This article was medically reviewed by Janice Litza, MD. Dr. Litza is a board certified Family Medicine Physician in Wisconsin. She is a practicing Physician and taught as a Clinical Professor for 13 years, after receiving her MD from the University of Wisconsin-Madison School of Medicine and Public Health in 1998.
There are 10 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 15,681 times.
No matter what type of ulcer you’re dealing with, working with your doctor to develop a treatment plan comprised of medication and pain management techniques is the fastest, most effective way to heal it. For peptic ulcers, antibiotics or PPIs may be necessary. Leg ulcers are generally treated through compression therapy. Rectal ulcers can often be managed with lifestyle changes. Be sure to talk to your doctor prior to starting any treatment to ensure that you’re using the most appropriate methods to treat your individual problem.
Steps
Treating Peptic Ulcers
-
1Make a doctor’s appointment to determine the cause of your ulcer. The type of treatment you need will depend upon what is causing your ulcer. If you don’t already know the cause, talk to your doctor about diagnostic options. They may suggest laboratory testing, endoscopy, and/or x-rays, and will be able to refer you to any necessary specialists.[1]
-
2Use antibiotics to treat H pylori infections. A course of antibiotics is the fastest and most effective way to treat peptic ulcers caused by H. pylori infections. After diagnosis, your doctor will be able to write you a prescription. Take the full course of antibiotics as recommended by your doctor or pharmacist, even if you start to feel better.[2]
- If you experience any severe side-effects like nausea or diarrhoea advanced enough to inhibit your daily life, talk to your doctor. They can help you find a more appropriate medication for your needs.
Advertisement -
3Use Proton Pump Inhibitors (PPIs) to treat NSAID-induced ulcers. If your ulcer is caused by NSAID use, your doctor may prescribe PPIs to help reduce your stomach acid and coat your ulcer. Common PPIs include esomeprazole, dexlansoprazole, omeprazole, pantoprazole, and rabeprazole.[3]
- In addition to PPIs, your doctor may prescribe histamine receptor blockers, which block signals in your body to produce more stomach acid.
- If you need to continue use of NSAIDs for conditions such as arthritis, talk to your doctor about the safest way to continue your regimen. Your doctor may suggest taking something like deglycyrrhizinated licorice (DGL) tablets with the NSAIDS to reduce irritation.
-
4Try bismuth subsalicylate and antacids to manage symptoms. Medicines containing bismuth subsalicylate, such as Pepto-Bismol, coat peptic ulcers and protect them from stomach acid. In addition to antacids, which can temporarily treat ulcer pain, these medications can be used to temporarily manage ulcer symptoms.[4]
- Your doctor may prescribe a medication with bismuth subsalicylate in conjunction with antibiotics.
-
5Treat pain with unverified home remedies such as aloe vera juice and apple cider vinegar. Half a cup (100 ml) of aloe vera juice twice a day may help relieve some stomach ulcer pain. In addition, adding a tablespoon of apple cider vinegar to a glass of warm water once a day may help ease discomfort caused by ulcers. There is little scientific evidence to support these, but some ulcer patients report positive results after using these home remedies.[5]
- In addition to these, some ulcer sufferers report positive results managing ulcer-related symptoms using tea. Ginger and fennel teas can both help sooth the stomach, and chamomile tea can help ease pain and cramping.[6]
-
6Defend against ulcers using cabbage, bananas, and cayenne. Some research suggests that bananas, cabbage, and cayenne can all help prevent stomach ulcers. Eat a banana or a serving of cabbage on a daily basis, and incorporate cayenne in your dishes to help prevent the growth of H. pylori.[7]
- While there is some research to support these claims, the results are not conclusive. Talk to your doctor before making any major dietary changes.
- These dietary home remedies are meant to help prevent future ulcers, and have not been studied extensively as a treatment for existing ulcers.
Caring for Venous Ulcers
-
1Seek out a medical professional for compression therapy. Your doctor or nurse practitioner will start by clearing out all debris and dead tissue from the ulcer and apply a simple, non-stick dressing. They will then apply a compression bandage over the affected leg. Dressing and bandages typically need to be changed once a week.[8]
- Your medical professional may be able to show you how to change and wrap your bandages so that you do not need to revisit them on a weekly basis.
- If your ulcer is still healing, initial compression may hurt. Talk to your nurse or doctor about an appropriate pain management program to help you deal with any discomfort.
-
2Keep your legs elevated to reduce swelling. Venous ulcers can lead to fluid buildup in your legs, which can cause your feet and ankles to swell. Keep your legs elevated whenever you can. If possible, keep your ankles at the same elevation as your eyes. Sit in a reclining fashion and use pillows, sofa cushions, or foam wedges to prop up your legs while you sleep or relax.[9]
-
3Wear compression socks to keep the ulcer from returning. Once your ulcer heals, your doctor or nurse may recommend wearing compression socks or stockings to keep it from returning. They will be able to recommend the appropriate socks and let you know where you can purchase them locally.[10]
- These socks or stockings are generally more tight-fitting than regular support tights.
-
4Look into surgery for ulcers that won’t heal. On rare occasions, large or resistant ulcers may require a skin graft or surgery on the veins to fully heal. If your ulcer does not start healing properly within 3-4 months, talk to your doctor to see if surgery will be necessary to completely heal the affected area.[11]
Managing Rectal Ulcers
-
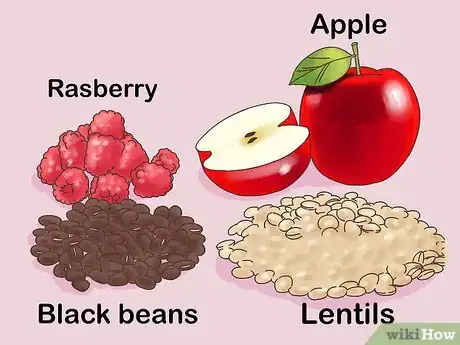
1Increase fiber intake to deal with rectal ulcer syndrome. Mild rectal ulcer symptoms can often be treated with lifestyle changes, including switching to a diet with increased fiber intake.[12] An adult male should aim to eat at least 30 g of fiber a day, while a female should aim for at least 25 g. Try foods including:[13]
- Raspberries
- Apples
- Pears
- Whole wheat pasta
- Barley
- Lentils
- Black beans
- Artichokes
- Green peas
-
2Use behavioral therapy to stop bowel strain. Some people naturally experience bowel strain or may strain out of habit. By working with a specialist, those who experience strain may eventually learn to control straining habits such as clenching pelvic floor muscles. Talk to your doctor about finding a specialist in your area if you find you strain in a way that hurts your ulcer or makes it worse.[14]
-
3Ask about surgical options. Surgery may be necessary in extreme cases for ulcers that struggle to heal. If rectal prolapse is causing your symptoms, your doctor may recommend a rectopexy to ensure that your rectum is in the correct position.[15]
References
- ↑ https://www.mayoclinic.org/diseases-conditions/peptic-ulcer/diagnosis-treatment/drc-20354229
- ↑ https://www.nhs.uk/conditions/stomach-ulcer/treatment/
- ↑ https://www.niddk.nih.gov/health-information/digestive-diseases/peptic-ulcers-stomach-ulcers/treatment
- ↑ https://www.niddk.nih.gov/health-information/digestive-diseases/peptic-ulcers-stomach-ulcers/treatment
- ↑ https://www.mayoclinic.org/drugs-supplements-aloe/art-20362267
- ↑ Petry JJ, Hadley SK. Medicinal herbs: answers and advice, Part 2.Hosp Pract (1995). 2001 Aug 15;36(8):55-9.
- ↑ https://www.thealternativedaily.com/how-to-treat-stomach-ulcer-naturally/
- ↑ https://www.nhs.uk/conditions/leg-ulcer/treatment/
- ↑ https://www.nhs.uk/conditions/leg-ulcer/treatment/
- ↑ https://www.circulationfoundation.org.uk/help-advice/veins/leg-ulcers
- ↑ https://www.circulationfoundation.org.uk/help-advice/veins/leg-ulcers
- ↑ https://www.mayoclinic.org/diseases-conditions/rectal-ulcer/basics/treatment/con-20027352
- ↑ https://www.mayoclinic.org/healthy-lifestyle/nutrition-and-healthy-eating/in-depth/high-fiber-foods/art-20050948
- ↑ https://www.mayoclinic.org/diseases-conditions/rectal-ulcer/basics/treatment/con-20027352
- ↑ https://www.mayoclinic.org/diseases-conditions/rectal-ulcer/basics/treatment/con-20027352

































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...