This article was medically reviewed by Janice Litza, MD. Dr. Litza is a board certified Family Medicine Physician in Wisconsin. She is a practicing Physician and taught as a Clinical Professor for 13 years, after receiving her MD from the University of Wisconsin-Madison School of Medicine and Public Health in 1998.
There are 23 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 145,093 times.
Experts say that symptoms of Parkinson's disease usually start slowly with a tremor in one hand, along with stiffness and slowing movement. Over time, you may develop more symptoms on both sides of your body.[1] Parkinson's disease is a condition where your brain's nerve cells don't produce enough dopamine, which effects your motor skills. Research suggests that Parkinson's disease can be difficult to diagnose because there's no test for it, so your doctor will likely review your medical records and do a neurological exam.[2] Getting an early diagnosis can help you get the best treatment to help manage your symptoms, so talk to your doctor if you think you might have symptoms of Parkinson's disease.
Steps
Recognizing Early Symptoms of Parkinson's Disease
-
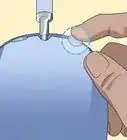
1Notice any shaking or twitching.[3] When you think of Parkinson's disease, the first thing to come to mind may be tremors. These can occur anywhere on the body: a shaking finger or leg, a twitching eye, a trembling lip or chin, etc. Note that some shaking and twitching can be perfectly normal — for example, after strenuous exercise or after an injury. Some medications can also cause tremors, so ask your doctor about the medications you are currently taking.
-
2Look for the onset of muscle rigidity.[4] After tremors, rigidity is the most well-known symptom of Parkinson's disease. Take note if your muscles feel stiff, even if you haven't over-exerted them recently. You might also see a decrease in flexibility or an increase in muscle pain or cramps.
- Muscle rigidity in the face sometimes causes people with Parkinson's to develop a “mask”-like, blank expression.[5] The Parkinson's mask is characterized by staring with little blinking, little or no smiling, and the general suggestion that the person is angry, even if he or she feels just fine.
- You may also notice the development of slouched posture due to rigidity. This might mean the person hunches forward, or they may bend over to one side more than the other.[6]
Advertisement -
3Track bowel movements. When you think of the loss of muscle control that comes with Parkinson's disease, you may think of the decreased ability to walk, talk, eat, and so on. However, the disease also affects the autonomic nervous system, which controls the movements and function of the internal organs — the muscles we never think about using.[7] If the autonomic nervous system is affected, the intestinal tract may not work properly, causing constipation.
- Failure to have a bowel movement every day does not necessarily indicate constipation. For some people, it may be normal to go 3-4 days between movements.
- Constipation is marked by a significant decrease in movement frequency. They are also drier than usual, and difficult to pass. You may find that you're straining when you use the bathroom.
- Make allowances for other causes of constipation. These might include dehydration, fiber deficiency, excessive alcohol, caffeine or dairy, and stress, among other potential causes.[8]
-
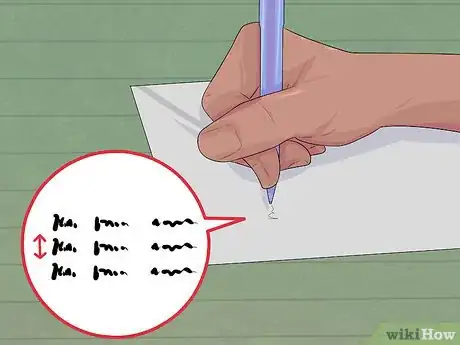
4Be aware of the signs of micrographia. Parkinson's affects motor skills and causes muscle stiffness, so people who have it often find that it becomes more and more difficult to write. Micrographia is a change in handwriting commonly associated with the disease. Take note if:[9]
- Your handwriting becomes small and more cramped than usual
- You can no longer write in a smooth, fluid motion
- Your hands feel tight when writing
- Note that micrographia is usually marked by a sudden rather than gradual change.
-
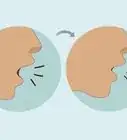
5Make note of vocal changes. 90% of people with Parkinson's will experience a decrease in speech ability. The most common early symptom of this is a softening or quieter voice, though speech can also become breathy or hoarse. Some people may find that their speech gets slower, while others — about 10% — speed up their rate of talking, resulting in stumbling, stuttering speech. It might be hard to notice these changes in yourself, so ask the people around you if they notice any change in your speech.[10]
-
6Be vigilant for signs of hyposmia. Over 90% of people with Parkinson's disease suffer from hyposmia, or a loss of the ability to smell.[11] Research suggests that the decrease in ability to smell is a predictor for the dementia that accompanies Parkinson's disease, and can precede motor and coordination problems by several years.[12] If you suspect your ability to smell might be decreasing, test yourself with bananas, dill pickles, or licorice before contacting a medical professional.[13]
- Remember that there are other, completely harmless reasons for the sudden loss of smell. Let a cold, the flu, or a stuffy nose run their course before worrying about hyposmia.
-
7Take note of changes to normal sleep patterns. Trouble sleeping is an early indicator of Parkinson's, and is usually noticeable before any trouble with motor function.[14] Sleep problems can take many forms, including:
- Insomnia (the inability to fall asleep at night)[15]
- Feeling sleepy during the day (reported by 76% of Parkinson's sufferers) or having “sleep attacks” (sudden, involuntary onset of sleep)
- Nightmares or the “acting out” of dreams while you're asleep
- Sleep apnea (when you stop breathing for a few seconds at a time while asleep)[16]
-
8Do not disregard dizziness or fainting spells. While these symptoms can have a range of causes, in Parkinson's sufferers, they are due to orthostatic hypotension, a form of low blood pressure that affects 15-50% of patients. Orthostatic hypotension causes your blood pressure to drop suddenly and dramatically when you get up after standing or lying down for a period of time. This causes wooziness, trouble finding your balance, and even loss of consciousness.[17]
-
9Keep in mind that none of these symptoms alone indicates Parkinson's.[18] Each of the symptoms described in this section could either be due to normal stress on the body, or a different underlying medical condition. However, if more than one of these symptoms is observed together for an extended period of time, you should contact a medical professional to be tested for Parkinson's disease.[19]
Getting Tested for Parkinson's
-
1Understand the genetic causes and risks of Parkinson's disease. Only 1-2% of Parkinson's sufferers have genes that directly cause the development of the disease. Most people have “associated” genes, meaning that they are at a higher risk of developing Parkinson's, but will not necessarily have it even if they have the genetic predisposition for it. If associated genes are combined with other inherited genes or environmental factors, they can trigger the onset of Parkinson's. About 15-25% of people with the disease have relatives who suffered from it as well.[20]
- Age also increases your risk of developing Parkinson's. Whereas 1-2% of the general population suffers from the disease, 2-4% of the population over 60 years in age suffers from it.
- Be aware of your genetic risk factors and be able to provide them to your doctor.
-
2Approach your general practitioner with your concerns. Parkinson's disease can be difficult to diagnose, especially in its early stages. However, early detection is very important for maintaining a good quality of life for as long as possible. If you observe more than one of the symptoms listed in the previous section and have a family history of Parkinson's, ask your internist or family physician to go over your symptoms with you.
-
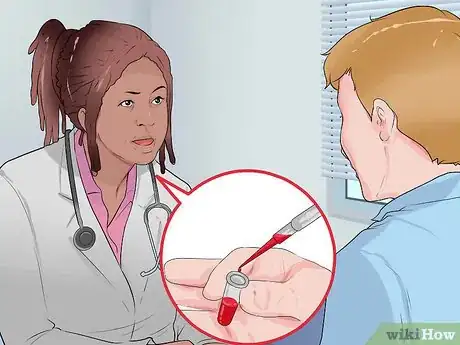
3Complete the doctor's evaluation exercises. There is no standard diagnostic test for Parkinson's disease, though scientists are working to find a biological marker — like blood tests or an imaging scan — that can confirm a diagnosis. But because we don't have that test yet, the doctor will instead draw on his or her knowledge of how the disease manifests and combine it with observations of your ability to complete some simple tasks. The test will likely test for the symptoms that were listed in the previous section:[21]
- Animation of the facial muscles
- The presence of tremors when your limbs are resting
- Limb or neck stiffness
- Ability to stand up suddenly without dizziness
- Flexibility and muscle strength
- Ability to regain balance quickly
-
4Follow up with a neurological specialist. Even if your family physician doesn't see any cause for concern, ask for a referral to a neurologist if you are still worried. A specialist will be more familiar with the signs of Parkinson's, and may disagree with your general practitioner's opinion.
- Be prepared for additional tests (blood tests, scans) that may be carried out to rule out other causes for the symptoms you've observed.[22]
-
5Ask about taking carbidopa-levodopa.[23] Carbidopa-levodopa is a medication that treats the symptoms of Parkinson's disease. If you begin taking the medication and notice an improvement in your symptoms, the doctor can use that information to confirm a diagnosis of Parkinson's disease.
- Make sure to take the medication as directed. If you space out the doses too much or don't take a high enough dose, the doctor won't be able to accurately gauge how much and why your symptoms improved or didn't improve.
-
6Get a second opinion. Because there is not yet a test for a biological marker of Parkinson's disease, it can be very difficult to get an accurate diagnosis — especially in the early stages. Getting second opinions will help ensure that you're getting the best possible treatment for whatever is causing your symptoms.
- If the doctors say you don't have Parkinson's, but the symptoms don't go away, get retested periodically. This is a progressive disease, and with time, the symptoms may progress to a stage that will allow a doctor to confirm a solid diagnosis.[24]
Expert Q&A
-
QuestionMy hand has been shaking recently for the past two days, is this a sign?
 Janice Litza, MDDr. Litza is a board certified Family Medicine Physician in Wisconsin. She is a practicing Physician and taught as a Clinical Professor for 13 years, after receiving her MD from the University of Wisconsin-Madison School of Medicine and Public Health in 1998.
Janice Litza, MDDr. Litza is a board certified Family Medicine Physician in Wisconsin. She is a practicing Physician and taught as a Clinical Professor for 13 years, after receiving her MD from the University of Wisconsin-Madison School of Medicine and Public Health in 1998.
Board Certified Family Medicine Physician Parkinson's is just one possible cause for tremors. If the shaking continues, I recommend that you see your doctor.
Parkinson's is just one possible cause for tremors. If the shaking continues, I recommend that you see your doctor. -
QuestionI'm very concerned about my 32-year-old father's symptoms. How can I get more information or help?
 Janice Litza, MDDr. Litza is a board certified Family Medicine Physician in Wisconsin. She is a practicing Physician and taught as a Clinical Professor for 13 years, after receiving her MD from the University of Wisconsin-Madison School of Medicine and Public Health in 1998.
Janice Litza, MDDr. Litza is a board certified Family Medicine Physician in Wisconsin. She is a practicing Physician and taught as a Clinical Professor for 13 years, after receiving her MD from the University of Wisconsin-Madison School of Medicine and Public Health in 1998.
Board Certified Family Medicine Physician The first step is to go see his doctor together. You can ask the doctor questions and make sure your concerns are addressed. You can also visit the national website for information: http://www.parkinson.org/
The first step is to go see his doctor together. You can ask the doctor questions and make sure your concerns are addressed. You can also visit the national website for information: http://www.parkinson.org/
References
- ↑ https://www.nia.nih.gov/health/parkinsons-disease
- ↑ https://medlineplus.gov/parkinsonsdisease.html
- ↑ http://www.parkinson.org/understanding-parkinsons/10-early-warning-signs
- ↑ http://www.parkinsons.org.uk/content/rigidity-parkinsons
- ↑ https://my.clevelandclinic.org/health/diseases/8525-parkinsons-disease-an-overview
- ↑ https://www.parkinson.org/Understanding-Parkinsons/Symptoms/Movement-Symptoms/Stooped-Posture
- ↑ https://www.apdaparkinson.org/article/bowel-and-bladder-management-in-advanced-parkinsons-disease/
- ↑ https://my.clevelandclinic.org/health/diseases/4059-constipation
- ↑ https://www.parkinson.org/Understanding-Parkinsons/Symptoms/Non-Movement-Symptoms/Small-Handwriting
- ↑ https://www.parkinson.org/Understanding-Parkinsons/Symptoms/Non-Movement-Symptoms/Speech-and-Swallowing-Problems
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3429117/
- ↑ http://www.ncbi.nlm.nih.gov/pubmed/24482154
- ↑ http://www.parkinson.org/understanding-parkinsons/10-early-warning-signs
- ↑ http://sleepfoundation.org/sleep-topics/parkinsons-disease-and-sleep
- ↑ http://sleepfoundation.org/insomnia/content/what-is-insomnia
- ↑ http://sleepfoundation.org/sleep-disorders-problems/sleep-apnea
- ↑ https://www.parkinson.org/Understanding-Parkinsons/Symptoms/Non-Movement-Symptoms/Vertigo-Dizziness-Parkinsons
- ↑ http://www.parkinson.org/understanding-parkinsons/10-early-warning-signs
- ↑ https://www.nhs.uk/conditions/parkinsons-disease/diagnosis/
- ↑ https://www.hopkinsmedicine.org/health/conditions-and-diseases/parkinsons-disease/parkinsons-disease-risk-factors-and-causes
- ↑ https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/how-parkinson-disease-is-diagnosed
- ↑ https://www.parkinson.org/Understanding-Parkinsons/Diagnosis/How-a-Diagnosis-is-Made
- ↑ https://medlineplus.gov/druginfo/meds/a601068.html
- ↑ https://www.parkinson.org/Understanding-Parkinsons/What-is-Parkinsons/Stages-of-Parkinsons
About This Article
To recognize the symptoms of Parkinson’s Disease, take note of twitching or tremors in your limbs, eyes, or muscles. You should also look for stiff muscles, especially if you’ve not been exercising. Additionally, watch for signs that you're losing your ability to smell. Then, notice changes in your handwriting, known as micrographia, which suggests muscle stiffness and a loss of motor skills. If you observe two or more of these symptoms over an extended period of time, contact your doctor to get tested for Parkinson's. For tips from our Medical co-author on how to get tested for Parkinson’s, read on!

































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...