This article was medically reviewed by Janice Litza, MD. Dr. Litza is a board certified Family Medicine Physician in Wisconsin. She is a practicing Physician and taught as a Clinical Professor for 13 years, after receiving her MD from the University of Wisconsin-Madison School of Medicine and Public Health in 1998.
There are 9 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 36,506 times.
Lymphatic filariasis is a parasitic disease common to tropical areas worldwide. According to the WHO, the parasite is usually transmitted to humans through mosquitos, and it affects the lymphatic system—the system that fights infections and balances fluids in your body.[1] People suffering from the disease may have lymphedema (swelling from fluid build-up) and elephantiasis (engorgement and thickened skin, often of the leg). Learn to prevent lymphatic filariasis by avoiding mosquito bites that spread the disease, and recognize when an infection is present.[2]
Steps
Identifying Signs and Symptoms
-
1Recognize lymphedema. Because the parasite infection damages the lymph system, the most common symptom is lymphedema–fluid buildup and swelling. This usually occurs in the leg or legs, but can also occur in one or both arms, breasts, and the genitalia.[3] Lymphedema will make the affected area feel puffy, heavy, and swollen; sometimes pressing the skin will leave a small dent due to the fluid buildup. If you experience lymphedema, you should absolutely see your doctor; you can also try to minimize symptoms by:[4]
- Elevating and exercising the swollen limb to improve the movement of fluids.
- Washing the affected area with soap and water daily to avoid skin infections.
- Using antibacterial or antifungal cream as needed, and properly disinfecting any wounds. Washing, disinfecting, and using fungal creams are meant to reduce infection of the affected leg. The swelling decreases circulation to the skin, so there is more risk for infection.
-
2Identify elephantiasis. With a poorly functioning lymphatic system, it’s also harder for your body to fight infections. Bacteria can more frequently infect the skin, especially the damaged skin of areas suffering from lymphedema. Over time this causes hardening and thickening of the skin, known as elephantiasis.[5]
- You can’t really prevent lymphedema, but you can try to prevent elephantiasis by warding off skin infections.[6] Keep your skin clean and dry as much as possible and use antibacterial soap on affected areas. Wash your hands regularly. Keep any wounds or cuts in the skin clean and covered until they heal.
Advertisement -
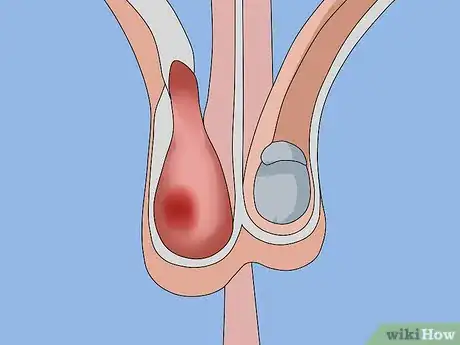
3Check for a swollen scrotum. Men infected with LF may experience swelling in the scrotum. This is also due to fluid buildup, and is called a hydrocele.[7] Sometimes hydroceles can resolve on their own after several months.[8] However, with a poorly functioning lymph system, it likely requires surgical treatment.[9]
-
4Look for associated breathing problems. A rare disorder that can be caused by lymphatic filariasis is called pulmonary tropical eosinophilia syndrome. This is a pulmonary disorder (i.e. it affects the lungs), and can cause a persistent cough, shortness of breath, and wheezing or gasping for breath.[10]
- Those infected usually live in Asia. If you experience these breathing symptoms and have spent time in tropical climates, get tested for LF.
- Pulmonary tropical eosinophilia syndrome can be diagnosed with a blood test. Blood will show high levels of eosinophils, a certain type of blood cell that increases when your body is exposed to allergens or parasites. You will also have high levels of immunoglobulin E (IgE) and antifilarial antibodies.[11]
-
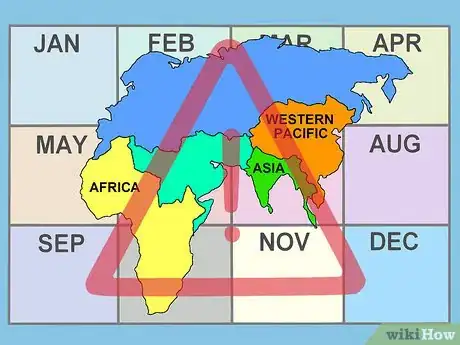
5Know your risk factors. You are at the highest risk for infection if you spend a significant time (months to years) in a tropical or sub-tropical area where the disease is common (or endemic).[12]
- The disease is present in over 73 countries in Asia, Africa, the Western Pacific, and some tropical areas of the Caribbean and South America (Haiti, the Dominican Republic, Guyana, and Brazil).[13]
- Tourists visiting these areas for short times have a low risk of infection, but it’s still best to take preventative measures and be aware of symptoms.[14]
-
6Remember that symptoms may not develop for years after infection. The majority of people infected with lymphatic filariasis will never develop symptoms. However, a small number of those infected may start to have symptoms after being infected for years.[15] Even if you haven’t lived in an endemic area for years, always consider lymphatic filariasis as a possible cause of symptoms associated with lymphatic dysfunction and severe swelling.
- Because there are other more common causes of lymphedema, it is important to tell your doctor if you have traveled to endemic areas. Your doctor is unlikely to consider filariasis without you sharing your travel history.
-
7Get diagnosed. An infection with lymphatic filariasis will show up on a blood test if a doctor has the equipment to look for the worms under a microscope. The worms are sometimes nocturnal and only circulate in the blood at night, so the blood test has to occur from blood taken at nighttime.[16]
- However, because symptoms might not occur until years after infection, some patients with LF will have a negative blood test. Other methods of diagnosing LF use blood serum to look for antibodies to the worms, which can be more accurate.[17]
Preventing Disease Transmission
-
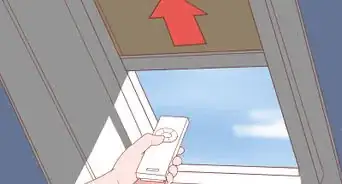
1Avoid mosquito bites at night. The worms that cause lymphatic filariasis are spread person-to-person through mosquito bites. Avoiding mosquito bites when in endemic areas is the best way to avoid infection, though it generally takes months to years of repeated bites to become infected.[18] Protect yourself at night when mosquitoes are most active.
-
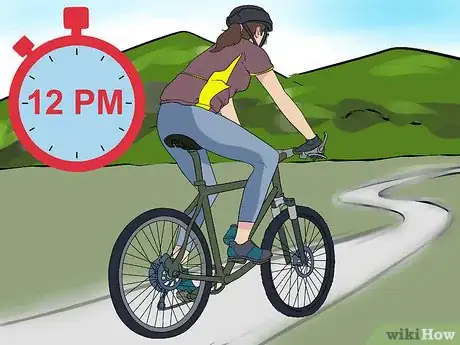
2Plan your outdoor activities for when the sun is up. The mosquitoes that transmit LF usually bite between dusk and dawn. When possible, limit your time outdoors in endemic areas to after dawn and before dusk – i.e. largely during daytime hours.[21]
-
3Cover your skin with clothing. As much as possible, wear long sleeve shirts, long pants, and socks. Cover as much skin as possible to minimize areas for mosquito bites.[22]
-
4Use a mosquito repellent on exposed skin. Obtain a natural or chemical mosquito repellent, or make your own at home, and be diligent about using it regularly.[23] Effective repellents usually contain either DEET, icaridin (or picaridin), or the oil of lemon eucalyptus.[24]
- Apply mosquito repellent outside, away from food, and at least 20 minutes after putting on sunscreen if you’re using both.
- Cover up any rashes, wounds, burns, or cuts before putting on mosquito repellent.
-
5Get medicated to avoid infecting others. Those actively infected with LF can take a yearly dose of a medication called diethylcarbamazine (DEC). This drug does not kill all of the worms, but it prevents you from spreading the disease to another person.
- If you live in North America or another area where LF is not common, your doctor will have to get this medication from the Centers for Disease Control and Prevention (CDC) or other agency that deals with rare disorders.[25]
- The medication is usually well tolerated, with minor possible side effects of dizziness, headache, fever, nausea, or muscle aches.[26]
- Other treatment options are ivermectin and albendazole.[27]
Warnings
- The adult worms live in your lymphatic system for about 5-7 years, but lymphedema and other symptoms can develop even after the adult worms die.⧼thumbs_response⧽
- Mosquitoes transmit many potentially serious diseases. If you travel abroad or live in areas with endemic diseases spread by mosquitoes (such as malaria), seek emergency medical care if you experience any of these symptoms:
- Chills, shaking, or excessive sweating
- Headache or muscle aches
- Nausea, with or without vomiting
- Fever over 101°F (38.3°C)
⧼thumbs_response⧽
References
- ↑ https://www.who.int/news-room/fact-sheets/detail/lymphatic-filariasis
- ↑ https://www.cdc.gov/parasites/lymphaticfilariasis/index.html
- ↑ https://www.cdc.gov/parasites/lymphaticfilariasis/gen_info/faqs.html
- ↑ https://www.cdc.gov/parasites/lymphaticfilariasis/gen_info/faqs.html
- ↑ https://www.cdc.gov/parasites/lymphaticfilariasis/gen_info/faqs.html
- ↑ https://www.cdc.gov/parasites/lymphaticfilariasis/gen_info/faqs.html
- ↑ https://www.cdc.gov/parasites/lymphaticfilariasis/gen_info/faqs.html
- ↑ http://www.mayoclinic.org/diseases-conditions/hydrocele/basics/treatment/con-20024139
- ↑ http://www.mayoclinic.org/diseases-conditions/hydrocele/basics/treatment/con-20024139
- ↑ https://www.cdc.gov/parasites/lymphaticfilariasis/gen_info/faqs.html
- ↑ https://www.cdc.gov/parasites/lymphaticfilariasis/gen_info/faqs.html
- ↑ https://www.cdc.gov/parasites/lymphaticfilariasis/gen_info/faqs.html
- ↑ https://www.cdc.gov/parasites/lymphaticfilariasis/epi.html
- ↑ https://www.cdc.gov/parasites/lymphaticfilariasis/epi.html
- ↑ https://www.cdc.gov/parasites/lymphaticfilariasis/gen_info/faqs.html
- ↑ https://www.cdc.gov/parasites/lymphaticfilariasis/gen_info/faqs.html
- ↑ https://www.cdc.gov/parasites/lymphaticfilariasis/gen_info/faqs.html
- ↑ https://www.cdc.gov/parasites/lymphaticfilariasis/gen_info/faqs.html
- ↑ https://www.cdc.gov/parasites/lymphaticfilariasis/gen_info/faqs.html
- ↑ https://www.cdc.gov/parasites/lymphaticfilariasis/prevent.html
- ↑ https://www.cdc.gov/parasites/lymphaticfilariasis/gen_info/faqs.html
- ↑ https://www.cdc.gov/parasites/lymphaticfilariasis/gen_info/faqs.html
- ↑ https://www.cdc.gov/parasites/lymphaticfilariasis/gen_info/faqs.html
- ↑ http://www.mayoclinic.org/diseases-conditions/mosquito-bites/basics/prevention/con-20032350
- ↑ https://www.cdc.gov/parasites/lymphaticfilariasis/gen_info/faqs.html
- ↑ https://www.cdc.gov/parasites/lymphaticfilariasis/treatment.html
- ↑ https://rarediseases.info.nih.gov/diseases/3321/lymphatic-filariasis
About This Article
To recognize lymphatic filariasis, consider if you've spent a long time in a sub-tropical or tropical climate, which is where the disease can be contracted. Next, check for swelling or a build-up of fluid in the legs, arms, breasts, or genitals. You may also notice breathing problems, like gasping or coughing. See your doctor as soon as you notice any symptoms, since lymphatic filariasis is a contagious disease. In order to prevent lymphatic filariasis, wash your skin daily with soap and water. Additionally, protect yourself against mosquito bites at night by using a net over your bed, since the disease is spread by mosquitoes. For tips from our Medical co-author on how to avoid infecting others if you have lymphatic filariasis, read on!


































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...