This article was co-authored by wikiHow Staff. Our trained team of editors and researchers validate articles for accuracy and comprehensiveness. wikiHow's Content Management Team carefully monitors the work from our editorial staff to ensure that each article is backed by trusted research and meets our high quality standards.
There are 12 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 28,432 times.
Learn more...
High uric acid can lead to a form of arthritis called gout and other medical issues. If routine blood work or a uric acid test showed that you have elevated levels, try not to get overwhelmed. There are plenty of things you can do to manage uric acid. For moderately high levels, you may only need to make dietary changes. Your doctor may, if necessary, prescribe medication to lower your uric acid levels. If you have gout, flare-ups can be painful, but try not to worry. There are lots of steps you can take to keep pain and swelling in check.
Steps
Maintaining a Healthy Diet
-
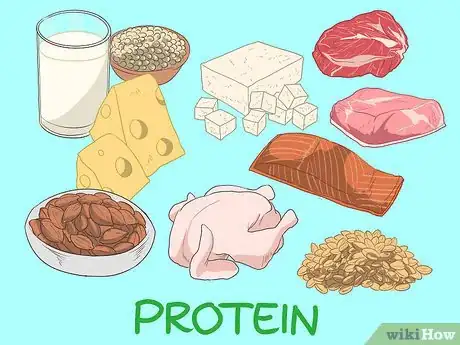
1Go for lean meats instead of fatty, purine-rich cuts. Good protein choices include boneless, skinless chicken, lentils, and beans. Do your best to avoid eating red meat, bacon, and organ meat, such as brain, kidney, and liver.[1]
- Red and organ meat contain higher levels of purines, which are substances that can increase uric acid levels. Check with your doctor about avoiding or limiting purine-rich foods while still meeting your nutritional requirements.
-
2Consume seafood in moderation. While you can eat salmon, shrimp, and crab in moderation, there are several kinds of seafood you should avoid altogether. Items to avoid include anchovies, haddock, herring, mackerel, mussels, sardines, and scallops.[2]
- Avoid eating seafood more than 2 to 3 times per week, or as directed by your doctor.
Advertisement -
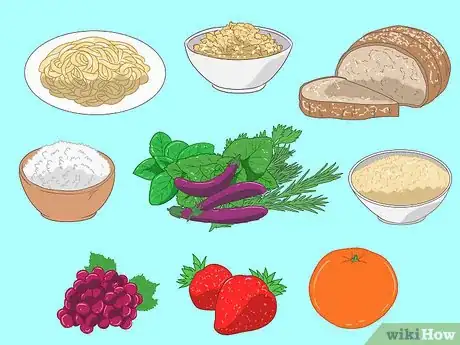
3Eat more complex carbs, such as fruits, veggies, and whole grains. Complex carbs are an important part of a healthy diet, and are especially beneficial if you have high uric acid levels. Each day, try to eat about 3 cups (400 g) each of fruit and veggies and 2 to 5 servings of whole grains. Example whole grain servings include 1 slice of bread and ½ cup (75 to 120 g) of pasta, quinoa, oatmeal, or brown rice.[3]
- Make sure your breads and pastas are labeled “whole grain,” as they’re healthier choices than refined products.
-
4Limit your sugar intake. Manage your dietary intake by avoiding soft drinks and other sweetened beverages, and drink sports drinks sparingly. Do your best to stay away from candy, sweet pastries and desserts, and other sugary foods. Check the labels for cereals, condiments, and other items as well, and avoid products that contain added sugars.[4]
- Purines are released as your body breaks down the type of sugar found in sweets and soft drinks. In turn, purines lead to spikes in uric acid levels and gout flare-ups.
Tip: While fruit is an important part of your diet, you should only drink fruit juice in moderation. Additionally, choose low-sugar juices that do not contain added sweeteners. Drinking too much fruit juice could cause spikes in your sugar levels.[5]
-
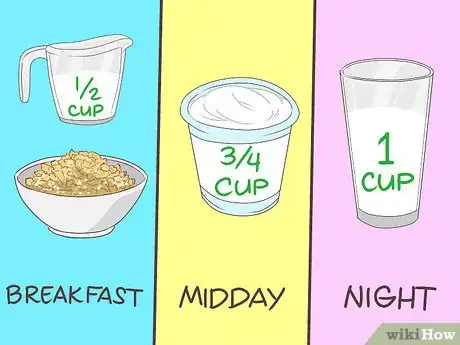
5Include low-fat dairy products in your diet. Try to get 3 servings of dairy per day; just be sure to choose low-fat or skim products. A sample menu could be 1⁄2 cup (120 mL) of milk with your breakfast cereal, ¾ cup (200 g) of yogurt as a midday snack, and a 1 cup (240 mL) glass of milk before bed.[6]
- Dairy products may lower uric acid levels by helping your body flush the substances that form uric acid.
- If you’re dairy-free, you’ll need non-dairy alternatives to meet your daily calcium needs, but they may not have the same effect on uric acid levels as actual dairy.
Making Lifestyle Changes
-
1Drink at least 8 to 10 cups (1.9 to 2.4 L) of fluids per day. Staying hydrated helps your kidneys flush uric acid and other substances from your body. The exact amount you need depends on factors like age and activity level, but 8 to 10 cups (1.9 to 2.4 L) is a good rule of thumb.[7]
- Remember to drink more liquids when it’s hot, during physical activity, and when you’re sweating a lot. Drinking 1 cup (240 mL) every 20 minutes during these periods should do the trick.
- Don’t wait to drink until you’re thirsty, as thirst means you’re started to get dehydrated. Instead, check your urine to gauge your hydration. If it’s dark yellow in color, you need to drink more fluids.
-
2Avoid drinking alcohol, especially during gout flare-ups. Wine in moderation may be acceptable, but avoid drinking daily and don’t consume more than 1 to 2 glasses per sitting. Steer clear of beer and liquor, as they’re particularly harmful if you have high uric acid levels.[8]
- If you have gout, avoid alcohol altogether during an attack.
- Ask your doctor for recommendations on drinking in moderation, especially if you have medical issues other than high uric acid.
-
3Try to lose weight gradually, if necessary. If you’re overweight, aim to lose about 1 pound (450 g) per week. Being overweight makes it harder for your kidneys to remove uric acid from your body. Track the amount of calories you ingest and do your best to stay as active as possible. Keep in mind dramatic weight loss can increase uric acid levels, so avoid crash diets and don’t skip meals.[9]
- In addition to managing uric acid, maintaining a health diet and losing weight can help reduce strain on your joints. If you have gout, lowering joint stress can help you manage pain and maintain joint function.
- Find out your daily recommend calorie intake, and try not to exceed that number. Additionally, eat a healthy, low-fat, and low-sugar diet. Swapping soft drinks for water is also a great way to cut calories.
- Try to get 30 minutes of light to moderate exercise per day, or according to your doctor's instructions. Keep meal and exercise journals to track your progress.
- Calculate your daily calorie and nutritional needs at https://www.choosemyplate.gov/myplateplan.
-
4Keep your stress levels in check. Stress can aggravate gout, and reducing stress may help lower uric acid levels. Try including relaxation exercises in your routine, such as meditating for 15 or 20 minutes a day or breathing slowly and deeply when you feel stressed.[10]
- Avoid over-scheduling yourself or taking on too many commitments. If you're feeling overwhelmed, ask a friend a relative to help you with responsibilities such as childcare, housework, and errands.
Managing Uric Acid Levels with Medication
-
1Take allopurinal if you have recurrent or severe symptoms. If you have frequent gout flare-ups, joint damage, or kidney stones, your doctor will prescribe a drug that reduces the uric acid in your blood. Of these medications, allopurinal is the most commonly prescribed. You’ll most likely start by taking 50 to 100 mg orally per day, then your doctor will gradually increase your dose to 200 to 300 mg.[11]
- Side effects may include nausea, diarrhea, and headache. If side effects interfere with your quality of life, ask your doctor if it’s possible to try another medication for uric acid.
Safety Tip: Even if you experience undesirable side effects, don’t stop taking a prescription medication without consulting your doctor. Additionally, take your medication as directed even if you don’t experience symptoms, as stopping could lead to a flare-up.[12]
-
2Control uric acid with pegloticase if other drugs aren’t effective. If allopurinal or similar oral drugs are ineffective or cause intolerable side effects, your doctor may prescribe pegloticase injections. It’s usually administered every 2 weeks, and you’ll need to visit your doctor’s office to receive injections.[13]
- Side effects may include nausea, vomiting, constipation, bruising, and sore throat. Tell your doctor if any side effects are severe, or if you experience rash, difficulty breathing, or swelling.[14]
-
3Consult your doctor about managing any underlying conditions. Elevated uric acid levels may be caused by or associated with conditions including diabetes, high blood pressure, high cholesterol, and kidney disease. If you have any underlying medical issues and don’t already take medication, work with your doctor to develop a treatment plan for your specific condition.[15]
- Note that diuretics, which are prescribed for high blood pressure and a range of other medical conditions, can increase uric acid levels. Ask your doctor if a drug could affect your uric acid levels and see if you should take any steps to lower your risk, such as drinking more water.[16]
Relieving Pain during a Flare-up
-
1Ice the affected joint during a flare-up. To manage pain and inflammation, apply ice for 15 to 20 minutes every 1 to 2 hours. Be sure to wrap ice or an ice pack in a towel instead of holding it directly against your skin.[17]
- Additionally, do your best to avoid using the affected joint as long as symptoms like pain, swelling, or redness persist.
-
2Manage your symptoms with an over-the-counter pain reliever. Your doctor may suggest taking a high-dose NSAID pain reliever, such as ibuprofen or naproxen, while symptoms persist. Check with them about the right amount of medicine to take. Dosages used to treat gout flare-ups are typically higher than the maximum amount recommended on instruction labels.[18]
- For instance, your doctor may advise taking 800 mg of ibuprofen 4 times a day while you experience symptoms and for an additional 24 hours after pain and inflammation subside.
Warning: Consult your doctor before taking NSAID pain relievers if you have an ulcer, kidney issues, liver disease, heart failure, or a bleeding condition, or if you take a blood thinner.[19]
-
3Take colchicine at the first sign of a flare-up. Colchicine is a prescription medication that’s usually taken in tablet form 1 to 2 times per day during a flare-up. It’s most effective when taken as soon as possible after symptoms develop. If you have gout, your doctor will write you a prescription so you’ll have it on hand in case a flare-up occurs.[20]
- Most people who take colchicine experience nausea, vomiting, or diarrhea. If side effects interfere with your normal routine, talk to your doctor about lowering your dose.
- Do not eat grapefruit or drink grapefruit juice while taking colchicine.
-
4Talk to your doctor about oral or injected corticosteroids. Corticosteroids are generally only recommended for people who can’t take NSAIDs and colchicine, or if these medications are ineffective. If 1 or 2 of your joints are affected, your doctor will probably inject a corticosteroid directly into each one. For widespread or frequent flare-ups, you may need to take an oral corticosteroid.[21]
- While you may experience discomfort at the injection site, side effects are usually minimal for injected corticosteroids.
- Systemic oral corticosteroids may cause side effects including weight gain, high blood sugar, and increased risk for infections.
Warnings
- While there are often no symptoms of high uric acid levels, signs may include kidney stones and joint pain, stiffness, swelling, or burning. See your doctor if you suspect you may have high uric acid levels, have risk factors like eating a high-fat diet or being overweight, or experience any unusual symptoms.[25]⧼thumbs_response⧽
- Consult your doctor or a registered dietitian before making any changes to your diet.[26]⧼thumbs_response⧽
References
- ↑ https://www.mayoclinic.org/healthy-lifestyle/nutrition-and-healthy-eating/in-depth/gout-diet/art-20048524
- ↑ https://www.mayoclinic.org/healthy-lifestyle/nutrition-and-healthy-eating/in-depth/gout-diet/art-20048524
- ↑ https://www.mayoclinic.org/healthy-lifestyle/nutrition-and-healthy-eating/in-depth/gout-diet/art-20048524
- ↑ https://www.mayoclinic.org/healthy-lifestyle/nutrition-and-healthy-eating/in-depth/gout-diet/art-20048524
- ↑ https://www.rheumatology.org/I-Am-A/Patient-Caregiver/Diseases-Conditions/Gout
- ↑ https://www.rheumatology.org/I-Am-A/Patient-Caregiver/Diseases-Conditions/Gout
- ↑ https://www.healthdirect.gov.au/gout
- ↑ https://www.mayoclinic.org/healthy-lifestyle/nutrition-and-healthy-eating/in-depth/gout-diet/art-20048524
- ↑ https://www.cdc.gov/arthritis/basics/gout.html
- ↑ https://www.arthritis.org/about-arthritis/types/gout/treatments/types.php
- ↑ https://medlineplus.gov/ency/article/000422.htm
- ↑ https://www.health.harvard.edu/newsletter_article/all-about-gout
- ↑ https://www.rheumatology.org/I-Am-A/Patient-Caregiver/Diseases-Conditions/Gout
- ↑ https://medlineplus.gov/druginfo/meds/a611015.html
- ↑ https://www.cdc.gov/arthritis/basics/gout.html
- ↑ https://newsinhealth.nih.gov/2014/02/gripped-gout
- ↑ https://www.healthdirect.gov.au/gout
- ↑ https://medlineplus.gov/ency/article/000422.htm
- ↑ https://www.rheumatology.org/I-Am-A/Patient-Caregiver/Diseases-Conditions/Gout
- ↑ https://www.aafp.org/afp/1999/0215/p925.html
- ↑ https://www.aafp.org/afp/1999/0215/p925.html
- ↑ https://www.rheumatology.org/I-Am-A/Patient-Caregiver/Diseases-Conditions/Gout
- ↑ https://www.health.harvard.edu/newsletter_article/all-about-gout
- ↑ https://www.mayoclinic.org/diseases-conditions/gout/symptoms-causes/syc-20372897
- ↑ https://www.mayoclinic.org/diseases-conditions/gout/symptoms-causes/syc-20372897
- ↑ https://www.niams.nih.gov/health-topics/gout#tab-living-with




































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...