This article was co-authored by Siddharth Tambar, MD. Dr. Siddharth Tambar, MD is a board certified rheumatologist at Chicago Arthritis and Regenerative Medicine in Chicago, Illinois. With over 19 years of experience, Dr. Tambar specializes in Regenerative Medicine and Rheumatology, with a focus on platelet rich plasma and bone marrow derived stem cell treatments for arthritis, tendinitis, injuries, and back pain. Dr. Tambar holds a BA in Economics from State University of New York at Buffalo. He earned his MD from State University of New York at Syracuse. He completed his Internship, Residency in Internal Medicine, and his Rheumatology Fellowship at Northwestern Memorial Hospital. Dr Tambar is board certified in both rheumatology and internal medicine. He also holds Musculoskeletal Ultrasound Diagnostic and Interventional certifications from the American College of Rheumatology and the American Institute of Ultrasound in Medicine.
There are 10 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 30,428 times.
Septic arthritis, also called infectious arthritis, is an infection of a joint.[1] Bacteria or a virus that spreads to a joint or its surrounding fluid causes septic arthritis. In most cases, the infection starts in another part of the body and circulates through the bloodstream into the joint. People who develop septic arthritis usually have it in only one large joint such as the knee, hip or shoulder. You can diagnose septic arthritis by identifying its symptoms and seeking professional assessment.
Steps
Determining Physical and Behavioral Symptoms
-
1Recognize risk factors. Individuals of any age can develop septic arthritis. However, some people may be more susceptible to this condition. Children, older adults, and illegal drug users are more likely to have septic arthritis. Other risk factors include:[2]
- Having existing joint problems such as gout or lupus.
- Taking medication for rheumatoid arthritis.
- Having fragile skin that breaks easily.
- Having a weakened immune system.
- Having joint trauma such as animal bites or puncture wounds.
- Having recent surgery.[3]
- Taking immunosuppressants.
-
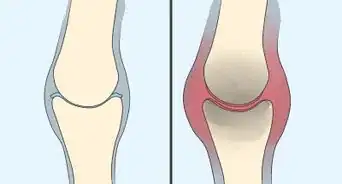
2Watch for swelling. Septic arthritis generally comes on quickly.[4] Symptoms are usually in one joint, though in rare cases may affect two or more areas.[5] One of the most common symptoms of septic arthritis is swelling around the affected joint.[6] This is caused by a buildup of infected fluid around your joint. Watching for swelling in one joint can help you diagnose septic arthritis.
- Pay attention to any warmth and redness that accompanies the swelling. This can also indicate septic arthritis.
Advertisement -
3Notice pain and immobility in the joint. The swelling caused by septic arthritis infection can also bring on mild to severe pain. It can also lead to an inability to fully move your joint.[7] Watching for any pain and immobility in the joint can help you diagnose septic arthritis and seek prompt treatment.
- Recognize that your pain may get worse when you move the affected joint.
- Avoid forcing a painful joint to move. Septic arthritis may also lead to an inability to move the joint.[8]
- Listen for crying or whimpering in infants and small children when the joint is moved. This is a sign of pain and may indicate that the child is suffering from septic arthritis.
-
4Check for a fever. Infections, including septic arthritis, are often accompanied by a fever and chills.[9] This is a sign that something out of the ordinary is happening in the body.[10] Taking the temperature can indicate a fever which may be the result of septic arthritis.
- Recognize that chills, muscle aches, sweating, and headache are common symptoms of a fever.[11] These may also accompany a fever with septic arthritis.
- Seek immediate medical attention if your fever is higher than 103 degrees Fahrenheit (39.4 degrees Celsius). In a small child, contact your doctor as soon as you realize they have even a slightly elevated temperature. This can indicate a serious infection.
-
5Observe fatigue and weakness. Two symptoms that are common with a fever are fatigue and weakness.[12] These can also accompany septic arthritis. If you experience fatigue and weakness along with other symptoms of septic arthritis, you may have the condition.
- Recognize typical symptoms of weakness and fatigue, which include: delayed or slow movement, muscle cramps, muscle twitching, and uncontrollable shaking. Feeling run down is the most common symptom of fatigue.
- Be aware that your fatigue and weakness may lead to a decreased appetite, which can also signal septic arthritis.
-
6Detect irritability. Most symptoms of septic arthritis are physical. However, some may be emotional or behavioral, especially in infants and small children. Noticing if you or another person are irritable can indicate septic arthritis, especially when in conjunction with other symptoms.
- Look for fussiness in children and infants. This can accompany any irritability they have.[13]
Seeking a Professional Diagnosis
-
1Schedule an appointment with your doctor. Only your doctor can definitively diagnose septic arthritis. If you have sudden onset of severe pain in a joint or any other symptoms of septic arthritis, contact your doctor as soon as possible. Prompt diagnosis of septic arthritis can minimize potential joint damage, including degeneration.[14]
- Schedule the first available appointment by letting the doctor’s staff know that you have the symptoms of septic arthritis.
- Seek emergency medical attention if your doctor is unable to see you. Emergency rooms and emergency care centers can also diagnose septic arthritis.
-
2Undergo an examination. During your appointment or exam, explain to the doctor that you suspect you may have septic arthritis. Discuss any symptoms you are experiencing as well as other relevant information, such as if you recently had surgery or a puncture wound. Your doctor will consider this information while examining your joint for signs of septic arthritis.
- Answer any questions the doctor may have honestly. Remember the doctor is trying to make a proper diagnosis and formulate the best treatment plan to minimize the risk of more serious conditions. If you are an illegal drug user, this information could be important information for a diagnosis.
-
3Get your blood and joint fluid tested. Depending on the examination, your doctor may order additional tests. These can give a more definitive diagnosis of septic arthritis.[15] Your doctor may prescribe the following additional tests:
- Arthrocentesis, which requires inserting a small needle into the joint for a sample of the synovial fluid. This test can indicate the presence of bacteria.[16] It can also assess your white blood cell count. It can also help your doctor figure out what medications to prescribe as treatment.[17] Synovial fluid with greater than 50,000 white cells with a predominance of Polymorphonuclear Leukocytes (PMN) is significant for the disease and needs treatment. Other than the cell count, a doctor will do a gram stain of the synovial fluid as well as a culture of the fluid. This will help guide treatment.
- Blood culture, which requires taking blood with a small needle.[18] A blood culture can determine what signs of infection are in your blood.[19] This test can help your doctor figure out the severity of infection in your joint.
-
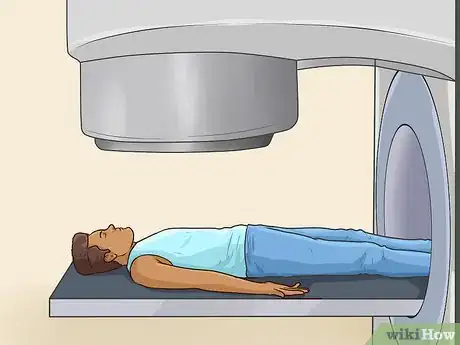
4Have imaging tests. In addition to joint fluid and blood tests, your doctor may also call for imaging tests. These can confirm the presence of infection as well as if your joint is damaged.[20] Imaging tests often used for diagnosing septic arthritis include:
- X-rays.
- MRI scans.
- CT scans.
- Bone scans.
- Ultrasound.
-
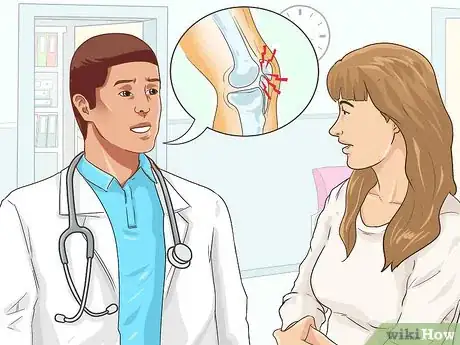
5Receive a diagnosis. Based on the outcome of an examination and any testing, your doctor may diagnose you with septic arthritis. Your doctor will talk to you about the results of your testing, including any damage in your joint. Your doctor will also discuss your treatment options.
- Ask your doctor any questions you may have about the diagnosis or treatment.
- If you have a MRSA infection you will need to treated with IV antibiotics such as vancomycin. This is the safest option for treatment given the prevalence of MRSA in hospitals and the community.
Expert Q&A
-
QuestionCan a blood test detect septic arthritis?
 Siddharth Tambar, MDDr. Siddharth Tambar, MD is a board certified rheumatologist at Chicago Arthritis and Regenerative Medicine in Chicago, Illinois. With over 19 years of experience, Dr. Tambar specializes in Regenerative Medicine and Rheumatology, with a focus on platelet rich plasma and bone marrow derived stem cell treatments for arthritis, tendinitis, injuries, and back pain. Dr. Tambar holds a BA in Economics from State University of New York at Buffalo. He earned his MD from State University of New York at Syracuse. He completed his Internship, Residency in Internal Medicine, and his Rheumatology Fellowship at Northwestern Memorial Hospital. Dr Tambar is board certified in both rheumatology and internal medicine. He also holds Musculoskeletal Ultrasound Diagnostic and Interventional certifications from the American College of Rheumatology and the American Institute of Ultrasound in Medicine.
Siddharth Tambar, MDDr. Siddharth Tambar, MD is a board certified rheumatologist at Chicago Arthritis and Regenerative Medicine in Chicago, Illinois. With over 19 years of experience, Dr. Tambar specializes in Regenerative Medicine and Rheumatology, with a focus on platelet rich plasma and bone marrow derived stem cell treatments for arthritis, tendinitis, injuries, and back pain. Dr. Tambar holds a BA in Economics from State University of New York at Buffalo. He earned his MD from State University of New York at Syracuse. He completed his Internship, Residency in Internal Medicine, and his Rheumatology Fellowship at Northwestern Memorial Hospital. Dr Tambar is board certified in both rheumatology and internal medicine. He also holds Musculoskeletal Ultrasound Diagnostic and Interventional certifications from the American College of Rheumatology and the American Institute of Ultrasound in Medicine.
Board Certified Rheumatologist It may, but more likely your doctor will test a small sample of the fluid in your affected joint.
It may, but more likely your doctor will test a small sample of the fluid in your affected joint.
References
- ↑ Siddharth Tambar, MD. Board Certified Rheumatologist. Expert Interview. 25 August 2020.
- ↑ https://www.hopkinsmedicine.org/health/conditions-and-diseases/arthritis/septic-arthritis
- ↑ https://medlineplus.gov/ency/article/000430.htm
- ↑ https://medlineplus.gov/ency/article/000430.htm
- ↑ http://www.arthritis.org/about-arthritis/types/infectious-arthritis/
- ↑ Siddharth Tambar, MD. Board Certified Rheumatologist. Expert Interview. 25 August 2020.
- ↑ Siddharth Tambar, MD. Board Certified Rheumatologist. Expert Interview. 25 August 2020.
- ↑ https://medlineplus.gov/ency/article/000430.htm
- ↑ Siddharth Tambar, MD. Board Certified Rheumatologist. Expert Interview. 25 August 2020.
- ↑ https://www.hopkinsmedicine.org/health/conditions-and-diseases/arthritis/septic-arthritis
- ↑ https://www.hopkinsmedicine.org/health/conditions-and-diseases/arthritis/septic-arthritis
- ↑ https://www.versusarthritis.org/about-arthritis/conditions/septic-arthritis/
- ↑ https://medlineplus.gov/ency/article/000430.htm
- ↑ http://www.mayoclinic.org/diseases-conditions/bone-and-joint-infections/symptoms-causes/dxc-20166654
- ↑ http://www.arthritis.org/about-arthritis/types/infectious-arthritis/
- ↑ Siddharth Tambar, MD. Board Certified Rheumatologist. Expert Interview. 25 August 2020.
- ↑ http://www.mayoclinic.org/diseases-conditions/bone-and-joint-infections/diagnosis-treatment/diagnosis/dxc-20166670
- ↑ https://medlineplus.gov/ency/article/000430.htm
- ↑ http://www.mayoclinic.org/diseases-conditions/bone-and-joint-infections/diagnosis-treatment/diagnosis/dxc-20166670
- ↑ http://www.mayoclinic.org/diseases-conditions/bone-and-joint-infections/diagnosis-treatment/diagnosis/dxc-20166670































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...