This article was co-authored by David Schechter, MD. Dr. David Schechter is a physician in Culver City, California. With over 25 years of experience as a family and sports medicine physician, Dr. Schechter specializes in mind-body medicine, preventive medicine, and chronic pain. Dr. Schechter received his MD from New York University and is an attending physician at Cedars-Sinai Medical Center. He was named a Top Doctor by Los Angeles Magazine and Men's Health Magazine. He has also written several books, including The MindBody Workbook.
There are 22 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 235,862 times.
Hemorrhoids, or piles, are enlarged and inflamed veins located in the lower rectum and anus. They are common, and almost half of all adults have dealt with them at least once before age 50. Hemorrhoids result from increased pressure on the lower rectum and anus. The increased pressure within the hemorrhoidal veins causes them to swell. Symptoms you may notice include painless bleeding during bowel movements, rectal/anal pain, anal itching, and/or tender lumps near the anus.[1] You have a wide array of options when it comes to treating hemorrhoids and hemorrhoid pain both at home and via your physician.
Steps
Treating Hemorrhoid Pain at Home
-
1Use a Sitz bath. These baths can provide immediate relief of pain and itching from hemorrhoids. Soak the anal area in warm water for 10 to 20 minutes two to three times per day and following bowel movements. Pharmacies sell small plastic tubs that fit over the toilet seat. Alternatively, you can fill a bathtub to approximately hip level with warm water.[2]
- Fill the bathtub with about 6 in (15 cm) of warm or hot water as you prepare your bath.[3]
- Gently pat the anal area dry with a towel or use a hair dryer after each treatment.
-
2Apply cold treatments to the area. Cold treatment can alleviate swelling and pain associated with hemorrhoids. You can apply a frozen, water-filled condom or ice cubes wrapped in a cloth to the anal area for 5-10 minutes 3-4 times per day.[4]
- Gently pat the anal area dry with a towel or use a hair dryer after each treatment.
Advertisement -
3Try over-the-counter topical agents. Your local pharmacy will have a variety of OTC products designed to help with the pain and discomfort associated with hemorrhoids. Some of these products include:[5]
- You can use pads such as Tucks as compresses on irritated hemorrhoids up to six times per day to relieve pain and itching. These have witch hazel, which is a soothing, natural anti-inflammatory agent.
- Preparation H cream is a topical anesthetic, constrictor of blood vessels (vasoconstrictor), and skin protectant useful in the treatment of hemorrhoids. The cream blocks pain signals coming from the nerve endings of the anal area and also shrinks swollen, inflamed tissue.[6]
- OTC creams or suppositories containing the steroid hydrocortisone can also be helpful in the treatment of hemorrhoids. Hydrocortisone is a potent anti-inflammatory agent that can help ease the pain and itching of hemorrhoids. Topical steroids such as hydrocortisone should not be used for more than one week as they can lead to atrophy (or thinning) of the skin in the anal area.
- Pramoxine, available OTC and by prescription, is another topical anesthetic used to treat hemorrhoids.[7]
-
4Take oral pain relievers. OTC oral pain relievers such as acetaminophen (Tylenol), ibuprofen (Advil), or aspirin can be used to help relieve the discomfort of hemorrhoids.[8]
- Acetaminophen can be taken 650-1000 mg every 4-6 hours, not to exceed 4 grams (0.14 oz) in a 24-hour period.
- Ibuprofen can be taken 800 mg up to 4 times per day.
- Aspirin can be taken 325-650 mg every 4 hours as needed, not to exceed 4 grams (0.14 oz) in a 24-hour period.
-
5Take a stool softener. Stool softeners can be helpful if you are experiencing constipation from your hemorrhoids. OTC stool softeners such as docusate (Colace) can be used to keep stools soft and reduce constipation and straining. You can take 100-300 mg of docusate daily for up to one week.[9]
- Do not strain when you're on the toilet. If your bowel movement doesn't occur on its own, come back later and try again.[10]
Getting Professional Medical Treatment
-
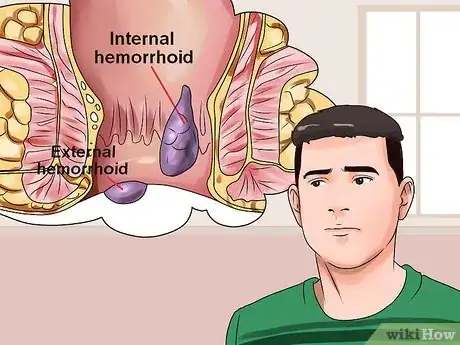
1Identify the type of hemorrhoid. Hemorrhoids can be either internal or external. Pain is most often associated with external hemorrhoids. However, you may want to see your doctor for a positive diagnosis.[11]
- Internal hemorrhoids develop in the lower rectum, and they are usually painless because the body doesn’t have any pain receptors in the rectum. You may not even know you have an internal hemorrhoid until you notice blood in your stool or the hemorrhoid prolapsing (protruding from the anus).
- If you have pain associated with your hemorrhoid, then it is likely an external hemorrhoid, which develops under the skin around the anus. If a blood clot forms inside the hemorrhoid, it is called a “thrombosed hemorrhoid,” and the pain is typically described as sudden and severe. Those afflicted might see or feel a lump in the vicinity of the anus. The clot usually dissolves and may leave a skin tag, or excess skin, in the anal area.[12]
-
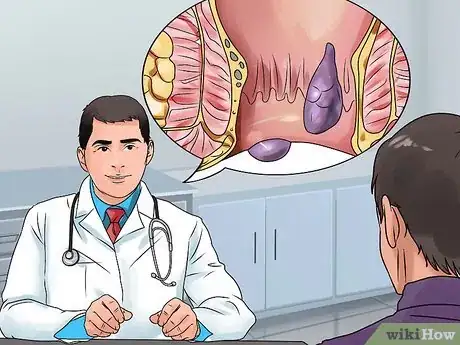
2See your doctor. Sometimes hemorrhoids will improve with home treatment methods and medical treatment will not be necessary. However, you should consult your physician if your hemorrhoid symptoms do not improve with a week of home treatments. Your doctor may discuss a number of prescription-strength or surgical options.[13]
- Sometimes hemorrhoids may linger for a long time, but if they're severe, it usually takes about 7-10 days for the pain to mostly go away.[14]
- Hemorrhoids can be caused by things like genetics, pregnancy and childbirth, or sitting on the toilet for too long.[15]
- Your doctor may advise you to make some diet and lifestyle changes before trying anything too drastic. These changes may include increasing your fiber intake and getting more exercise.
-
3Ask about prescription-strength anesthetics. If your doctor doesn’t believe a surgical option is necessary, yet he or she wants to help you with the pain associated with your hemorrhoids, he or she can provide a prescription-strength anesthetic, such as lidocaine (Xylocaine), to help deal with the discomfort and itching.[16]
-
4Discuss rubber band ligation. This is the most common procedure used to treat hemorrhoids. A small elastic band is place around the base of an internal hemorrhoid, which cuts off the circulation to the hemorrhoid. With no circulation, the hemorrhoid will shrink and wither away in a week.[17]
-
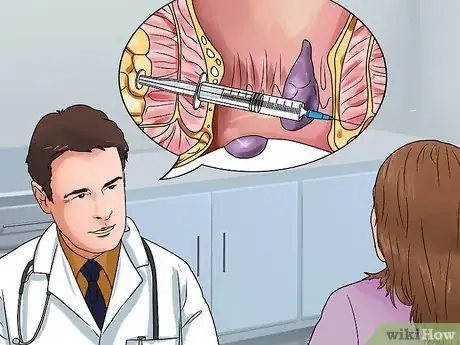
5Talk to your physician about sclerotherapy. In this procedure, a physician injects a chemical solution into the hemorrhoid, which causes scarring and shrinkage of tissue. Sclerotherapy is less effective than rubber band ligation.[18]
- Sclerotherapy, however, may not be the recommended option by a number of doctors because studies have shown that while effective in the short term, most patients develop recurrent hemorrhoids.[19]
-
6Investigate coagulation techniques. Coagulation techniques use laser, infrared light, or heat.[20] The procedures stop bleeding in small hemorrhoids and also cause them to scar and shrivel. Coagulation has higher rates of recurrence of hemorrhoids than rubber band ligation.
- This technique is often used for small hemorrhoidal tissue for which rubber band ligation is not an option, or it may be used in association with rubber band ligation as the combination of the two techniques has shown as 97 percent success rate.[21]
- This method also leads to some of the shorter recovery times for hemorrhoid surgery at one to two weeks.[22]
-
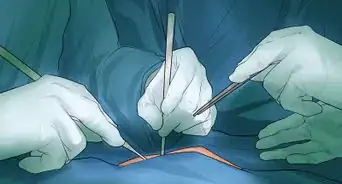
7Look into removing the hemorrhoid. This procedure is known as a hemorrhoidectomy. The offending external or internal hemorrhoid is surgically removed. It is the most effective method of treating severe or recurring hemorrhoids. It cures 95% of patients and has a low rate of complications.[23]
- This procedure is typically performed in the cases of strangulated internal hemorrhoids, mixed internal and external hemorrhoids, or preexisting anorectal conditions that necessitate surgery.[24] This option is also known for the larger degree of pain associated with the healing time.[25]
- Recovery time for removal options is approximately two to three weeks with a follow-up visit to your surgeon.
- This is typically reserved for severe cases that don't get better for a long period of time.[26]
-
8Consider hemorrhoid stapling as an option. With stapled hemorrhoidectomy (or stapled hemorrhoidopexy), a physician uses a stapling device to anchor the bleeding or prolapsed hemorrhoid in its normal position. The stapling procedure blocks the blood flow to the hemorrhoid, which causes it to shrink.[27]
- Compared to hemorrhoidectomy, stapling has a higher risk of hemorrhoid recurrence and rectal prolapse, which is when the rectum protrudes out of the anus. However, this surgical procedure is also known for its marked decrease in postoperative pain for the patient versus standard hemorrhoidectomy.[28]
Preventing Hemorrhoids
-
1Increase the amount of fiber in your diet. Increasing your fiber intake can help to prevent constipation, which is the main cause of hemorrhoids. You will find fiber in fruits, vegetables, and whole grains. The increased fiber softens the stool, which makes it easier to avoid straining with bowel movements, which is a prime cause of hemorrhoids.[29]
- The recommended daily amount of fiber varies from about 20 to 35 grams per day depending on your age and sex. Women under 51 require 25 grams per day, while women over 51 require 21 grams per day. Men under 51 require 38 grams per day, while men under 51 require 30 grams per day.[30]
- You can also supplement your fiber intake with over-the-counter fiber sources such as psyllium husk (Metamucil, Citrucel).
- Increase fiber in your diet slowly to avoid increased gas.
- If increasing you fiber intake does not help with your constipation, then you may want to consider incorporating a stool softener, such as Colace, as a short-term solution.[31]
-
2Drink more water. Staying hydrated can also help to prevent constipation. Try to drink 6 to 8 eight ounce glasses of water per day. It softens the stool and helps bowel movements pass more easily. This is especially important for individuals using fiber supplementation because not drinking enough water with increased fiber can cause constipation or make pre-existing constipation worse.[32]
-
3Exercise regularly. Regular exercise increases the motility of the bowel, which prevents constipation. It can also help an individual lose weight, which could decrease pressure in the lower rectum and anus, which is another measure for preventing hemorrhoids.[33]
- Aim for 30 minutes of exercise at least five days per week. You can divide your exercise sessions into shorter ones as well. For example, you could exercise for 15 minutes twice per day or 10 minutes three times per day if that is easier for you.[34]
- Look for an activity that you enjoy so that you will be more likely to stick with it. Try going for a walk after dinner, riding your bike to work, or taking an aerobics class a few times per week.
-
4Use the bathroom as soon as you feel the urge. Delaying bowel movements can worsen constipation, which then aggravates hemorrhoids. Try to stay close to a bathroom during your regular times for bowel movements in order to go as soon as you feel the urge.[35]
- If you cannot go to the bathroom after sitting for about five minutes, then get off of the toilet and come back later. Sitting on the toilet for long periods of time can worsen hemorrhoids.[36]
-
5Avoid sitting for long periods of time. Prolonged sitting increases the pressure in the veins of the lower rectum and anus, which can contribute to the development of hemorrhoids. Try standing up and walking around even for a few minutes whenever you take breaks at work if your job involves lots of sitting.[37]
Expert Q&A
-
QuestionWhat can cause butt pain?
 Chris M. Matsko, MDDr. Chris M. Matsko is a retired physician based in Pittsburgh, Pennsylvania. With over 25 years of medical research experience, Dr. Matsko was awarded the Pittsburgh Cornell University Leadership Award for Excellence. He holds a BS in Nutritional Science from Cornell University and an MD from the Temple University School of Medicine in 2007. Dr. Matsko earned a Research Writing Certification from the American Medical Writers Association (AMWA) in 2016 and a Medical Writing & Editing Certification from the University of Chicago in 2017.
Chris M. Matsko, MDDr. Chris M. Matsko is a retired physician based in Pittsburgh, Pennsylvania. With over 25 years of medical research experience, Dr. Matsko was awarded the Pittsburgh Cornell University Leadership Award for Excellence. He holds a BS in Nutritional Science from Cornell University and an MD from the Temple University School of Medicine in 2007. Dr. Matsko earned a Research Writing Certification from the American Medical Writers Association (AMWA) in 2016 and a Medical Writing & Editing Certification from the University of Chicago in 2017.
Family Medicine Physician Problems with hemorrhoids, or perhaps you have sciatica or some other musculoskeletal disorder that is causing you butt to hurt. I would seek out the attention of a surgeon.
Problems with hemorrhoids, or perhaps you have sciatica or some other musculoskeletal disorder that is causing you butt to hurt. I would seek out the attention of a surgeon. -
QuestionHow long does it take for hemorrhoids to go away?
 David Schechter, MDDr. David Schechter is a physician in Culver City, California. With over 25 years of experience as a family and sports medicine physician, Dr. Schechter specializes in mind-body medicine, preventive medicine, and chronic pain. Dr. Schechter received his MD from New York University and is an attending physician at Cedars-Sinai Medical Center. He was named a Top Doctor by Los Angeles Magazine and Men's Health Magazine. He has also written several books, including The MindBody Workbook.
David Schechter, MDDr. David Schechter is a physician in Culver City, California. With over 25 years of experience as a family and sports medicine physician, Dr. Schechter specializes in mind-body medicine, preventive medicine, and chronic pain. Dr. Schechter received his MD from New York University and is an attending physician at Cedars-Sinai Medical Center. He was named a Top Doctor by Los Angeles Magazine and Men's Health Magazine. He has also written several books, including The MindBody Workbook.
Family Medicine Practitioner Hemorrhoids can vary. Sometimes they linger at a low level for a long time, but if they're very severely painful, it usually takes 7-10 days for the pain to mostly go away. Occasionally, the doctor needs to do a procedure to open them up and release a clot if there's one in time, or they may do surgery if it's a very severe case that doesn't get better for a long period of time.
Hemorrhoids can vary. Sometimes they linger at a low level for a long time, but if they're very severely painful, it usually takes 7-10 days for the pain to mostly go away. Occasionally, the doctor needs to do a procedure to open them up and release a clot if there's one in time, or they may do surgery if it's a very severe case that doesn't get better for a long period of time.
Warnings
- Though this article provides information pertaining to hemorrhoids, it should not be taken as medical advice. Always consult your physician regarding the best way to treat your specific condition.⧼thumbs_response⧽
- Urgent medical evaluation should be sought by individuals who experience anorectal bleeding while on blood thinners (anticoagulants) such as warfarin (Coumadin), clopidogrel (Plavix), enoxaparin (Lovenox), rivaroxaban (Xarelto), dabigatran (Pradaxa), or apixaban (Eliquis).⧼thumbs_response⧽
- Medical care should be sought immediately if anorectal bleeding is accompanied by abdominal pain. Hemorrhoids do not cause abdominal pain.⧼thumbs_response⧽
- Anorectal bleeding with associated symptoms such as dizziness, lightheadedness, or fainting (syncope) should also be immediately evaluated. These symptoms may represent significant blood loss requiring transfusion.⧼thumbs_response⧽
- Prolapsed internal hemorrhoids that cannot be pushed back (reduced) through the anus require urgent medical attention.⧼thumbs_response⧽
- Thrombosed hemorrhoids causing excruciating pain may need medical evaluation and evacuation of the blood clot if indicated.⧼thumbs_response⧽
References
- ↑ https://medlineplus.gov/ency/article/000292.htm
- ↑ https://www.health.harvard.edu/diseases-and-conditions/hemorrhoids_and_what_to_do_about_them
- ↑ David Schechter, MD. Family Medicine Practitioner. Expert Interview. 15 July 2020.
- ↑ https://myhealth.alberta.ca/Health/aftercareinformation/pages/conditions.aspx?hwid=uf7564
- ↑ https://www.health.harvard.edu/diseases-and-conditions/hemorrhoids_and_what_to_do_about_them
- ↑ https://reference.medscape.com/drug/preparation-h-cream-maximum-strength-pain-relief-phenylephrine-pramoxine-glycerin-petrolatum-rectal-999742
- ↑ https://www.uofmhealth.org/health-library/d01303a1
- ↑ https://familydoctor.org/condition/hemorrhoids/
- ↑ https://medlineplus.gov/ency/article/000292.htm
- ↑ David Schechter, MD. Family Medicine Practitioner. Expert Interview. 15 July 2020.
- ↑ https://my.clevelandclinic.org/health/diseases/15120-hemorrhoids
- ↑ https://www.health.harvard.edu/diseases-and-conditions/hemorrhoids_and_what_to_do_about_them
- ↑ https://my.clevelandclinic.org/health/diseases/15120-hemorrhoids
- ↑ David Schechter, MD. Family Medicine Practitioner. Expert Interview. 15 July 2020.
- ↑ David Schechter, MD. Family Medicine Practitioner. Expert Interview. 15 July 2020.
- ↑ https://www.nhs.uk/medicines/lidocaine-for-piles-and-itchy-bottom/
- ↑ https://www.uofmhealth.org/health-library/hw212526
- ↑ https://www.ncbi.nlm.nih.gov/books/NBK279465/
- ↑ http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2780175/
- ↑ https://emedicine.medscape.com/article/1582358-technique#c3
- ↑ http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2780175/
- ↑ http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3786491/
- ↑ https://www.uofmhealth.org/health-library/hw212391#hw212418
- ↑ http://colorectal.surgery.ucsf.edu/conditions--procedures/hemorrhoidectomy.aspx
- ↑ http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2780175/
- ↑ David Schechter, MD. Family Medicine Practitioner. Expert Interview. 15 July 2020.
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4775568/
- ↑ http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2780175/
- ↑ https://www.niddk.nih.gov/health-information/digestive-diseases/hemorrhoids/eating-diet-nutrition
- ↑ https://www.eatright.org/food/vitamins-and-supplements/types-of-vitamins-and-nutrients/easy-ways-to-boost-fiber-in-your-daily-diet
- ↑ https://www.niddk.nih.gov/health-information/digestive-diseases/hemorrhoids/treatment
- ↑ https://health.clevelandclinic.org/5-simple-ways-you-can-prevent-hemorrhoids/
- ↑ https://health.clevelandclinic.org/5-simple-ways-you-can-prevent-hemorrhoids/
- ↑ https://www.heart.org/en/healthy-living/fitness/fitness-basics/aha-recs-for-physical-activity-in-adults?utm_source=redirect_heartorg&utm_medium=referral&utm_campaign=301
- ↑ https://health.clevelandclinic.org/5-simple-ways-you-can-prevent-hemorrhoids/
- ↑ https://my.clevelandclinic.org/health/diseases/15120-hemorrhoids
- ↑ https://familydoctor.org/condition/hemorrhoids/
About This Article
If you’re experiencing hemorrhoid pain, you can try several home treatments to relieve it. Soak the affected area in a warm bath, also known as a sitz bath, 2 to 3 times a day for 10 minutes. You can also apply ice cubes wrapped in a cloth to your anal area for 10 minutes to numb the pain and reduce swelling. Try over-the-counter pain relievers, such as Tucks pads or Preparation H cream, which you can buy from a pharmacy. Oral pain relievers, like Aspirin and Ibuprofen, can also help. If your symptoms don’t improve after a week of home treatments, see your doctor for a diagnosis. For tips from our Medical co-author on how to get your hemorrhoids removed, read on!







































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...