This article was co-authored by Allison Romero, PT, DPT. Dr. Allison Romero is a Pelvic Health Specialist, Physical Therapist, and the Owner of Reclaim Pelvic Therapy in the San Francisco Bay Area. With over a decade of experience, Allison specializes in comprehensive pelvic physical therapy treatments for pelvic floor dysfunction. She holds a Bachelor of Science in Kinesiology and Exercise Science from Sonoma State University and a Doctor of Physical Therapy from the University of Southern California. Allison is a board certified Physical Therapist in California and is a member of the American Physical Therapy Association-Section on Women’s Health and the International Pelvic Pain Society.
There are 10 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 32,396 times.
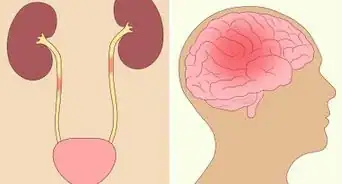
Weakness in the bladder muscles may lead to incontinence, and this can be quite frustrating. However, there are several things you can do to strengthen your bladder muscles and gain more control over when you have to urinate. Start by incorporating exercises and bladder control techniques to train your bladder. Then, make some simple lifestyle changes to improve your overall bladder health. You may also want to consult with a physician to determine what is causing your bladder control issues.
Steps
Using Exercises and Bladder Control Techniques
-
1Do kegels to strengthen the muscles that control urination.[1] A kegel is an exercise that works your pelvic floor muscles. These are the muscles that control urination, so doing kegels daily can help you to control your bladder better. To do a kegel, lift your pelvic floor muscles, hold for 5 seconds, and then relax them. Do 10 repetitions 3 times daily.[2]
- To help you locate your pelvic floor muscles, imagine the muscles you use to control the flow of urine when you're using the bathroom.[3] The muscles that control this flow are the muscles you’ll need to contract and release during kegel exercises. However, you should not do Kegels while urinating, as this can lead to a bladder infection.[4]
Tip: You might not be able to hold the kegels for the full 5 seconds at first. If needed, start by holding each kegel for 1 or 2 seconds and work up to holding them for 5 seconds.
-
2Wait 10 minutes past when you get the urge to urinate. This can be helpful if you have to urinate frequently and find it hard to wait. Wait for 10 minutes after you first get the urge to go to the bathroom and increase the amount of time you wait by 10 minutes the next time. Keep increasing the amount of time you wait to go until you’re only going to the bathroom once every 2-2.5 hours.[5]
- By increasing the amount of time that you wait, you’ll be strengthening the muscles around your bladder and training your bladder to hold onto urine for longer.
Advertisement -
3Urinate twice each time you go to the bathroom. After you finish going to the bathroom, wait for 3 minutes, and then try to urinate again. This is called double-voiding. It’s a good way to ensure that you’ve completely emptied your bladder, and it may help to promote more complete emptying in the future.[6]
Tip: Sitting in a relaxed position may make it easier to urinate. If you normally stand or hover just above the toilet seat when you urinate, sit down completely and take a few deep breaths to help yourself relax.[7]
-
4Schedule regular bathroom trips every 2 to 4 hours. Going to the bathroom on a set schedule may help to train your bladder to function better. Schedule a bathroom trip every 2 to 4 hours and stop whatever you’re doing when it’s time for you to go.[8]
- Never go more than 4 hours without urinating. Holding urine in your bladder for long periods of time can weaken it.[9] https://familydoctor.org/bladder-training-urinary-incontinence/
Promoting General Bladder Health
-
1Drink water throughout the day. It’s important to keep yourself well-hydrated to ensure good bladder health. Don’t restrict your fluid intake as a way to urinate less as this may lead to dehydration and urinary tract infections. Drink water whenever you are thirsty or sweaty, such as from warm weather or exercise.[10]
-
2Quit smoking if you’re a smoker. Smoking is harmful for many parts of your body, including your bladder. If you’re a smoker and experiencing bladder problems, talk to your doctor about options that might help you quit. They may be able to prescribe a medication, recommend nicotine replacement products, or refer you to a smoking cessation program in your area.[12]
-
3Lose weight if you’re overweight or obese. Talk to your doctor to find out if you’re at a healthy weight or see if you might need to lose weight. Even losing 5 to 10% of your body weight may improve urinary incontinence. Once you get to a healthier body weight, maintain it with a healthy diet and regular exercise.[13]
- Keep in mind that this might not work for everyone, but it may be as effective as taking a medication or using another non-surgical treatment for incontinence, so it’s worth trying.
-
4Wear cotton underwear to promote air flow. Although wearing cotton underwear won’t strengthen your bladder, it may help to reduce the chances of getting a urinary tract infection. Choose 100% cotton underwear and avoid underwear that’s made from synthetic fabrics.[14]
- Avoid clothing that fits tightly in the crotch area as well.
- If you wear pantyhose or leggings, make sure they have a cotton crotch panel.[15]
Tip: Always change your clothing after getting sweaty or wet, such as after exercising or swimming. Take a shower, dry yourself off thoroughly, and put on clean, dry clothing and underwear. This may help to prevent urinary tract infections.[16]
Seeking Medical Treatment for Incontinence
-
1Make an appointment to see your doctor if you have concerns. If you’re having bladder control issues, make an appointment to see a doctor. There are different potential causes of bladder control problems, so your doctor will need to run tests to find out what’s causing your issues.[17] Some diagnostic tests your doctor might use include:[18]
- Running a urinalysis test to check for infection, blood, and other abnormalities in your urine.
- Having you keep a bladder diary to look for patterns in your urinary habits.
- Using an ultrasound or catheter to check the amount of urine in your bladder after you urinate.
Tip: Make sure to tell your doctor about any other symptoms you are having along with loss of bladder control.
-
2Ask your doctor about medications for incontinence. Depending on the type of incontinence you have, your doctor might recommend a medication to treat the problem. There are different types of medications available including:[19]
- Anticholinergics. These medications are helpful for calming an overactive bladder. This is a common issue with urge incontinence, which is when you frequently get the urge to urinate.
- Mirabegron. This medication makes it possible for your bladder to hold more urine at once, which may be helpful for urge incontinence.
- Alpha blockers (for men with overflow incontinence). These medications help to relax the muscles in the neck of the bladder and make it easier to fully empty it when you urinate.
- Topical estrogen (for women). This may help to stimulate tissue toning and rejuvenation in the vagina.
-
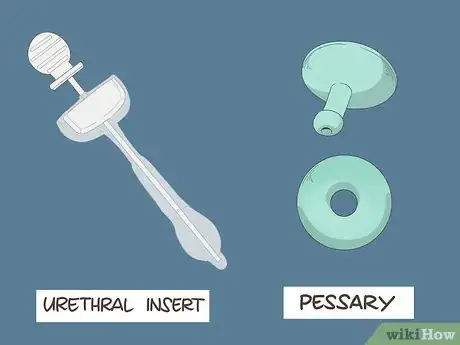
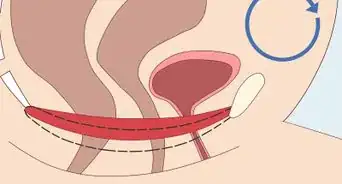
3Look into insertable devices if you’re a woman. There are a couple of devices that are available for treating incontinence in women. If you decide to use one of these, you’ll need to insert it into your urethra or vagina each day, similar to how you’d insert a tampon. The devices available include:[20]
- Urethral insert. This is a small plug-like device that you put into your urethra before engaging in an activity that might trigger incontinence, such as playing a sport. Then, you remove the device right before you have to urinate.
- Pessary. This is a stiff ring that you insert into your vagina and wear all day long. It can help to support your bladder and prevent leaks, which may be helpful if you’ve had a bladder prolapse.
-
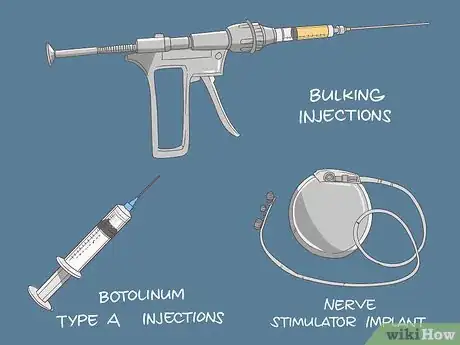
4Discuss injections and implants if medications don’t help. Injections and implants are more invasive than some other types of treatments for incontinence, but they’re less invasive than surgery. If you are still experiencing issues after trying lifestyle modifications and medications, talk to your doctor about injections and implants to treat incontinence. Some options to consider include:[21]
- Bulking injections. In this treatment, a synthetic material is injected into your urethra to help keep it closed and prevent leaks.
- Botulinum toxin type A injections. These injections might be helpful if you have an overactive bladder. The botulinum toxin helps the bladder’s sphincter relax and reduces frequent urges to go.[22]
- Nerve stimulator implant. This device goes under the skin near your bladder and it sends out painless electrical impulses—similar to a pacemaker—that may help to control urge incontinence.
-
5Ask about surgical treatment options if other treatments fail. Surgery is usually the last resort for incontinence treatment if other less invasive treatments have failed. However, there are effective surgical options that may help control your bladder. Some procedures to discuss with your doctor include:[23]
- Sling procedures, which use your own body tissue, a synthetic material, or mesh to support the urethra and bladder neck. This may help keep the urethra closed when you do something that might cause a leak, such as sneezing or exercising.
- Bladder neck suspension, which is another way of supporting the bladder neck and urethra to help prevent stress incontinence.
- Prolapse surgery, which is more common for women. This procedure may be recommended if the bladder has lost its support. The surgeon uses body tissue or mesh to reinforce it.
- Artificial urinary sphincter, which is when your doctor replaces your urinary sphincter with an artificial one to provide more control. After the surgery, you’ll press a valve located under your skin each time you need to urinate and it will open the sphincter and release the urine.
Expert Q&A
Did you know you can get expert answers for this article?
Unlock expert answers by supporting wikiHow
-
QuestionWhat causes weak bladder muscles?
 Allison Romero, PT, DPTDr. Allison Romero is a Pelvic Health Specialist, Physical Therapist, and the Owner of Reclaim Pelvic Therapy in the San Francisco Bay Area. With over a decade of experience, Allison specializes in comprehensive pelvic physical therapy treatments for pelvic floor dysfunction. She holds a Bachelor of Science in Kinesiology and Exercise Science from Sonoma State University and a Doctor of Physical Therapy from the University of Southern California. Allison is a board certified Physical Therapist in California and is a member of the American Physical Therapy Association-Section on Women’s Health and the International Pelvic Pain Society.
Allison Romero, PT, DPTDr. Allison Romero is a Pelvic Health Specialist, Physical Therapist, and the Owner of Reclaim Pelvic Therapy in the San Francisco Bay Area. With over a decade of experience, Allison specializes in comprehensive pelvic physical therapy treatments for pelvic floor dysfunction. She holds a Bachelor of Science in Kinesiology and Exercise Science from Sonoma State University and a Doctor of Physical Therapy from the University of Southern California. Allison is a board certified Physical Therapist in California and is a member of the American Physical Therapy Association-Section on Women’s Health and the International Pelvic Pain Society.
Pelvic Health Specialist
Warnings
- Don’t restrict your fluid intake to prevent incontinence. This can lead to dehydration and urinary tract infections.⧼thumbs_response⧽
References
- ↑ Allison Romero, PT, DPT. Pelvic Health Specialist. Expert Interview. 2 December 2020.
- ↑ Allison Romero, PT, DPT. Pelvic Health Specialist. Expert Interview. 2 December 2020.
- ↑ Allison Romero, PT, DPT. Pelvic Health Specialist. Expert Interview. 2 December 2020.
- ↑ Allison Romero, PT, DPT. Pelvic Health Specialist. Expert Interview. 2 December 2020.
- ↑ https://www.ouh.nhs.uk/patient-guide/leaflets/files/65610Poveractivebladder.pdf
- ↑ https://www.urologyhealth.org/overactive-bladder
- ↑ https://www.nia.nih.gov/health/13-tips-keep-your-bladder-healthy
- ↑ https://familydoctor.org/bladder-training-urinary-incontinence/
- ↑ https://www.nia.nih.gov/health/13-tips-keep-your-bladder-healthy
- ↑ https://www.nia.nih.gov/health/13-tips-keep-your-bladder-healthy
- ↑ https://www.ouh.nhs.uk/patient-guide/leaflets/files/65610Poveractivebladder.pdf
- ↑ https://www.nia.nih.gov/health/13-tips-keep-your-bladder-healthy
- ↑ https://www.ncbi.nlm.nih.gov/pubmed/15947625
- ↑ https://www.nia.nih.gov/health/13-tips-keep-your-bladder-healthy
- ↑ https://journals.lww.com/nursing/fulltext/2003/06000/stop_utis_in_their_tracts.26.aspx
- ↑ https://journals.lww.com/nursing/fulltext/2003/06000/stop_utis_in_their_tracts.26.aspx
- ↑ Allison Romero, PT, DPT. Pelvic Health Specialist. Expert Interview. 2 December 2020.
- ↑ https://patient.info/womens-health/lower-urinary-tract-symptoms-in-women-luts/overactive-bladder-syndrome-oab
- ↑ https://patient.info/womens-health/lower-urinary-tract-symptoms-in-women-luts/overactive-bladder-syndrome-oab
- ↑ https://www.nhs.uk/conditions/urinary-incontinence/treatment/
- ↑ https://patient.info/womens-health/lower-urinary-tract-symptoms-in-women-luts/overactive-bladder-syndrome-oab
- ↑ https://www.bladderandbowel.org/surgical-treatment/botulinum-toxin/
- ↑ https://patient.info/womens-health/lower-urinary-tract-symptoms-in-women-luts/overactive-bladder-syndrome-oab

































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...