This article was co-authored by Mark Co, DPM. Dr. Mark Co is a Podiatrist who runs his own private practice in San Francisco, California. Dr. Co specializes in treatments for bunions, ingrown toenails, toenail fungus, warts, plantar fasciitis and other causes of foot pain. He also offers custom orthotics for the treatment and prevention of foot and ankle issues. Dr. Co completed a Master of Business Administration (MBA) at New York University and an MA in Electrical Engineering and Computer Science at Johns Hopkins University. Dr. Co also completed his DPM at the California School of Podiatric Medicine and a residency and internship at the Kaiser Permanente Medical Center, Santa Clara, California. Dr. Co was awarded San Francisco's "Top 3 Podiatrists" in 2018, 2019, and 2020. Dr. Co is also a member of the CPMA (American Podiatric Medical Association).
There are 10 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 116,702 times.
Athlete’s foot, also known as tinea pedis, is a common fungal infection — especially among athletes or people who shower often in bare feet.[1] Direct exposure to fungus or mold while bathing (particularly in high risk places such as public swimming pools or gyms) leads to most cases of athlete's foot, but excessive foot sweating combined with poor hygiene are risk factors also. Athlete’s foot initially affects the sole of the foot, in between the toes, but it can spread to various parts of the body if not recognized and appropriately treated.
Steps
Recognizing the Common Symptoms
-
1Look between your 3rd, 4th, and 5th toes. These are the most susceptible areas of your foot for fungal infection due to three main factors: they are often neglected when drying the feet; the spaces between toes don't evaporate sweat or moisture very well; they are most prone to abrasion from poorly fitting shoes.[2] If you're itchy in that part of your foot and see some redness, then you might be dealing with a fungal infection.
- The primary signs and symptoms of athlete's foot include: a scaly, itchy rash that sometimes leads to stinging or burning pain.
- In advanced cases, inflammation and peeling of the skin occur between the toes — a process called maceration.
- Athlete's foot is contagious and is easily spread via contaminated floors, towels, socks or flip-flops.
-
2Look for dry, flaky skin on the bottoms and sides of your feet. As athlete's foot worsens it spreads over the sole of the foot, where it causes dry, flaky skin.[3] It will feel rough to the touch and likely be itchy and somewhat irritated. Initially the area will be small, but it will spread and form an irregular margin.
- There are three main varieties of tinea pedis: moccasin type (involves the sole of the feet), inter-digital type (involves the clefts between the toes) and the blistering type (involves the formation of blisters).[4]
- Athlete's foot is sometimes called "jungle rot" by members of the armed forces who serve in humid tropical climates.
Advertisement -
3Be suspicious if you feel itching and burning pain. Foot pain, particularly aches and cramps, are common and usually the result of overuse or ill-fitting shoes, but burning pain accompanied by severe, non-stop itching should make you consider athlete's foot. Fungi cause burning and itching because they burrow into the tissue of the foot and use superficial layers as food. As a result, nerve endings become irritated, which provokes itching and leads to burning pain.
- Itching is often most intense right after you take off your shoes and socks.[5]
- Athlete's foot is caused by the same type of fungi that leads to ringworm and jock itch.
-
4Distinguish between types of blisters. A foot blister can easily be caused by too much walking or running, especially if your shoes don't fit well, but blisters caused by athlete's foot are different — they tend to ooze pus and other fluid and get crusty.[6] Blisters usually form on the thick skin patches, which increases the risk of bacterial infection.
- After the fungal blisters erupt, lesions with a red, scaly border grow outward and leave a clear center — this is the classic ringworm appearance found over the skin.
- You're at higher risk of athlete's foot if you are male, frequently wear damp socks or tight-fitting shoes, walk barefoot in public areas and/or have weakened immunity.[7]
-
5Pay attention to toenail changes. The fungus of athlete's foot often spreads to infect the toenails, which then become discolored, thick and even crumbly.[8] In advanced (chronic) stages of infection, toenails become brittle and may even fall off — a condition known as onycholysis.
- Fungus is difficult to eradicate from nail beds because it burrows deep into the tissue.
- Burning foot pain and toenail changes are also common with diabetes, so make sure your blood sugar levels are within the normal range.
Confirming Athlete's Foot
-
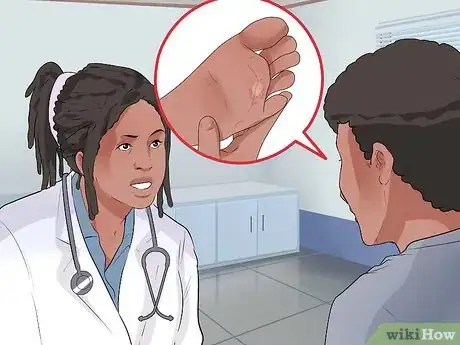
1See your family doctor. There's no point in guessing about your foot ailment, so make an appointment with your physician and tell him/her your observations and suspicions. In some cases, your doctor may be able to diagnose a fungal infection simply by looking at your foot. However, to confirm the diagnosis (and rule out other conditions), he/she might take a skin sample, add a few drops of potassium hydroxide (KOH) solution and look at it under a microscope. The KOH dissolves skin, but leaves budding fungi intact, making it easy to see.[9]
- Alternatively, your doctor may view your feet under black light from a Wood's light, which highlights the presence of fungal infections.[10]
- Your doctor may also do a gram stain to see if there is an underlying bacterial infection.[11]
- Your doctor may also take a blood test in order to rule out diabetes and other types of infections (bacterial and viral).
-
2Get a referral to a medical specialist. Medical specialists who deal with skin problems are called dermatologists. A dermatologist is likely to have much more experience than your family physician in dealing with skin conditions, such as infections, rashes and other afflictions. A dermatologist is more likely to be able to do a skin biopsy and KOH preparation under a microscope in their office, so the results can be available in a matter of minutes instead of hours or days.[12]
- If there is no sign of fungus, then the dermatologist needs to consider other skin conditions that cause a similar appearance such as psoriasis, contact dermatitis, eczema, bacterial infections, gout and venous insufficiency.
- Psoriasis can be distinguished by its characteristic silvery white scales, which are usually found in the folds of joints.
-
3See a podiatrist. A podiatrist is a foot specialist who also can confirm a diagnosis of athlete's foot and provide treatment. A podiatrist is also a great source of information on what kinds of shoes and socks to wear to prevent fungal infections from reoccurring.
- Occlusive shoe materials, such as vinyl, rubber and plastic, don't allow for sufficient ventilation, which cause feet to remain warm and moist — providing an excellent opportunity for the fungus to proliferate.[13] Switch to shoes with leather insoles instead.
- Use cotton socks that absorb water from your feet. Try to avoid socks made with nylon or other synthetic materials.
- Try to change your socks every day. Wash them in hot water with baking soda to kill any fungus.
Combating Athlete's Foot
-
1Use an over-the-counter anti-fungal preparation. Over-the-counter anti-fungal powders, creams and/or ointments can help rid you of athlete's foot.[14] The topical drugs that are effective against tinea pedis include azoles, allylamines, ciclopirox, tolnaftate, and amorolfine.[15] Keep using the medicine for a couple of weeks after the infection has cleared to prevent its return, as there may be spores buried in the skin.
- Use the powder to disinfect your shoes and save the cream / ointment for your feet, applying it early in the morning and at bedtime.
- Fungicidal and fungistatic chemicals used for athlete's foot frequently fail to kill the fungi in the deeper horny layers of the skin, which explains why they're sometimes ineffective.
-
2Try some home remedies. Instead of buying creams from the pharmacy, look in your cupboards for white vinegar (acetic acid). Diluted vinegar (with 75% water) is strong enough to inhibit fungal growth.[16] Soak your feet in diluted vinegar for 10-15 minutes, twice daily, until the itchiness and dryness disappear.
- Alternatively, soaking your feet in a drying solution of aluminum acetate (Burow's solution or Domeboro solution) can be effective also.
- Clorox bleach can also be effective for killing fungi and most other pathogens, but it may temporarily irritate your skin and nerve endings. Furthermore, try not to inhale it directly as it may cause dizziness, headache or confusion.
- Consider an aluminum salt solution, such as aluminum chloride 10% solution or aluminium acetate. These act as antiperspirants by blocking sweat glands. The usual ratio is 1 part solution mixed with 20 parts water (unless a physician instructs otherwise). The solution should be applied to your feet overnight.
-
3Get a prescription for an anti-fungal drug. More advanced or resistant cases of athlete's foot may need an oral (pill) anti-fungal such as terbinafine (Lamisil), itraconazole (Sporanox) or fluconazole (Diflucan). Potent oral medications are reserved for people who don't respond to powders, creams, sprays or ointments. Pills may need to be taken for up to a month or so.[17]
- Blood tests may be needed before you take these medications to make sure your liver can tolerate them.
- Treatment for nail fungus may be more intensive and require longer courses (three to four months) of oral medications.
- Fluconazole 50 mg once daily for 4-6 weeks is adequate to clear most fungal infections.
- Itraconazole 100 mg once daily for 15 days may be a better alternative.
Expert Q&A
-
QuestionWhen should I go to the doctor for athlete's foot?
 Mark Co, DPMDr. Mark Co is a Podiatrist who runs his own private practice in San Francisco, California. Dr. Co specializes in treatments for bunions, ingrown toenails, toenail fungus, warts, plantar fasciitis and other causes of foot pain. He also offers custom orthotics for the treatment and prevention of foot and ankle issues. Dr. Co completed a Master of Business Administration (MBA) at New York University and an MA in Electrical Engineering and Computer Science at Johns Hopkins University. Dr. Co also completed his DPM at the California School of Podiatric Medicine and a residency and internship at the Kaiser Permanente Medical Center, Santa Clara, California. Dr. Co was awarded San Francisco's "Top 3 Podiatrists" in 2018, 2019, and 2020. Dr. Co is also a member of the CPMA (American Podiatric Medical Association).
Mark Co, DPMDr. Mark Co is a Podiatrist who runs his own private practice in San Francisco, California. Dr. Co specializes in treatments for bunions, ingrown toenails, toenail fungus, warts, plantar fasciitis and other causes of foot pain. He also offers custom orthotics for the treatment and prevention of foot and ankle issues. Dr. Co completed a Master of Business Administration (MBA) at New York University and an MA in Electrical Engineering and Computer Science at Johns Hopkins University. Dr. Co also completed his DPM at the California School of Podiatric Medicine and a residency and internship at the Kaiser Permanente Medical Center, Santa Clara, California. Dr. Co was awarded San Francisco's "Top 3 Podiatrists" in 2018, 2019, and 2020. Dr. Co is also a member of the CPMA (American Podiatric Medical Association).
Podiatrist You can usually treat athlete's foot with an over-the-counter antifungal cream. If the athlete's foot doesn't start to disappear in a day or two or it's a particularly severe case, you may need to see your doctor to get a prescription-strength antifungal cream. You may also need to see a doctor if your skin becomes infected and the athlete's foot gets under the nails.
You can usually treat athlete's foot with an over-the-counter antifungal cream. If the athlete's foot doesn't start to disappear in a day or two or it's a particularly severe case, you may need to see your doctor to get a prescription-strength antifungal cream. You may also need to see a doctor if your skin becomes infected and the athlete's foot gets under the nails. -
QuestionHow do I stop itching my foot when I'm trying to sleep?
 Chris M. Matsko, MDDr. Chris M. Matsko is a retired physician based in Pittsburgh, Pennsylvania. With over 25 years of medical research experience, Dr. Matsko was awarded the Pittsburgh Cornell University Leadership Award for Excellence. He holds a BS in Nutritional Science from Cornell University and an MD from the Temple University School of Medicine in 2007. Dr. Matsko earned a Research Writing Certification from the American Medical Writers Association (AMWA) in 2016 and a Medical Writing & Editing Certification from the University of Chicago in 2017.
Chris M. Matsko, MDDr. Chris M. Matsko is a retired physician based in Pittsburgh, Pennsylvania. With over 25 years of medical research experience, Dr. Matsko was awarded the Pittsburgh Cornell University Leadership Award for Excellence. He holds a BS in Nutritional Science from Cornell University and an MD from the Temple University School of Medicine in 2007. Dr. Matsko earned a Research Writing Certification from the American Medical Writers Association (AMWA) in 2016 and a Medical Writing & Editing Certification from the University of Chicago in 2017.
Family Medicine Physician You need to use an antifungal ointment, powder, or cream to cure athletes foot.
You need to use an antifungal ointment, powder, or cream to cure athletes foot. -
QuestionI have red spots on my hands that seem to get worse when I touch my feet, which have the same spots. The doctor says it's eczema, and cream seems to help my hands until I touch my feet to apply the cream there. No pain or itching. What should I do?
 Chris M. Matsko, MDDr. Chris M. Matsko is a retired physician based in Pittsburgh, Pennsylvania. With over 25 years of medical research experience, Dr. Matsko was awarded the Pittsburgh Cornell University Leadership Award for Excellence. He holds a BS in Nutritional Science from Cornell University and an MD from the Temple University School of Medicine in 2007. Dr. Matsko earned a Research Writing Certification from the American Medical Writers Association (AMWA) in 2016 and a Medical Writing & Editing Certification from the University of Chicago in 2017.
Chris M. Matsko, MDDr. Chris M. Matsko is a retired physician based in Pittsburgh, Pennsylvania. With over 25 years of medical research experience, Dr. Matsko was awarded the Pittsburgh Cornell University Leadership Award for Excellence. He holds a BS in Nutritional Science from Cornell University and an MD from the Temple University School of Medicine in 2007. Dr. Matsko earned a Research Writing Certification from the American Medical Writers Association (AMWA) in 2016 and a Medical Writing & Editing Certification from the University of Chicago in 2017.
Family Medicine Physician If you have eczema, use eucerin cream to counterbalance the dry skin. If you have an infection, ask your doctor about mupirocin.
If you have eczema, use eucerin cream to counterbalance the dry skin. If you have an infection, ask your doctor about mupirocin.
Warnings
- If your foot is swollen and warm to the touch with red streaks (particularly if you have a fever), then see a doctor immediately because you likely have a bacterial infection.⧼thumbs_response⧽
- Athlete's foot is contagious. Avoid touching other people with areas of your skin that are showing symptoms.⧼thumbs_response⧽
References
- ↑ http://www.mayoclinic.org/diseases-conditions/athletes-foot/basics/definition/con-20014892
- ↑ http://www.netdoctor.co.uk/diseases/facts/athletesfoot.htm
- ↑ Mark Co, DPM. Podiatrist. Expert Interview. 21 April 2020.
- ↑ http://www.medicinenet.com/athletes_foot/page3.htm
- ↑ https://www.mayoclinic.org/diseases-conditions/athletes-foot/symptoms-causes/syc-20353841
- ↑ http://www.nlm.nih.gov/medlineplus/ency/article/000875.htm
- ↑ https://www.mayoclinic.org/diseases-conditions/athletes-foot/symptoms-causes/syc-20353841
- ↑ http://www.nlm.nih.gov/medlineplus/ency/article/000875.htm
- ↑ http://www.nlm.nih.gov/medlineplus/ency/article/000875.htm
- ↑ http://www.mayoclinic.org/diseases-conditions/athletes-foot/basics/tests-diagnosis/con-20014892
- ↑ https://www.niaid.nih.gov/topics/antimicrobialresistance/examples/gramnegative/Pages/default.aspx
- ↑ http://www.medicinenet.com/athletes_foot/page4.htm
- ↑ http://www.medicinenet.com/athletes_foot/page5.htm
- ↑ Mark Co, DPM. Podiatrist. Expert Interview. 21 April 2020.
- ↑ http://www.nlm.nih.gov/medlineplus/ency/article/000875.htm
- ↑ http://www.medicinenet.com/athletes_foot/page5.htm
- ↑ Mark Co, DPM. Podiatrist. Expert Interview. 21 April 2020.
About This Article
To know if you have athlete’s foot, check between your toes for a scaly, itchy rash or inflammation. Look particularly close at the spaces between the three smaller toes on the outside of your foot as the infection often shows up there because those areas don’t dry as well. You should also look for dry, flaky skin on the bottom or sides of your feet as well as discolored, thick, crumbly, or brittle toenails. If you notice any of these symptoms or have general itchiness or pain in your foot, visit your doctor so they can have a look or take a skin sample. For more help from our Medical co-author, including how to treat athlete’s foot with medication and home remedies, scroll down!





































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...