This article was co-authored by Tu Anh Vu, DMD. Dr. Tu Anh Vu is a board certified dentist who runs her private practice, Tu's Dental, in Brooklyn, New York. Dr. Vu helps adults and kids of all ages get over their anxiety with dental phobia. Dr. Vu has conducted research related to finding the cure for Kaposi Sarcoma cancer and has presented her research at the Hinman Meeting in Memphis. She received her undergraduate degree from Bryn Mawr College and a DMD from the University of Pennsylvania School of Dental Medicine.
This article has been viewed 47,688 times.
Infections occur when harmful bacteria enter your body and begin to multiply, causing pain, swelling, and redness. Any dental work that draws blood can expose you to infection, including teeth cleaning, as it opens a pathway for invading bacteria. Preventing an infection after getting dental work is not hard, though – just practice good oral hygiene, take preventative antibiotics if needed, and watch vigilantly for any of the hallmarks of infection. Also, be sure to talk to your dentist for any post-op instructions that are specific to the procedure you've had done.[1]
Steps
Keeping the Mouth Clean
-
1Brush gently. Depending on what work you’ve had done – like oral surgery or a tooth extraction – you may need to stop brushing for a short time. You should still keep your mouth and teeth clean, however, as food particles and other debris can promote the growth of bacteria. Follow your dentist’s instructions. She may want you to continue brushing gently to keep your mouth clean or stop for a period.[2]
- For tooth extractions, you won’t be able to brush, rinse, spit, or use mouthwash on the day of the surgery or for about 24 hours afterward. Resume brushing thereafter, but avoid the extraction site for about 3 days.
- If you had a tooth extraction, you should not rinse with force. This will create negative pressure that is bad for the blood clot created in the socket.
- Use a soft-bristled toothbrush, as medium- and hard-bristled toothbrushes can wear the enamel away on your teeth, and can lead to receding gums.[3]
-
2Rinse with salt water, alternatively. A salt water rinse is a more gentle way to clean your mouth, though it doesn’t replace brushing. Salt temporarily raises the pH balance in your mouth and creates an alkaline environment hostile to bacteria, slowing their growth. It can therefore ward off infections that might otherwise form in open wounds or sores.[4]
- It’s very easy to make a salt water rinse. All you have to do is add a half teaspoon of salt to one cup of warm water.
- After oral surgery like wisdom tooth extraction, start to rinse your mouth with salt water the next day. Rinse every two hours and after each meal for a total of about five to six times per day. Rinse gently, by moving your tongue from one cheek to the other. Take care not to harm the extraction site. Continue to do this for a week after the surgery.
- Some dentists may ask you to irrigate after a tooth extraction, too. They will give you a small dental irrigator to use starting three days afterward, to flush the tooth socket with warm water after meals and at bedtime. This will clean the site and reduce your chance of infection.
Advertisement -
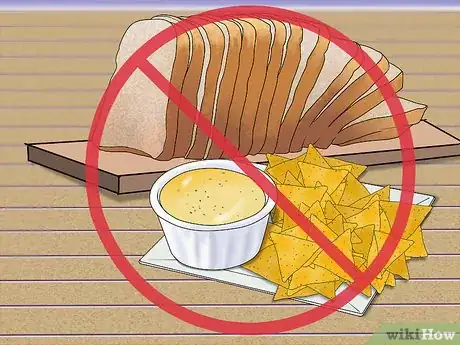
3Avoid foods that can irritate the wound. Infections occur when bacteria enter into your blood stream and multiply. Wounds in your mouth need to close properly and stay closed, then, which means that you’ll need to watch what you eat to avoid reopening incisions, dislodging things like stitches, or irritating the wound. Follow your dentist’s instructions and, if need be, restrict your diet.[5]
- You may need to eat a liquid or semi-soft diet for a few days. Things like applesauce, yogurt, pudding, Jello, eggs, or pancakes are usually OK.
- Avoid tough, crunchy, or hard foods. Things like toast, chips, and fried shrimp could disturb site of your dental work or worse, like opening your stitches and causing bleeding.
Taking Preventative Antibiotics
-
1Talk to your dentist. People with certain medical conditions are at a higher risk for developing dangerous infections after getting dental work and may need preventative or “prophylactic” antibiotics. This is especially true for people who are at risk of an infection of the heart, or endocarditis. They will need antibiotics before the procedure. Talk to your dentist to see whether you fall into this group.[6]
- Endocarditis occurs in the heart valves, especially in the presence of heart defects. Usually, bacteria in the bloodstream don’t stick to the walls of the heart. However, with some abnormalities the blood flows turbulently and allows bacteria to attach themselves and grow.
- Endocarditis is a risk if you have artificial heart valves, shunts or conduits, rheumatic heart disease, or other congenital heart defects. Risky procedures for people in this category include dental extractions, dental and periodontal surgeries, implants, and the cleaning of teeth or implants where bleeding is expected.
- Some people with artificial joints are also at risk for developing infections around those joints. If you have an artificial knee or hip, for example, you could be at an elevated risk for infection after dental work.
-
2Evaluate your risk. Healthy patients aren’t usually prescribed antibiotics before or after dental procedures as part of the treatment. While one study suggests that preventative antibiotics taken post-op can reduce the risk of infection, it argues that the practice may do more harm than good. Talk to your dentist to see whether or not you are healthy enough to go without antibiotics.
- Check your medical history – do you know that you have any congenital heart defects? Have you ever had heart surgery? If you don’t remember, ask your general practitioner.
- Always be honest. Inform your dentist about any kind of health problem you had or you may have, as this can influence the entire treatment.
- Talk to your dentist to evaluate your risk. She should be able to advise you and, if you are at risk, she will likely prescribe you antibiotics.
-
3Follow the directions and take the appropriate dosage. Antibiotics are like any medicine and should be used with care. Follow your dentist’s instructions to the letter. Take the prescribed dosage for as long as she recommends, if your dentist decides to have you take preventative antibiotics.
- In the past, dentists and doctors recommended that at-risk patients take antibiotics before and after dental procedures. Today many instead advise patients to take a single dose about an hour before the procedure.
- If you’re at-risk you may receive penicillin. However, patients that are allergic to penicillin are often prescribed amoxicillin either in capsule or liquid form. Patients that can’t swallow medicine may be given injectable doses.
- If you are at-risk for endocarditis and develop a fever or other symptoms of infection after dental work, contact your doctor immediately.
Watching for Signs of Infection
-
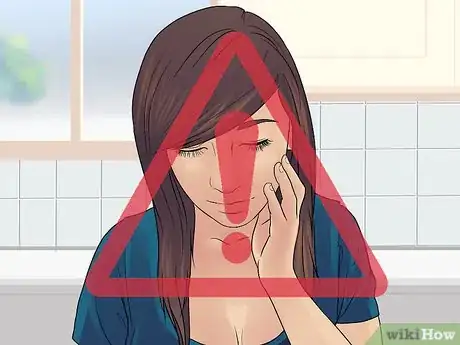
1Watch for tenderness and pain. An infection can form anywhere in your mouth, from your teeth and gums to your jaw, tongue, and palate. You should be vigilant in the days after your dental work and try to spot any developing infection. One of the most obvious signs is pain, discomfort, and tenderness near the site of the infection. You might also have a fever and pulsatile pain. You may notice that the discomfort also increases with touch or when in contact with hot and cold.[7]
- Does it hurt to chew or to touch the area of your mouth that’s affected? Infections are usually sensitive to touch and pressure.
- Does it hurt to eat hot food or to drink a cold beverage? Infections are also sensitive to temperature.
- Keep in mind that in some cases, dental infections may not show any symptoms, so it's important to keep any followup appointments with your dentist so they can monitor you for infection.[8]
-
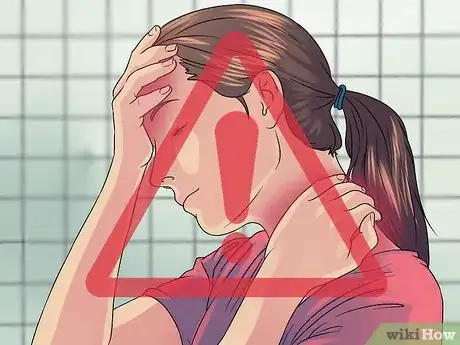
2Beware of swelling. Certain kinds of dental procedures may cause some swelling, like wisdom tooth extractions and periodontal surgery. Usually you can manage the level of swelling with ice packs. However, this sort of swelling should go down within about 3 days. If you have unexpected swelling or still have swelling three days after a major procedure, you might have an infection and should seek medical attention.[9]
- Swelling in the jaw and gums is often a sign of an infection, especially if you haven’t had an extraction or surgery at the site. Difficulty opening your mouth can also indicate that you have an infection.
- In some cases, you may find swelling in your neck or under your jaw. This is caused when an infection spreads to the lymph glands there and can be a very serious situation. See a medical professional immediately if you notice an infection in your head or neck.
-
3Note bad breath or foul tastes in the mouth. Another giveaway of an infection is a foul taste or smell in your mouth. This is caused by the build up of pus – white blood cells that have died while fighting the infection – and is an almost certain sign that you should see your dentist as soon as possible. Pus is one of the main hallmarks of infection.[10] [11]
- Pus tastes bitter and slightly salty and also smells bad. It may be the cause if you have a bad taste in your mouth that won’t go away or bad breath.
- Pus can get trapped inside your body in what’s called an abscess. If the abscess breaks, you will taste a sudden rush of bitter and salty fluid. You might also feel some pain relief.
- Talk to your dentist or a doctor if you notice pus in your mouth. You will need to get be treated for infection.
Expert Q&A
-
QuestionIf I just received dental work, what are some steps I should take to prevent infections?
 Tu Anh Vu, DMDDr. Tu Anh Vu is a board certified dentist who runs her private practice, Tu's Dental, in Brooklyn, New York. Dr. Vu helps adults and kids of all ages get over their anxiety with dental phobia. Dr. Vu has conducted research related to finding the cure for Kaposi Sarcoma cancer and has presented her research at the Hinman Meeting in Memphis. She received her undergraduate degree from Bryn Mawr College and a DMD from the University of Pennsylvania School of Dental Medicine.
Tu Anh Vu, DMDDr. Tu Anh Vu is a board certified dentist who runs her private practice, Tu's Dental, in Brooklyn, New York. Dr. Vu helps adults and kids of all ages get over their anxiety with dental phobia. Dr. Vu has conducted research related to finding the cure for Kaposi Sarcoma cancer and has presented her research at the Hinman Meeting in Memphis. She received her undergraduate degree from Bryn Mawr College and a DMD from the University of Pennsylvania School of Dental Medicine.
Board Certified Dentist Make sure to ask your dentist for post-op instructions for specific dental procedures. However, to prevent future dental infections, have good oral hygiene by brushing twice a day and flossing at least once a day.
Make sure to ask your dentist for post-op instructions for specific dental procedures. However, to prevent future dental infections, have good oral hygiene by brushing twice a day and flossing at least once a day.
References
- ↑ Tu Anh Vu, DMD. Dentist. Personal interview. 7 May 2020.
- ↑ http://www.mayoclinic.org/tests-procedures/wisdom-tooth-extraction/basics/what-you-can-expect/prc-20020652
- ↑ Tu Anh Vu, DMD. Dentist. Personal interview. 7 May 2020.
- ↑ https://www.pacificofs.com/p/BLOG-65762-2019.10.15-Rinsing-with-Salt-Water-After-Oral-Surgery-Can-Speed-Up-Healing-p.asp
- ↑ http://www.mayoclinic.org/tests-procedures/wisdom-tooth-extraction/basics/what-you-can-expect/prc-20020652
- ↑ https://www.sepsis.org/sepsisand/dental-health/
- ↑ https://www.sepsis.org/sepsisand/dental-health/
- ↑ Tu Anh Vu, DMD. Dentist. Personal interview. 7 May 2020.
- ↑ https://www.merckmanuals.com/home/mouth-and-dental-disorders/urgent-dental-problems/complications-after-dental-treatment































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...