This article was co-authored by Rajesh Khanna, MD and by wikiHow staff writer, Christopher M. Osborne, PhD. Dr. Rajesh Khanna is a board certified Ophthalmologist and the Founder of Khanna Vision Institute in Los Angeles, California. Dr. Khanna specializes in Lasik, cataract, and refractive eye surgery as well as treatments for presbyopia and keratoconus. Dr. Khanna completed his first Ophthalmology Residency in Mumbai and his second Ophthalmology Residency at SUNY Downstate in New York City. He went on to complete a fellowship training in corneal and refractive surgery from the University of Cincinnati in Ohio and a Neurophthalmology fellowship from Kingsbrook Jewish Hospital in New York City. Dr. Khanna is also a voluntary member of the UCLA faculty and is an Internationally recognized top Lasik, presbyopic implants in the eye (PIE), and Refractive vision care specialist. He is board certified by the American Board of Ophthalmology and is a certified Master of Surgery by the University of Bombay.
There are 14 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 14,354 times.
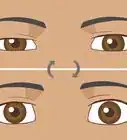
In simple terms, binocular vision refers to your brain’s ability to accept individual signals from each of your eyes and combine them into a single signal. Poor binocular vision results in poor depth perception and can also cause symptoms like headaches and blurred vision. Fortunately, your binocular vision can often be improved through a combination of treatments, especially vision therapy exercises. For the best results, start with a visit to your eye doctor—then get to work improving your binocular vision!
Steps
Symptoms and Diagnosis
-
1Watch out for symptoms like eye pain, double vision, and headaches. Ideally, your brain combines signals from both eyes, filters out conflicting signals, and creates a single, binocular signal.[1] Poor binocular vision usually occurs when signals from one eye aren’t being produced or sent effectively. If you have poor binocular vision, you may experience symptoms like the following:[2]
- Headaches.
- Eye strain.
- Eye pain.
- Blurred vision.
- Double vision.
- Poor depth perception.
-
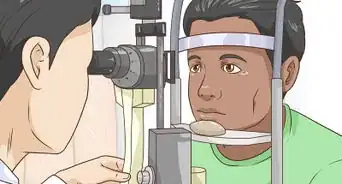
2Undergo a complete eye exam by a trained professional. Make an appointment with your eye doctor and tell them about your symptoms. They’ll check for binocular vision problems by doing tests that are generally similar to a typical eye exam—things like having you cover one eye, following their finger, and so on. Be honest and accurate about what you’re seeing—or not seeing![3]
- Binocular vision problems are fairly common, especially among children but also in adults, so eye doctors are typically well-prepared to recognize them.
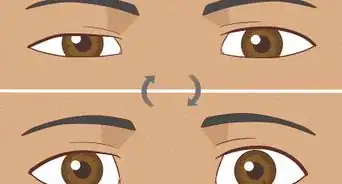
- Convergence insufficiency (CI) is one of the more common binocular vision problems. If you have CI, one of your eyes will tend to turn outward when you try to focus on near objects.[4]
Advertisement -
3Talk to your eye doctor about potential causes of your condition. Binocular vision troubles are often genetic or simply have no known cause. That said, injury, illness, and medication, among other factors, can also contribute. Particularly if you have CI, for example, the following are potential contributing factors:[5]
- You’ve suffered a concussion.
- You’ve been diagnosed with ADHD.
- You have Lyme disease.
- You take an SSRI antidepressant medication like Zoloft, Paxil, or Prozac.
- You take a stimulant medication (such as methylphenidate, dexmethylphendate, or dextroamphetamine) that lists blurred vision as a possible side effect.
At-Home Exercises
-
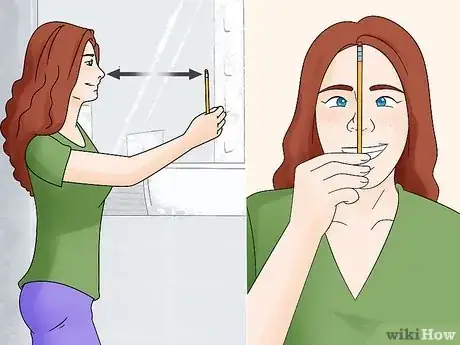
1Do pencil push-ups several times per day. To begin a pencil push-up, hold a pencil at arm’s length—or at least 20 in (51 cm) away—in line with the tip of your nose. Focus your eyes on the pencil. Slowly draw the pencil straight in toward the tip of your nose. Maintain your eye focus. Stop when you see double (2 pencils), then maintain eye focus as you slowly return the pencil to the starting point.[6]
- Repeat the process for up to 5 minutes, up to 3 times per day, or as directed by your eye doctor. Do not exceed these recommendations unless your eye doctor specifically prescribes it.
- As an alternative, your eye doctor may recommend that you bring the pencil all the way to your nose before returning to the starting point.
-
2Use doctor-recommended vision therapy computer programs at home. While pencil push-ups have been the low-tech vision therapy option for decades, computer-based exercises have become increasingly popular. These are often set up as games or challenges that require you to adjust your eye focus regularly—you may even have fun doing them! Your eye doctor may recommend at-home computer programs alone, or in combination with in-office programs.[7]
- While vision therapy programs are widely available online, consult your eye doctor before trying them. For one thing, not all vision therapy programs are created equal—some are better designed and more effective than others. Also, like with pencil push-ups, it’s important not to over-do it with computer programs. Follow the treatment schedule recommended by your eye doctor.
-
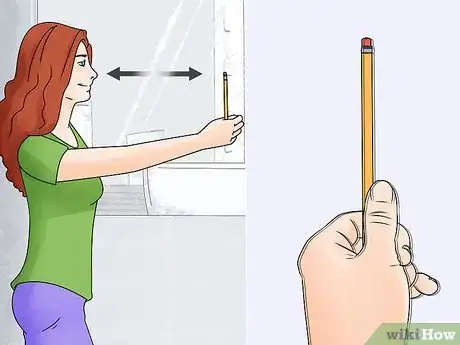
3Do jump convergence exercises for diagnosed CI. To begin this at-home exercise for convergence insufficiency (CI), hold a pencil at arm’s length. Instead of looking at the pencil, though, focus on a stationary object—such as a poster on the wall or a houseplant—that’s in your line of sight and about 10–13 ft (3.0–4.0 m) away. Quickly shift your gaze to the pencil, working to focus your eyes if you see double. Once you see a single pencil, shift your focus back to the distant object. Bring the pencil in a few inches/centimeters closer and repeat the process. Keep bringing the pencil in until you can no longer avoid seeing double.[8]
- As with pencil push-ups, don’t do this for more than 5 minutes at a time and 15 minutes total each day.
- If you haven’t been diagnosed with CI, ask your eye doctor whether this exercise may be helpful for you.
-
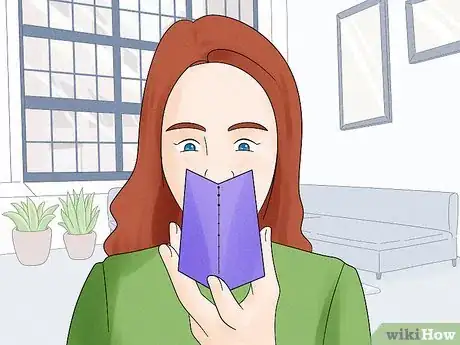
4Use dot cards provided by your eye doctor as another CI exercise. Hold the rectangular card to your nose so that the line of dots on it extends away from your nose; angle the card down a bit if doing so helps you see the dots better. Focus your eyes on the dot farthest away from you, working to turn your eyes inward so you don’t see double. Once the dot is in focus, hold your gaze for 10 seconds, then move on to the dot that’s next in line. Repeat the process with each dot on the card.[9]
- Do this exercise once per day, or as directed by your eye doctor.
- If you can’t focus on one of the dots, backtrack to the previous dot, focus on it for 10 seconds, then try again. If you’re unable to focus on the farthest dot, let your eye doctor know.
- This exercise may not be recommended by your eye doctor if you don’t have a CI diagnosis. Have a chat with them first.
-
5Follow the 20/20/20 rule to rest your eyes during screen time. Taking frequent “eye breaks” may be particularly helpful if your binocular vision suffers after staring at a screen for long periods.[10] Many eye professionals promote the “20/20/20 rule:” after every 20 minutes of screen time, you should take a 20 (or longer) second break and focus your eyes on an object that’s approximately 20 ft (6.1 m) away.[11]
- If you get headaches or blurred vision when looking at a screen for long periods, this easy treatment may prove very helpful!
In-Office Therapy
-
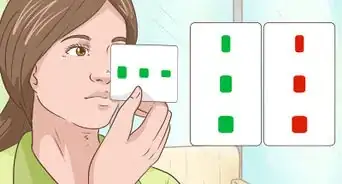
1Use “push-pull” treatments with red and green glasses. During a common form of push-pull exercise, your eye doctor will have you put on special glasses that have a red lens and a green lens. You’ll be shown a series of images with varying contrast levels which, in combination with the lenses, force your brain to more readily accept signals from your less effective eye. It ends up being more like a game than an exercise![12]
- Exercises like these are called “push-pull” because they both increase perceptive stimulus to your less effective eye (“push”) and suppress stimulus to your more effective eye (“pull”).[13]
-
2Try MFBF therapy to utilize only your less effective eye. Monocular fixation in a binocular field (MFBF) therapy uses special glasses with one red-tinted lens over your more effective eye, while your other eye remains unobstructed. Your eye doctor will give you writing activities to complete using a red pencil or pen, which means that you’ll only be able to see what you’re doing with your less effective (no red lens) eye.[14]
- MFBF therapy is less of a penalization/suppression therapy than is patching, since your more effective eye isn’t covered, but it provides less of a push-pull effect than do exercises that use both red and green lenses.
- For maximum effectiveness, therapies like MFBF should be done in-office.
-
3Do prism (lens fixation) therapy under your eye doctor’s guidance. Prism (or lens fixation) therapy involves the use of various combinations of lenses while you look at objects placed in close proximity. The types of lenses used will vary based on your condition, but the goal is to use a push-pull effect to help retrain your brain’s signal acceptance.[15]
- In nearly all cases, your eye doctor will use a range of both in-office and at-home vision therapy techniques. These will usually also be combined with a range of other therapies, possibly including patching, atropine drops, and other options.
Additional Treatments
-
1Use corrective eyewear as prescribed. Wearing corrective eyewear can improve your binocular vision in some cases, but it typically does not help cure the underlying problem. If your eye doctor gives you a prescription, use the eyewear as directed—for instance, wear your prescribed glasses only when reading or looking at close-in objects.[16]
- If you have CI, you may be prescribed glasses that have one prism lens. The prism lens compensates for the outward drift of your less effective eye when you look at close-in objects. It does not, however, help retrain your less effective eye to not drift outward.
-
2Patch your more effective eye for short periods as directed. Patching—covering your more effective eye to strengthen the less effective one—used to be the primary treatment tool for binocular vision issues. While patching still has a treatment role, though, research shows that “penalization” treatments like patching are best used in a limited, supporting role. So, if your eye doctor does recommend patching, follow their treatment instructions carefully.[17]
- You might, for example, be advised to wear a patch for up to 2 hours per day.
- Patching is still widely used for amblyopia (“lazy eye”), a common cause of binocular vision problems in children and some adults. However, even in this case, research indicates that penalization/suppression treatments like patching should be used more sparingly.[18]
- Some research even indicates that penalization/suppression treatments like patching may do more harm than good in some cases,[19] but other experts still believe patching has a role to play in treatment.[20]
-
3Use prescribed atropine drops as an alternative to patching. Patching may be beneficial when used in a limited approach, but compliance is often an issue—many people find an eye patch uncomfortable or don’t like how they look.[21] In this case, atropine drops—which your eye doctor uses to dilate your pupils during an exam—may be prescribed as an alternative. By dilating your pupil and blurring the vision in your more effective eye, atropine temporarily forces your brain to more readily accept signals from your less effective eye.[22]
- Prescription atropine often comes in single-dose, mini squeeze bottles. Wash your hands and carefully squeeze the medication into your more effective eye. Follow the dosing schedule prescribed by your eye doctor.
- Like patching, atropine is a penalization/suppression therapy. This means it should typically be used only as a supporting treatment.
-
4Undergo corrective surgery for conditions such as strabismus. Surgery may be the best option if your binocular vision is impaired due to strabismus—a permanent misalignment of your eyes. During strabismus surgery, specific eye muscles will be tightened, loosened, or relocated so that your eyes align properly. While eye surgery sounds scary, this is usually an outpatient procedure with a recovery time of only a few days.[23]
- Surgery isn’t the best option for all types of binocular vision troubles, so talk to your eye doctor about whether surgery may be a good idea for you.
- In some cases, instead of surgery, your eye surgeon may instead inject one or more of your eye muscles with botulinum toxin (Botox) in order to paralyze them. This procedure may produce permanent results or need to be repeated every few months.
Warnings
- While vision therapy can really help to improve your binocular vision, remember not to overdo it! Even if you’re only doing simple at-home exercises like pencil push-ups, your best bet is always to consult your eye doctor first.⧼thumbs_response⧽
References
- ↑ https://pubmed.ncbi.nlm.nih.gov/30372739/
- ↑ https://opto.ca/health-library/binocular-vision
- ↑ https://www.reviewofoptometry.com/article/binocular-vision-problems
- ↑ https://aapos.org/glossary/convergence-insufficiency
- ↑ https://www.reviewofoptometry.com/article/binocular-vision-problems
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4302485/
- ↑ https://www.reviewofoptometry.com/article/binocular-vision-problems
- ↑ https://www.wwl.nhs.uk/Library/All_New_PI_Docs/Ophthalmology/Orth%20013%20Home%20Exercise%20for%20improving%20Convergence%20Insufficiency%2011.21%20v5.pdf
- ↑ https://www.wwl.nhs.uk/Library/All_New_PI_Docs/Ophthalmology/Orth%20013%20Home%20Exercise%20for%20improving%20Convergence%20Insufficiency%2011.21%20v5.pdf
- ↑ Rajesh Khanna, MD. Board Certified Ophthalmologist. Expert Interview. 11 November 2020.
- ↑ https://www.myopiainstitute.com/eye-care/4-vision-therapy-devices-and-exercises-to-improve-eyesight/
- ↑ https://www.reviewofoptometry.com/article/binocular-vision-problems
- ↑ https://grantome.com/grant/NIH/R01-EY023374-03
- ↑ https://www.reviewofoptometry.com/article/binocular-vision-problems
- ↑ https://www.myopiainstitute.com/eye-care/4-vision-therapy-devices-and-exercises-to-improve-eyesight/
- ↑ https://aapos.org/glossary/convergence-insufficiency
- ↑ https://www.reviewofoptometry.com/article/binocular-vision-problems
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4723179/
- ↑ https://jov.arvojournals.org/article.aspx?articleid=2213212
- ↑ https://www.myopiainstitute.com/eye-care/4-vision-therapy-devices-and-exercises-to-improve-eyesight/
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1172103/
- ↑ https://www.gosh.nhs.uk/conditions-and-treatments/procedures-and-treatments/treating-amblyopia-lazy-eye-atropine-drops
- ↑ https://www.aao.org/eye-health/diseases/strabismus-treatment



























































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...