This article was co-authored by Roy Nattiv, MD and by wikiHow staff writer, Jessica Gibson. Dr. Roy Nattiv is a Board-Certified Pediatric Gastroenterologist in Los Angeles, California. With over 20 years of experience he specializes in a broad range of pediatric gastrointestinal and nutritional illnesses such as constipation, diarrhea, reflux, food allergies, poor weight gain, SIBO, IBD, and IBS. He completed his pediatric residency at the Children’s Hospital at Montefiore, Albert Einstein College of Medicine in New York, and his fellowship at the University of California, San Francisco (UCSF). While at UCSF, he was a California Institute of Regenerative Medicine (CIRM) fellowship trainee and was awarded the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition (NASPGHAN) Fellow to Faculty Award in Pediatric IBD Research. Dr. Nattiv received his undergrad degree from the University of California, Berkeley, and his medical degree (MD) from the Sackler School of Medicine in Tel Aviv, Israel.
There are 19 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 30,832 times.
If you suffer from gastric ulcers (a type of peptic ulcer), your stomach lining has been damaged by acid erosion. Gastric ulcers aren't caused by anything you ate. Instead, they're usually caused by a bacterial infection or by frequent use of nonsteroidal anti-inflammatory drugs. Regardless of whether the pain is mild or severe, you should get medical attention to treat the cause of the gastric ulcer.
Steps
Getting Medical Treatment
-
1Take antibiotics. If your gastric ulcer was caused by an H. pylori infection, your doctor will prescribe antibiotics.[1] These will kill the bacteria so the ulcer can heal. Fortunately, you won't need to take antibiotics for a prolonged period of time.
- You'll probably need to take antibiotics for two weeks.[2] Be sure to take the full course of treatment so the bacteria doesn't return. Even if your symptoms resolve, this doesn't mean you can stop the medication. Make sure you take every single dose of antibiotics as instructed by your doctor.
-
2Use acid-blocking medications. You'll most likely need to take proton pump inhibitors which block stomach acid. Prescription or over-the-counter medications may include: omeprazole, lansoprazole, rabeprazole, esomeprazole, pantoprazole.[3]
- Proton pump inhibitors do have some long-term side effects which include an increased risk of pneumonia, osteoporosis, and intestinal infections.
Advertisement -
3Take antacids. Your doctor may also prescribe antacids to decrease the production of stomach acid, protecting and healing your stomach lining.[4] This can help relieve pain from gastric ulcers. You may experience constipation or diarrhea as side effect.[5]
- Antacids treat the symptoms of gastric ulcer, but you'll need to take other medications to treat the cause of your gastric ulcer.
-
4Switch the pain medications you take. Regularly taking NSAIDs (Non-Steroidal Anti-Inflammatory Drugs) is one of the main causes of gastric ulcers. If you often use aspirin, ibuprofen, naproxen, or ketoprofen, consider changing pain medications.[6] Ask your doctor about using acetaminophen for pain relief since it's not associated with ulcers. Always follow the manufacturer's dosing instructions and don't take more than 3000 to 4000 mg a day.
- Try not to take pain medications on an empty stomach. This can be hard on your stomach. Instead, take pain medications with a meal or snack.
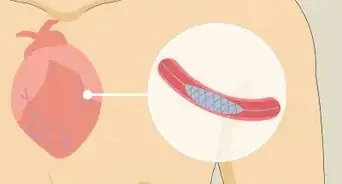
- Your doctor may also prescribe you carafate (sucralfate), which coats the ulcer from within your stomach, allowing your stomach to heal itself.[7]
-
5Stop smoking. Smoking can contribute to ulcers by wearing down the protective lining of the stomach. It also increases stomach acid which can cause upset stomach (dyspepsia) and pain. The good news is that stopping smoking will have an immediate effect on these symptoms.[8]
- Ask your doctor to recommend smoking cessation programs. You might join a support group or take medication to help you cut back on smoking.[9]
-
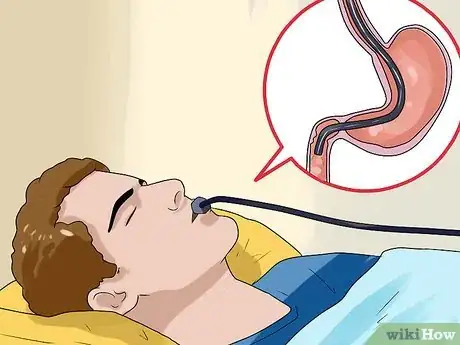
6Have an endoscopic procedure if the ulcer is more severe. If medications don't help your ulcer pain, your doctor may run a small tube from your mouth down into your stomach. There's a small camera on the end of the scope, and the doctor can also use it to administer medications or to clip or cauterize the ulcer.[10]
-
7Monitor your recovery. You should feel relief within two to four weeks after starting treatment, although it may take longer if you smoke. If you're not feeling better after four weeks, talk with your doctor. You may have an underlying condition or a refractory ulcer.
- Be aware that many medications will need to be taken long-term. This is why it's important to watch for side effects and talk with your doctor if you have concerns.[11]
Recognizing and Diagnosing Ulcers
-
1Pay attention to pain. Although symptoms of stomach ulcers can vary from person to person, pain is a common symptom. You may have pain in the area just below your rib cage near the center of your chest. In fact, you might notice pain anywhere from your belly button up towards your breastbone.[12]
- Don't be surprised if the pain comes and goes. It might be worse at night, if you're hungry, or it may go away and return weeks later.
-
2Look for ulcer damage. In addition to pain, you may experience nausea, vomiting, or bloating.[13] These can be caused by damaged stomach walls where the ulcer has formed. Then, when your stomach secretes acid it needs to digest food, the acid irritates and damages the ulcer even more.
- In severe cases, you may vomit blood or notice blood in your stools.[14]
-
3Know when to see a doctor. You should be able to spot "red flags" or warning signs of an ulcer.[15] If you have any of these symptoms along with stomach pain, call your physician or 911 right away:
- Fever
- Severe pain
- Diarrhea that lasts longer than two to three days
- Persistent constipation (longer than two to three days)
- Blood in the stools (which can appear red, black, or tarry)
- Persistent nausea or vomiting
- Vomiting blood or material that looks like coffee grounds
- Severe tenderness of the belly
- Jaundice (yellowish discoloration of the skin and the whites of the eyes)
- Swelling or visible bloating of the abdomen
-
4Get a diagnosis. Your doctor will probably want an EGD (EsophagoGastroDuodenoscopy). During this procedure, a small camera on a flexible tube is inserted into your stomach. This way, doctors can visualize the ulcers on your stomach and determine if any are bleeding.[16]
- X-rays of the upper gastrointestinal tract can also diagnose gastric ulcers, although these aren't as widely used since they can miss small ulcers.
- After your initial treatment, your doctor may wish to perform an endoscopy, a procedure during which your doctor will use a tube with a tiny camera and light to examine your digestive tract. This way your doctor can ensure that the ulcer responded to treatment and was not actually a symptom of stomach cancer.[17]
Managing Gastric Ulcer Pain
-
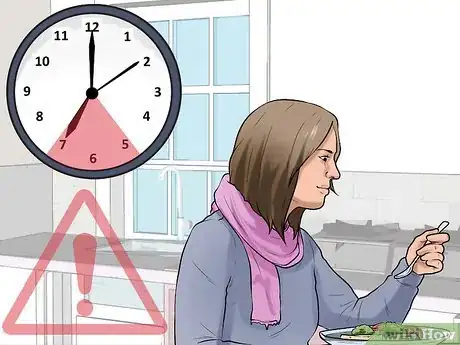
1Reduce pressure on your stomach. Since your stomach is already under great stress, avoid putting extra physical pressure on your stomach. You can wear clothing that doesn't constrict your stomach or abdomen. And, you might get relief by eating smaller, more frequent meals instead of a few large meals.[18] This reduces the amount of acid in your stomach and keeps the pressure off your stomach.
- Try not to eat within two to three hours before going to bed. This will keep food from putting pressure on your stomach while you sleep.
-
2Consult with your doctor. There a number of herbal approaches you can try to treat ulcer pain.[19] Talk to your physician before trying herbal or home remedies. In general, they're all very safe, but you should make sure that none of the herbs will interact with any medications you're taking.
- Since some remedies haven't been tested for use by pregnant women, it's important to talk with your doctor about using them if you're pregnant or nursing.
-
3Eat a low-acid diet. Acidic foods can irritate your ulcer, making the pain worse. In addition, avoid greasy or fried foods, and don't drink alcohol.[20]
-
4Drink aloe vera juice. Research shows that aloe vera can help heal gastric ulcers.[21] Aloe juice decreases inflammation and acts to neutralize the stomach acid, reducing pain. To use it, drink 1/2 cup of organic aloe vera juice. You can sip this throughout the day. But, since aloe vera can act as a laxative, limit your drinking to a total of 1 to 2 cups a day.
- Make sure to buy aloe vera juice that contains a high level of aloe vera juice. Avoid juices that contain a lot of added sugars or fruit juices.
-
5Drink an herbal tea. Ginger and chamomile make great anti-inflammatory teas which can soothe an irritated stomach and reduce nausea and vomiting.[22] Fennel helps settle the stomach and decreases the acid levels.[23] Mustard also acts as an anti-inflammatory and as an acid neutralizer. To prepare:
- Ginger tea: steep packaged tea bags. Or, cut up 1 teaspoon of fresh ginger and steep it in boiled water for 5 minutes. Drink ginger tea throughout the day, especially 20 to 30 minutes before meals.
- Fennel tea: crush about a teaspoon of fennel seeds and steep them in a cup of boiled water for five minutes. Add honey to taste and drink 2 to 3 cups a day about 20 minutes before meals.
- Mustard tea: dissolve powdered or good prepared mustard in hot water. Or, you can take 1 teaspoon of mustard by mouth.
- Chamomile tea: steep packaged tea bags. You can also steep 3 to 4 tablespoons (44.4 to 59.1 ml) of chamomile in 1 cup of boiled water for five minutes.[24]
-
6Take licorice root. Licorice root (deglycyrrhizinated licorice root) is commonly used to treat peptic ulcers, canker sores, and reflux.[25] Take the licorice root (which comes in chewable tablets) according to the manufacturer's instructions. You'll probably need to take two to three tablets every four to six hours. The taste might take some time to get used to, but licorice root can heal your stomach, control hyperacidity and relieve pain.[26]
- You can also take slippery elm as a chewable tablet or drink (3 to 4 ounces). Slippery elm coats and soothes irritated tissues. It's also safe to use during pregnancy.[27]
Expert Q&A
Did you know you can get expert answers for this article?
Unlock expert answers by supporting wikiHow
-
QuestionWhich medicine is best for gastric ulcer?
 Roy Nattiv, MDDr. Roy Nattiv is a Board-Certified Pediatric Gastroenterologist in Los Angeles, California. With over 20 years of experience he specializes in a broad range of pediatric gastrointestinal and nutritional illnesses such as constipation, diarrhea, reflux, food allergies, poor weight gain, SIBO, IBD, and IBS. He completed his pediatric residency at the Children’s Hospital at Montefiore, Albert Einstein College of Medicine in New York, and his fellowship at the University of California, San Francisco (UCSF). While at UCSF, he was a California Institute of Regenerative Medicine (CIRM) fellowship trainee and was awarded the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition (NASPGHAN) Fellow to Faculty Award in Pediatric IBD Research. Dr. Nattiv received his undergrad degree from the University of California, Berkeley, and his medical degree (MD) from the Sackler School of Medicine in Tel Aviv, Israel.
Roy Nattiv, MDDr. Roy Nattiv is a Board-Certified Pediatric Gastroenterologist in Los Angeles, California. With over 20 years of experience he specializes in a broad range of pediatric gastrointestinal and nutritional illnesses such as constipation, diarrhea, reflux, food allergies, poor weight gain, SIBO, IBD, and IBS. He completed his pediatric residency at the Children’s Hospital at Montefiore, Albert Einstein College of Medicine in New York, and his fellowship at the University of California, San Francisco (UCSF). While at UCSF, he was a California Institute of Regenerative Medicine (CIRM) fellowship trainee and was awarded the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition (NASPGHAN) Fellow to Faculty Award in Pediatric IBD Research. Dr. Nattiv received his undergrad degree from the University of California, Berkeley, and his medical degree (MD) from the Sackler School of Medicine in Tel Aviv, Israel.
Board Certified Gastroenterologist Gastric ulcers are typically treated with strong antacids to decrease the production of acid in the stomach. They're also sometimes treated topically with something called carafate (sucralfate), which will act to coat the acid from within, allowing the stomach to regenerate and heal itself from the outside in. If the ulcer is caused by an H. pylori infection, that should also be treated with antibiotics.
Gastric ulcers are typically treated with strong antacids to decrease the production of acid in the stomach. They're also sometimes treated topically with something called carafate (sucralfate), which will act to coat the acid from within, allowing the stomach to regenerate and heal itself from the outside in. If the ulcer is caused by an H. pylori infection, that should also be treated with antibiotics.
References
- ↑ Roy Nattiv, MD. Board Certified Gastroenterologist. Expert Interview. 18 December 2020.
- ↑ https://www.nhs.uk/conditions/stomach-ulcer/treatment/
- ↑ http://www.mayoclinic.org/diseases-conditions/peptic-ulcer/basics/treatment/con-20028643
- ↑ Roy Nattiv, MD. Board Certified Gastroenterologist. Expert Interview. 18 December 2020.
- ↑ https://www.niddk.nih.gov/health-information/digestive-diseases/peptic-ulcers-stomach-ulcers/treatment
- ↑ https://www.niddk.nih.gov/health-information/digestive-diseases/peptic-ulcers-stomach-ulcers/treatment
- ↑ Roy Nattiv, MD. Board Certified Gastroenterologist. Expert Interview. 18 December 2020.
- ↑ https://www.hopkinsmedicine.org/health/conditions-and-diseases/smoking-and-the-digestive-system
- ↑ http://www.lung.org/stop-smoking/i-want-to-quit/how-to-quit-smoking.html
- ↑ Roy Nattiv, MD. Board Certified Gastroenterologist. Expert Interview. 18 December 2020.
- ↑ https://www.nhs.uk/conditions/stomach-ulcer/treatment/
- ↑ https://familydoctor.org/condition/ulcers/
- ↑ https://my.clevelandclinic.org/health/diseases/10350-peptic-ulcer-disease
- ↑ http://patients.gi.org/topics/peptic-ulcer-disease/
- ↑ https://www.nhs.uk/conditions/stomach-ulcer/
- ↑ https://gi.org/topics/peptic-ulcer-disease/
- ↑ http://www.asge.org/uploadedFiles/Publications_and_Products/Practice_Guidelines/The%20role%20of%20endoscopy%20in%20the%20management%20of%20patientswith%20peptic%20ulcer%20disease.pdf
- ↑ https://patient.info/digestive-health/dyspepsia-indigestion/stomach-ulcer-gastric-ulcer
- ↑ Pizzorno, JE., Murray, MT., Joiner-Bey, H. The Clinician’s Handbook of Natural Medicine, pg.392-397, 2002.
- ↑ Roy Nattiv, MD. Board Certified Gastroenterologist. Expert Interview. 18 December 2020.
- ↑ http://www.ncbi.nlm.nih.gov/pubmed/16610053
- ↑ https://health.clevelandclinic.org/ginger-ale-and-saltine-crackers-5-ways-to-ease-stomach-pain-and-nausea/
- ↑ Pizzorno, JE., Murray, MT., Joiner-Bey, H. The Clinician’s Handbook of Natural Medicine, pg.392-397, 2002.
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2995283/
- ↑ https://www.stlukes-stl.com/health-content/medicine/33/000262.htm
- ↑ Glick, L., Deglycyrrhizinated liquorice for peptic ulcer. Lancet. 1982 Oct 9;2(8302):817
- ↑ Pizzorno, JE., Murray, MT., Joiner-Bey, H. The Clinician’s Handbook of Natural Medicine, pg.392-397, 2002.



































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...