This article was medically reviewed by Sarah Gehrke, RN, MS and by wikiHow staff writer, Christopher M. Osborne, PhD. Sarah Gehrke is a Registered Nurse and Licensed Massage Therapist in Texas. Sarah has over 10 years of experience teaching and practicing phlebotomy and intravenous (IV) therapy using physical, psychological, and emotional support. She received her Massage Therapist License from the Amarillo Massage Therapy Institute in 2008 and a M.S. in Nursing from the University of Phoenix in 2013.
There are 7 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 18,117 times.
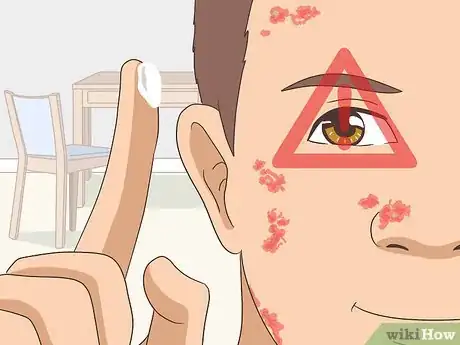
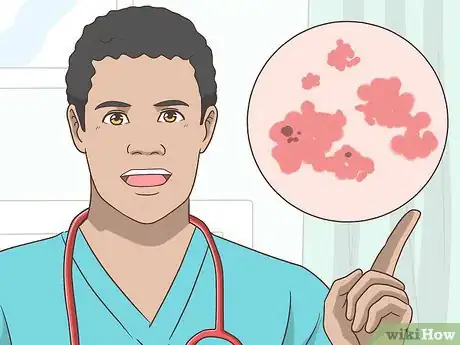
Actinic keratosis (AK), caused by long-term sun exposure and tanning bed use, presents as one or more rough, scaly patches (AKs) on your skin. Because a small percentage of AKs develop into a form of skin cancer (squamous cell carcinoma), dermatologists typically treat any AKs they find on you.[1] Often, they’ll combine targeted removal treatments for AKs with broad-based therapies to combat the condition.
Steps
Targeting a Single AK
-
1Choose a skilled and experienced dermatologist. When removing a single AK lesion with cryosurgery, curettage and desiccation, or laser therapy, the skill of the dermatologist is paramount in determining the results. Seek referrals from your doctor and your friends, research the qualifications of potential choices, and meet with dermatologists before choosing one.
- These three techniques can have 5-year cure rates of over 95% when done by a skilled dermatologist (“cure” here means the same AK doesn’t return).[2]
-
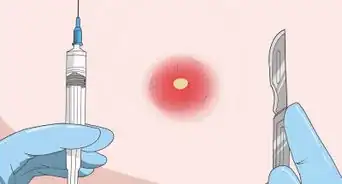
2Freeze away an AK with cryosurgery. With this method, your dermatologist will apply liquid nitrogen to the AK. The extreme cold will destroy the targeted cells, and the AK will typically blister or crust over and fall off within several days.[3]
- The liquid nitrogen might be sprayed on with a cryogun or applied directly with a cotton swab.[4]
- Cryosurgery is quick, comparatively affordable, and rarely causes side effects outside the targeted area.
Advertisement -
3Physically remove an AK via curettage and desiccation. For this method, your dermatologist will scrape, shave, or cut away the lesion. Then they will use heat, electricity, or chemicals to cauterize the wound and kill off any AK cells left behind in that spot.[5]
- This method is often used for deep-rooted AKs, or when hair follicles are in the way.[6]
- It is quick and fairly affordable like cryosurgery, but carries a somewhat greater risk of localized pain and scarring.
-
4Vaporize an AK with laser surgery. In this technique, the dermatologist aims an intense beam of light at the AK. This laser beam destroys the AK cells immediately.[7]
- Laser therapy may be less widely available than cryosurgery or curettage and desiccation, and may be more costly.
Addressing Multiple AKs
-
1Apply prescription topical creams as directed. It’s common to have several AKs clustered in an area that’s been exposed to years of sunlight, like your ears, nose, scalp, or forearms. In these cases, topical creams are often the first choice for eliminating the AKs. These include:[8]
- 5-fluorouracil, which is often applied 1-2 times daily for 3-4 weeks.
- Imiquimod, which is often used twice a week, or daily for alternating weeks, for 16 weeks.
- Diclofenac, which typically is applied nightly for 2-3 months.
- Ingenol, which you apply daily for only 2-3 days.
-
2Follow your instructions and watch for side effects. Don't allow any type of AK topical cream to get into your eyes. You also need to severely limit your exposure to UV radiation (sunlight) and wash your hands after application. If you have widespread AKs, your dermatologist will also likely limit your treatment to a single area, in order to check for negative reactions.[9]
- Topical treatments can cause irritation, redness, peeling, scaling, or scarring. Talk to your dermatologist about what to expect, and contact them if you experience unexpected pain or discomfort.[10]
- Imiquimod can also rarely cause flu-like symptoms, and diclofenac should be avoided by those with aspirin or NSAID allergies.
-
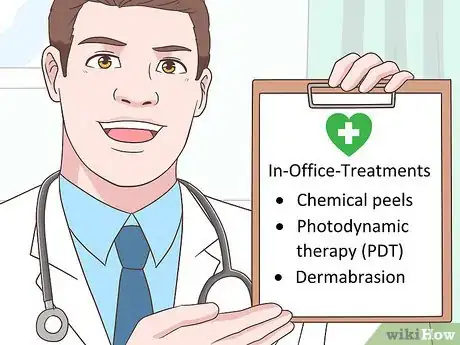
3Peel away or eradicate widespread AKs. Instead of (or in addition to) applying topical treatments at home, your dermatologist might recommend undergoing in-office treatments over the affected area(s). These include:[11]
- Chemical peels, which cause the top layers of your skin to slough off. This is most effective for AKs that aren’t deep-rooted. These can cause pain, redness, and stinging.
- Photodynamic therapy (PDT), in which a light-sensitive cream is applied to the AKs, followed by an intense light that kills the AKs. This can also cause pain and stinging, and you must avoid sunlight for at least 1-2 days afterward.
- Dermabrasion, in which healthy skin and the AKs alike are essentially “sanded off” by your dermatologist. This causes pain, redness, and bleeding, and the overall effects on fully eliminating AKs are unclear.[12]
-
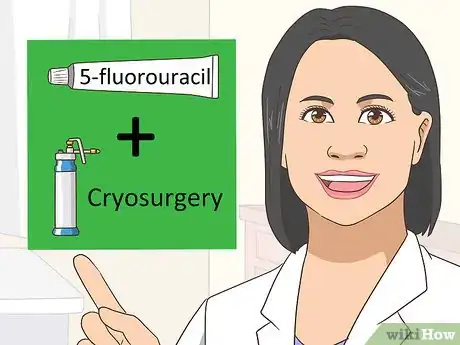
4Consider combining AK therapies. Say, for instance, you have one substantial AK and several smaller ones on the back of your neck. Your dermatologist might recommend a course of 5-fluorouracil followed by cryosurgery, or PDT followed by a course of imiquimod.[13]
- There is evidence that some 2-therapy combinations increase the 5-year cure rate for AKs beyond that of either therapy alone.[14]
- However, combined therapies are also more costly, and can cause a greater range of side effects.
Preventing and Limiting AKs
-
1Wear sunscreen every day. Even if it’s a cloudy winter day, you should apply a broad-spectrum, SPF-30 or greater sunscreen to all exposed skin (and skin that is covered only by lightweight clothing). Also apply a lip balm with the same sunscreen properties.[15]
- If you already have AKs, talk to your dermatologist about the best sunscreen options for you.
- Skin protection measures like these can help you avoid AKs in the first place, and can also limit the growth of additional AKs or the expansion of existing ones.
-
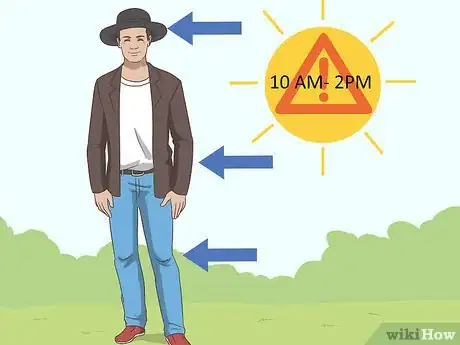
2Limit your skin’s exposure to direct sunlight. Try to avoid the mid-day sun (between 10 am and 2 pm) whenever possible. When you do go out in the sun, wear a broad-brimmed hat, pants, and long sleeves.[16]
- Not all clothes are created equal, though. If you hold a shirt in front of a bright light and the light shines through, the shirt won’t give you full sun protection. You’ll have to wear sunscreen underneath your shirt as well.
-
3See a dermatologist right away if you suspect AKs. Assume you have an AK if you can feel a rough, scaly patch on your skin in an area that has gotten lots of sunlight over the years. The patch may be pink or brown, or it may not be visible at all. It might also flake off and then reappear a few days or weeks later.[17]
- Only a small percentage of AKs develop into skin cancer, but prompt treatment of AKs reduces this percentage to virtually zero.
-
4See your dermatologist regularly if you have AKs. Once you’ve been diagnosed with one or more AKs, you should have regular checkups with your dermatologist. They may want to see you at least once or twice per year, for instance. This way, new or recurring AKs can be detected and treated early.[18]
- Even with proper treatment and sun protection measures, you may continue to develop AKs for the rest of your life. These should always be treated promptly.
References
- ↑ Uhlenhake EE. Optimal treatment of actinic keratoses. Clinical Interventions in Aging. 2013;8:29-35. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3549675/
- ↑ Uhlenhake EE. Optimal treatment of actinic keratoses. Clinical Interventions in Aging. 2013;8:29-35. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3549675/
- ↑ https://www.skincancer.org/skin-cancer-information/actinic-keratosis/actinic-keratosis-treatment-options
- ↑ Uhlenhake EE. Optimal treatment of actinic keratoses. Clinical Interventions in Aging. 2013;8:29-35. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3549675/
- ↑ https://www.skincancer.org/skin-cancer-information/actinic-keratosis/actinic-keratosis-treatment-options
- ↑ Uhlenhake EE. Optimal treatment of actinic keratoses. Clinical Interventions in Aging. 2013;8:29-35. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3549675/
- ↑ https://www.skincancer.org/skin-cancer-information/actinic-keratosis/actinic-keratosis-treatment-options
- ↑ Uhlenhake EE. Optimal treatment of actinic keratoses. Clinical Interventions in Aging. 2013;8:29-35, Table 1. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3549675/table/t1-cia-8-029/
- ↑ Uhlenhake EE. Optimal treatment of actinic keratoses. Clinical Interventions in Aging. 2013;8:29-35. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3549675/
- ↑ Uhlenhake EE. Optimal treatment of actinic keratoses. Clinical Interventions in Aging. 2013;8:29-35, Table 1. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3549675/table/t1-cia-8-029/
- ↑ https://www.skincancer.org/skin-cancer-information/actinic-keratosis/actinic-keratosis-treatment-options
- ↑ Uhlenhake EE. Optimal treatment of actinic keratoses. Clinical Interventions in Aging. 2013;8:29-35, Table 1. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3549675/table/t1-cia-8-029/
- ↑ https://www.skincancer.org/skin-cancer-information/actinic-keratosis/actinic-keratosis-treatment-options
- ↑ Uhlenhake EE. Optimal treatment of actinic keratoses. Clinical Interventions in Aging. 2013;8:29-35. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3549675/
- ↑ https://www.aad.org/public/diseases/skin-cancer/actinic-keratosis-self-care
- ↑ https://www.aad.org/public/diseases/scaly-skin/actinic-keratosis#tips
- ↑ https://www.aad.org/public/diseases/scaly-skin/actinic-keratosis#symptoms
- ↑ https://www.aad.org/public/diseases/scaly-skin/actinic-keratosis#tips
- ↑ https://www.skincancer.org/skin-cancer-information/actinic-keratosis
































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...