to clear the throat, and erosion of tooth enamel and other dental problems.
- Acid reflux is responsible for as many as 50% of non-cardiac chest pain cases. Many people go to the emergency room or urgent care treatment center due to chest pain, thinking they may be having a heart attack.
- Always seek medical attention when sudden or potentially life-threatening symptoms occur. If no evidence of cardiac problems are found, follow up with your regular doctor to see if you may be experiencing acid reflux.
-
2Inform your doctor of your medical history. Provide as much detail as possible about your medical history. Treating your acid reflux effectively may depend on your doctor's knowledge of other diseases or problems.[2]
- This includes a complete history of any digestive problems you have had in the past, persistent sore throats, coughing, hoarseness or laryngitis, stomach pain, and any history of stomach ulcers or other GI disorders.
- Tell your doctor about any allergies you may have, especially since you may need to follow-up with testing procedures that use uncommon medications and contrast media.
- Include all medical conditions in the information you provide to your doctor, as well as any other doctors like radiologists and anesthesiologists that may be part of your healthcare team. Be sure to let them know if you think you may be pregnant.
Advertisement -
3Provide a complete list of your medications. The list should include all prescription medications you are taking, plus over-the counter products, vitamins, and herbal supplements. Always let each of your doctors know when a new medicine is added, you start something new that is over-the-counter, or an existing medication is changed or discontinued.
- Sometimes over-the-counter medications, herbal supplements, and vitamins that you may think are harmless, can be the primary cause of your stomach problem.
- Follow you doctor's instructions on how to safely stop and re-start you medications as you proceed with testing procedures.
-
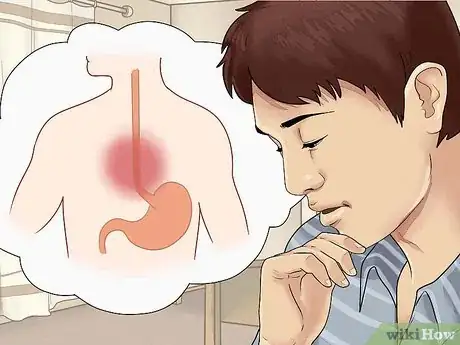
4Familiarize yourself with the different characterizations of acid reflux. Acid reflux generally falls into three categories. The categories are important to understand since they guide your doctor in determining the next step in confirming your diagnosis of acid reflux disease.[3]
- The first category is called functional or physiologic GERD.
- This category includes people that do not have risk factors for acid reflux or any medical conditions that may be contributing to the symptoms.
- People in this group are often treated with lifestyle changes or milder forms of medications. Diagnostic testing may not be needed to start treatment as long as no other medical conditions or risk factors are present. It is up to your doctor.
- The second category is called pathological reflux disease. People in this category develop acid reflux symptoms and possible complications due to more severe and lingering symptoms and sometimes have co-existing medical conditions that make their acid reflux worse.
- Persistent acid reflux that has not been treated for an extended period of time falls in this category.
- The third category is called secondary GERD. This means that another underlying medical condition may be causing or contributing to the development of acid reflux.
- For example, people that have a gastrointestinal disorder that causes problems with stomach emptying may develop acid reflux due to that condition.
-
5Take your symptoms seriously. Once you know you have acid reflux, follow the treatment suggestions provided by your doctor. If the treatment options provided do not seem to be working, then let your doctor know. Serious complications from acid reflux disease are possible.[4]
- The most common complication from acid reflux is called esophagitis. This means the esophagus becomes inflamed, irritated, or has areas of ulceration.
- This condition can get much worse over time if the acid reflux is not effective treated.
- Stricture is a complication that often develops in advanced forms of esophagitis. Stricture is commonly caused by continued exposure of the esophagus to stomach acid. Localized inflammation, scar tissue, or other tissue damage to the esophagus, cause it to become rigid and/or tight which makes it difficult for food to pass and difficult to swallow.
- People with a stricture from prolonged acid reflux disease often have trouble with vomiting undigested foods or difficulty swallowing solid food. In many cases, this requires surgery to repair.
- Another complication that may arise is called Barrett esophagus and occurs in approximately eight to 15% of people with acid reflux. Long-term exposure of the esophagus to stomach acid causes changes at the cellular level leading to dysplasia.
- Dysplasia is a change that is observed in tissues during the early development of cancer.
- The development of Barrett esophagus can lead to a type of cancer called adenocarcinoma, which is the most common type of esophageal cancer.[5] This is the most serious complication associated with GERD.
Participating in Diagnostic Testing
-
1Be aware of the common methods to diagnose acid reflux. Doctors rely heavily on symptoms and response to treatment for diagnosis. The doctor must rule out alternative diagnoses that may masquerade as GERD: functional heartburn, atypical cases of achalasia, or distal esophageal spasm. Based on your symptoms, you will likely be prescribed a proton pump inhibitor (PPI). These block the acid production in the stomach.[6] If there is no response to these medications, your doctor may try additional tests. The specific tests as suggested below are usually only used if there is unclear diagnosis for GERD, or if there are more serious symptoms.
- Some testing, such as esophageal manometry, is recommended for preoperative evaluation.
- Endoscopy is recommended in the presence of alarm symptoms and for screening of patients at high risk for complications.
-
2Have an upper GI endoscopy. An upper GI endoscopy procedure helps to evaluate the overall anatomy and identify any structural problems or complications from the disease. This test confirms the presence of acid reflux disease and is useful determining the extent of damage to the esophagus. Other upper GI conditions are also diagnosed by this method.[7]
- Examples of other conditions diagnosed by doing an upper GI endoscopy include anemia, unexplained nausea and vomiting, ulcers, bleeding, and precancerous abnormalities.
- An upper GI is done by inserting an endoscope, which is a long and flexible tube with a camera on the end, down the throat and into the esophagus. This allows the examiner to see the lining of your upper GI areas including your esophagus.
-
3Prepare for an upper GI endoscopy. Your doctor will give you clear instructions to follow prior to the procedure. Follow the directions provided by your doctor. The items listed here are provided for information only, and may differ from those provided by your doctor.[8]
- Do not eat or drink anything for at least eight hours before the procedure. In order for the doctor to clearly see the lining of your esophagus and stomach area, your stomach needs to be empty.
- This includes smoking, eating any food, drinking any beverages including water, and chewing gum.
- Upper GI endoscopies are usually done in a hospital or outpatient surgical center since mild sedation is provided.
- Be sure you have a ride home. You will be given a mild form of anesthesia so you will not be allowed to drive immediately after.
- Some doctors will perform this procedure without using sedation, but this is not commonly done.
-
4Know what to expect during the procedure and immediately after. You may be asked to gargle with, or spray, a liquid anesthetic on the back of your throat. This helps to stop the gag reflex as the tube is inserted.[9]
- You will lie on your side on an exam table during the procedure. An IV will be started in your arm or hand so you can be given the medication for sedation. Nurses or other doctors will be with you to monitor your vital signs throughout the procedure.
- The examiner will insert a long, thin, tube with a camera on the end into your mouth and gently push it through your esophagus and into your stomach area. This allows the examiner to look closely at the tissues in your upper GI tract and stomach area.
- If necessary, the doctor may take a biopsy of tissues during the examination. This is done by using an instrument carefully inserted through the tube that has been passed into your upper GI area. You will not feel any pain from the biopsy.
- Sometimes air is pumped into the stomach and duodenum, which is the uppermost part of your intestine. This helps the examiner to see all the tissues and linings to better determine the cause of the problem.
- The entire procedure usually takes between 15 and 30 minutes. In many cases, the doctor can give you immediate feedback on what was found. Tissue biopsies take several days to get the results.
- You will stay at the hospital or center for several hours after the procedure to allow time for you to wake up from the sedatives used, and to be sure there are no problems as a result of the procedure.
- Many people feel bloated and nauseous for a few hours and have a sore throat for one or two days following the procedure. You can expect to rest at home for the rest of the day and possibly the following day. Resume your normal diet once your sore throat has subsided and you do not have any trouble swallowing.
-
5Have a manometry study done. Manometry studies are done to provide detailed information on people that may be surgical candidates. The procedure allows the doctor to evaluate how well the esophagus is functioning and if there is are problems that can be corrected with surgery.[10]
- Manometry is a procedure that provides important information about the overall function of the esophagus and the sphincter at the bottom that normally tightens or closes once food has passed through.
- During the manometry, the doctor will be able to measure the pressure of the lower esophageal sphincter, check for problems with motility, evaluate the contraction and relaxation of the esophagus, and identify other problems that may be related to swallowing.
-
6Prepare for a manometry study. Your doctor will provide specific instructions for you to follow to prepare for your manometry study. Follow the guidelines exactly as your doctor outlined.[11]
- You will likely be told not to eat or drink anything for at least eight hours before the test is to be done. If it is scheduled for first thing in the morning, then you should not eat or drink anything after midnight the night before.
-
7Know what to expect before and immediately following the procedure. You will not be sedated during the test but medication is used to make the procedure more comfortable.[12]
- Medications that numb your throat area and nasal passages are used just before the procedure starts. The medication makes the insertion of the tube more comfortable.
- The procedure involves passing a thin, pressure-sensitive tube through your nose, down your throat and esophagus, an into your stomach. You will likely be sitting upright when the tube is inserted.
- You may feel a gagging sensation and some discomfort as the tube is passed through your nose and throat.
- The tube is pulled back slightly once it reaches the stomach to be sure it is in your esophagus. You may remain seated or be asked to recline on your back for the rest of the procedure.
- Once the tube is in the proper place, you will be asked to swallow small sips of water. The catheter, or tube, is connected to a computer and can take important readings as you swallow.
- Breathe slowly and regularly, remain as still as possible, and swallow only when asked to do so.
- The computer readings can determine if the sphincter muscles in your esophagus are normal. The procedure also checks the overall function of the esophagus with regards to proper contraction, relaxation, and motility.
- You may have a slight nosebleed, watery eyes, and sore throat, during and following the procedure. It is possible, but very rare, for your esophagus to be damaged during the procedure.
- Your doctor will advise you when you can resume normal eating and drinking, which is normally immediately after the procedure is completed.
- The entire procedure takes about 30 minutes to an hour. It is usually done in a hospital or surgical center setting.
- Expect several days for the final test results to be available.
Undergoing Other Testing Procedures
-
1Consider optional procedures. Your doctor may need additional information about your condition to properly treat your acid reflux. Other tests are sometimes done to evaluate people with acid reflux and related problems, in addition to the mandatory diagnostic testing.
- The two most common tests done to confirm a diagnosis of acid reflux, or to explore problems with similar symptoms, include a 24 hour pH probe exam and an upper GI series.
- These procedures are helpful in diagnosing related conditions, such as peptic ulcer disease, and in monitoring the progress of treatment interventions.
- Once treatment has been started for acid reflux, it is important to evaluate the effectiveness of treatment. Often this can be done by monitoring symptoms, but sometimes repeating a procedure to compare the results is the most effective way.
-
2Have a 24 hour pH probe exam.[13] The 24 hour pH probe exam is used to confirm the diagnosis of acid reflux disease in people that have acid reflux symptoms that are not the most common ones, and if the results of the endoscopy were not conclusive.[14]
- It is also used to determine the effectiveness of some treatments, and to find the cause of other problems like nighttime coughing or hoarseness.
- The test measures the pH of the esophagus over a 24 hour period. This helps your doctor to know if acid is in the esophagus when it shouldn't be.
- Your doctor will provide you with complete instructions on how to prepare for the test. Commonly instructions recommend no food or water for 2 hours before the procedure.
- During the procedure, a numbing medication will be placed in your nasal passages to make the insertion of the tube more comfortable. Once the tube is in place, it will be taped down against your face and nose to keep it in place.
- A small carrying case/backpack that contains a recording unit is attached to the tube. You will also be given a diary to record specific details of symptoms, when you eat or drink, and other information you doctor needs to know.
- The recording unit collects data for 24 hours. This information will be correlated with your diary entries to determine if there are problems with abnormal acid levels in your esophagus. After 18 to 24 hours, you will return to the hospital or clinic and the tube will be removed.
- Maintain your normal routines as much as possible to provide accurate readings and information.
-
3Have an upper GI series performed. An upper GI series uses fluoroscopy, or constant and real-time x-rays, to create images of the esophagus, stomach, and small intestine. The procedure is non-invasive and uses a barium contrast material to look for problems in your upper gastrointestinal tract. Many possible medical conditions, including acid reflux, can be diagnosed or confirmed using an upper GI series.[15]
- Your doctor will provide you with detailed instructions on how to prepare for the procedure. Most of the time, you will be asked not to chew gum, or eat or drink anything, including your routine medications, for several hours before the procedure.
- The procedure will be done in a hospital, clinic, or surgical center. You will be monitored by a radiologist since fluoroscopy is involved. Fluoroscopy is a form of x-ray.
- Jewelry, some dental appliances, eye glasses, and other metal objects will need to be removed before the procedure begins. You will be asked to wear a hospital gown for the procedure.
- You will be asked to drink some form of contrast media, such as barium. Next you will be asked to lie down on a special table that is part of the fluoroscopy equipment. This makes your organs visible to the equipment so the radiologist can see how they are working in real-time.
- Pictures are taken as the contrast medium travels through your upper GI tract. The table may tilt or move during the procedure so the images can be as thorough as possible. The entire exam takes about 20 to 30 minutes.
- During and after the exam, you may feel bloated if certain types of gas-producing materials were used.
- In most cases, you can resume your normal diet and regular medications immediately following the exam. The barium may cause your stools to be gray or white and you may feel constipated for two to three days following the procedure. Drink extra fluids if needed to help your body resume a regular schedule.
- The radiologist will review the results of your study and send a full report to your doctor. Your doctor will talk with you about the results of the procedure.
Expert Q&A
Did you know you can get expert answers for this article?
Unlock expert answers by supporting wikiHow
-
QuestionWhat is laryngopharyngeal reflux?
 Roy Nattiv, MDDr. Roy Nattiv is a Board-Certified Pediatric Gastroenterologist in Los Angeles, California. With over 20 years of experience he specializes in a broad range of pediatric gastrointestinal and nutritional illnesses such as constipation, diarrhea, reflux, food allergies, poor weight gain, SIBO, IBD, and IBS. He completed his pediatric residency at the Children’s Hospital at Montefiore, Albert Einstein College of Medicine in New York, and his fellowship at the University of California, San Francisco (UCSF). While at UCSF, he was a California Institute of Regenerative Medicine (CIRM) fellowship trainee and was awarded the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition (NASPGHAN) Fellow to Faculty Award in Pediatric IBD Research. Dr. Nattiv received his undergrad degree from the University of California, Berkeley, and his medical degree (MD) from the Sackler School of Medicine in Tel Aviv, Israel.
Roy Nattiv, MDDr. Roy Nattiv is a Board-Certified Pediatric Gastroenterologist in Los Angeles, California. With over 20 years of experience he specializes in a broad range of pediatric gastrointestinal and nutritional illnesses such as constipation, diarrhea, reflux, food allergies, poor weight gain, SIBO, IBD, and IBS. He completed his pediatric residency at the Children’s Hospital at Montefiore, Albert Einstein College of Medicine in New York, and his fellowship at the University of California, San Francisco (UCSF). While at UCSF, he was a California Institute of Regenerative Medicine (CIRM) fellowship trainee and was awarded the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition (NASPGHAN) Fellow to Faculty Award in Pediatric IBD Research. Dr. Nattiv received his undergrad degree from the University of California, Berkeley, and his medical degree (MD) from the Sackler School of Medicine in Tel Aviv, Israel.
Board Certified Gastroenterologist
References
- ↑ https://my.clevelandclinic.org/health/diseases/17019-gerd-or-acid-reflux-or-heartburn-overview#symptoms-and-causes
- ↑ https://oxfordmedicaleducation.com/history/medical-general/
- ↑ https://my.clevelandclinic.org/health/diseases/17019-gerd-or-acid-reflux-or-heartburn-overview
- ↑ https://www.cheyenneregional.org/service/gastroesophageal-reflux-disease-gerd-treatment/complications/
- ↑ http://www.cancercenter.com/terms/adenocarcinoma/
- ↑ http://www.aboutgerd.org/site/treatment/medications/ppi
- ↑ http://gi.org/guideline/diagnosis-and-managemen-of-gastroesophageal-reflux-disease/
- ↑ https://www.niddk.nih.gov/health-information/diagnostic-tests/upper-gi-endoscopy
- ↑ https://www.niddk.nih.gov/health-information/diagnostic-tests/upper-gi-endoscopy
- ↑ https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/esophageal-manometry
- ↑ https://www.nlm.nih.gov/medlineplus/ency/article/003884.htm
- ↑ https://www.nlm.nih.gov/medlineplus/ency/article/003884.htm
- ↑ https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/24-hour-ph-impedance-testing
- ↑ http://www.gikids.org/files/documents/digestive%20topics/english/Ph%20Probe%20-%20English.pdf
- ↑ http://www.radiologyinfo.org/en/info.cfm?pg=uppergi
About This Article
If you are experiencing symptoms such as heartburn, chest pain, trouble swallowing, a chronic dry cough, sore throat, nausea, or the sensation of a lump in your throat, see your doctor, who will most likely diagnose your condition as acid reflux. Be sure to provide your doctor with your full medical history and a complete list of the medications you use, since treatment for acid reflux can depend on other conditions you may have. Your doctor will probably prescribe you a proton pump inhibitor to block the acid production in your stomach. However, let them know if the medication doesn't seem to be working, so they can do additional tests, such as an esophageal manometry or endoscopy. For more advice from our Medical co-author, including how to prepare for an endoscopy to diagnose your acid reflux, scroll down.



































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...