This article was medically reviewed by Erik Kramer, DO, MPH. Dr. Erik Kramer is a Board-Certified Primary Care Physician at the University of Colorado. With over 15 years of experience, his clinical interests include obesity and weight management, diabetes care, and preventive care, as well as embracing a holistic approach to primary care. He received his Doctorate in Osteopathic Medicine (D.O.) from the Touro University Nevada College of Osteopathic Medicine and completed his residency at Central Maine Medical Center. Dr. Kramer is a Diplomate of the American Board of Obesity Medicine.
There are 15 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 24,656 times.
People with diabetes often have problems with their feet, and a common issue is itchiness. The typical causes of itchy feet for people with diabetes are dry skin, fungal infections, and poor circulation. Fortunately, you can relieve the itchiness, regardless of the cause, in a few simple steps.
Steps
Moisturizing Dry Skin
-
1Check if you have dry, cracked skin. In many cases, the root of itchy feet is overly dry skin. Inspect your feet and see if your skin is flaky or cracked. Also rub them and see if they feel rough. These symptoms indicate overly dry skin, which is probably the cause of your itching.[1]
- If your skin is cracked enough that your feet bleed, see your doctor right away. This can lead to a serious infection for someone with diabetes.
-
2Avoid scratching your feet. While it may be tempting, scratching your itchy feet can do more damage. If your skin is dry, it cracks more easily, so you can cut yourself if you scratch too hard. Even small cuts can get infected when you have diabetes.[2]
- If you have been scratching and there are cuts on your feet, visit your doctor right away.
Advertisement -
3Wash your feet daily with lukewarm water. Keeping your feet clean helps avoid dry skin. When you wash your feet, use only lukewarm water. Hot water can irritate your skin and cause further itching. Always test the water with your hand before washing your feet. If you can’t keep your hand in the water because it’s too hot, either wait for the water to cool down or turn the hot water down.[3]
- As a general guideline, use water that is the same temperature you would use on a newborn baby.
- When washing, use a soft sponge or washcloth. Don’t rub your feet hard because this can cause further irritation.
-
4Use hypoallergenic and fragrance-free soap when you wash your feet. Perfumes, fragrances, dyes, and harsh soaps can cause reactions on your skin. When you wash, use only hypoallergenic and fragrance-free soaps that are gentle on your skin.[4]
- Do not take bubble baths. These chemicals can dry out your skin further.
- If you need guidance on buying skincare products, ask your doctor for suggestions.
-
5Blot your feet dry with a towel after washing them. Make sure they are completely dry by gently blotting them with a towel. Do not rub, because this can irritate your skin. Do not get dressed until your skin is dry because your clothes can trap moisture, especially in humid weather.[5]
- Remember to dry in between your toes. Moisture here can cause fungal infections.
-
6Apply a gentle moisturizer to your feet daily. Moisturizers help prevent dry, itchy skin. Use a fragrance-free moisturizer after washing your feet to prevent your skin from drying out. Follow the application instructions on the product packaging.[6]
- Do not apply any cream between your toes. The extra moisture can encourage fungal growth.
-
7Wear socks designed for people with diabetes. These socks are designed with extra cushioning and moisture-wicking material. They keep your feet dry and help prevent skin irritations.[7]
- If you don’t wear specialized socks, make sure you change into clean, dry socks every day.
-
8Drink the daily recommended amount of water. Staying hydrated helps keep your skin moist and healthy. Prevent dryness and cracking by drinking water regularly throughout the day.[8]
- The daily recommended amount of water 15.5 cups (3.7 liters) for men and 11.5 cups (2.7 liters) for women. Use this as a guideline for your daily intake.[9]
Treating Fungal Infections
-
1Look for rashes or bumps indicating an infection. Diabetes leaves your feet susceptible to bacterial or fungal infections that may cause itching. Inspect your feet for any red patches. These may be raised or bumpy. Blistered skin is also a symptom of a fungal infection. If these signs are present on your feet, the itching may be from some kind of infection.[10]
- Remember to check between your toes. Some fungal infections like athlete’s foot primarily grow in between the toes.
Tip: A rash that's accompanied by swelling, dry skin, and possibly scaling may be caused by venous insufficiency, which means your veins in your legs aren't working well. Visit your doctor to make sure you're okay.
-
2Contact your doctor if you think you have a fungal infection. Most fungal infections are harmless and only cause itching, but someone with diabetes is at risk for further infections. If you inspect your feet and find signs of a fungal infection like red skin or blisters, contact your doctor right away. They will advise you best on how to proceed.[11]
- If you're having recurring fungal infections, it might be a sign of worsening uncontrolled blood sugar or undiagnosed diabetes. Getting your blood sugar under control can help prevent these infections.
-
3Apply antifungal cream to your feet. If your doctor inspects your feet and diagnoses you with a fungal infection, the first step will probably be applying antifungal cream to the area. Your doctor may recommend an over the counter product or write you a prescription for a stronger medication.[12]
- Follow all the instructions that your doctor gives you on using the cream properly.
- Common application instructions include washing and drying your feet completely, then applying the cream to the affected area twice a day.
-
4Keep the humidity low in your home. Fungal infections grow in damp environments. If you live in a humid area, your skin will stay wet if you sweat or bathe. Use a dehumidifier to keep your home’s humidity low. This can prevent fungal infections and stop existing ones from spreading.[13]
- If you don’t keep the humidity low in your home all the time, at least turn on the dehumidifier when you bathe, or only bathe when humidity is low. If humidity is high, your body will take a long time to dry. This could encourage fungal growth.
-
5Use an antiperspirant on the bottom of your feet. If you have a problem with sweaty feet, you may be more susceptible to fungal infections. Prevent this problem by applying an antiperspirant to the soles of your feet. Make sure the product you use is fragrance-free and hypoallergenic.[14]
- Check with your doctor before doing this. An antiperspirant may interact with other products you use on your feet.
-
6Wear clean socks every day. Fungal infections can remain in your socks and re-infect you when you put them back on. Avoid this possibility by wearing clean, dry socks every day. Always wash your socks thoroughly before wearing them again.[15]
- Specialized socks for people with diabetes may also help prevent fungal infections. These socks are designed with moisture-wicking material that keeps your feet dry.
Improving Circulation to Your Feet
-
1Inspect your feet for symptoms of poor circulation. Sometimes itching is caused by poor blood circulation, a common problem for people with diabetes. If the itching is accompanied by any of the following symptoms, poor circulation is probably the cause.[16]
- A pale blue color in your feet or lower legs.
- Numbness or tingling.
- Your feet feeling cold to the touch.
- Your calves feel painful while you're active and feel better at rest.
Warning: In some cases, poor circulation might be a sign of peripheral artery disease. Diabetes is a risk factor for this condition, so it's important that you talk to your doctor about what you're experiencing so you can get treatment.
-
2Get at least 30 minutes of physical activity 5 days per week. When poor circulation is the cause of your itching feet, you can take several actions to improve circulation. An important one in staying active. When you're sedentary, blood doesn't travel as well. Fix this by getting the recommended 30 minutes per day of physical activity. This can bring more blood to your feet and help the itching.[17]
- You can break this exercise up into several sets throughout the day. For example, you could take a 10-minute walk in the morning and go for a 20 minute run in the evening.[18]
- You don't have to work out hard to meet this goal. Walking for a few minutes a day is a perfect exercise.
- If you haven't exercised in a while, start off small. Go for a 5-minute walk each day for a week. Then increase the time by 5 minutes every week.
-
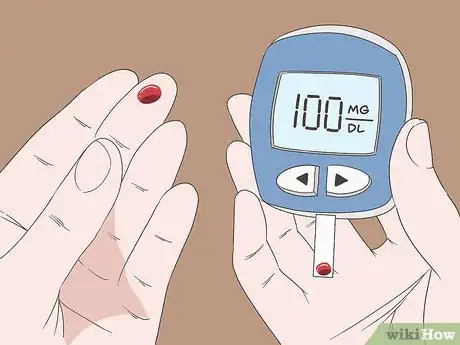
3Keep your blood sugar levels within the normal range. An abnormal blood sugar level can cause poor circulation. Do your best to manage your diabetes symptoms and maintain a normal blood sugar range. A normal range is usually between 70-100 mg/dl (4 and 9 mmol/L) or an A1C less than 5.7%, depending on the type of diabetes you have.[19]
- Diabetes patients can maintain a normal blood sugar range by taking their medication and eating 3 balanced meals a day. You should also avoid sugary food and drinks like soda.
- Also limit your alcohol intake. Speak with your doctor about drinking alcohol, because this can affect your blood sugar as well.
-
4Maintain a healthy cholesterol level. High cholesterol can also inhibit your body's circulation. Consult with your doctor to find the right cholesterol level for you. If your cholesterol is high, take steps to meet and maintain this level to improve your circulation.[20]
- You can reduce your cholesterol by eating less saturated fats, eating more polyunsaturated fats, and exercising regularly.
- Your doctor may prescribe medication to reduce your cholesterol as well.
References
- ↑ https://my.clevelandclinic.org/health/diseases/9492-diabetes-foot--skin-related-complications
- ↑ https://www.diabetes.org/diabetes/skin-complications
- ↑ https://www.foothealthfacts.org/conditions/diabetic-foot-care-guidelines
- ↑ https://my.clevelandclinic.org/health/articles/9491-diabetes-skin-care
- ↑ https://my.clevelandclinic.org/health/articles/9491-diabetes-skin-care
- ↑ https://www.foothealthfacts.org/conditions/diabetic-foot-care-guidelines
- ↑ https://www.foothealthfacts.org/conditions/diabetic-foot-care-guidelines
- ↑ https://my.clevelandclinic.org/health/articles/9491-diabetes-skin-care
- ↑ https://health.clevelandclinic.org/how-much-water-do-you-need-daily/
- ↑ https://my.clevelandclinic.org/health/diseases/9492-diabetes-foot--skin-related-complications
- ↑ https://www.diabetes.org/diabetes/complications/skin-complications
- ↑ https://my.clevelandclinic.org/health/diseases/9492-diabetes-foot--skin-related-complications
- ↑ https://my.clevelandclinic.org/health/articles/12176-diabetes-skin-conditions
- ↑ https://www.foothealthfacts.org/conditions/diabetic-foot-care-guidelines
- ↑ https://www.foothealthfacts.org/conditions/diabetic-foot-care-guidelines
- ↑ https://my.clevelandclinic.org/health/diseases/21882-poor-circulation
- ↑ https://www.niddk.nih.gov/health-information/diabetes/overview/preventing-problems/foot-problems
- ↑ https://my.clevelandclinic.org/health/articles/7050-aerobic-exercise
- ↑ https://www.cdc.gov/diabetes/managing/manage-blood-sugar.html
- ↑ https://www.niddk.nih.gov/health-information/diabetes/overview/managing-diabetes











































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...