This article was medically reviewed by Sarah Gehrke, RN, MS. Sarah Gehrke is a Registered Nurse and Licensed Massage Therapist in Texas. Sarah has over 10 years of experience teaching and practicing phlebotomy and intravenous (IV) therapy using physical, psychological, and emotional support. She received her Massage Therapist License from the Amarillo Massage Therapy Institute in 2008 and a M.S. in Nursing from the University of Phoenix in 2013.
There are 14 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 15,518 times.
Learning that you have kidney failure is scary and confusing. While you’ll have to adjust to new routines, living a long, fulfilling life is possible with proper treatment. Acute kidney failure is usually caused by an underlying condition, such as an injury or infection. It can be temporary, depending on how much damage your kidney has, and kidney function often returns after treating the underlying cause. You’ll need regular dialysis if you have end-stage renal disease or chronic kidney disease. If you’re healthy enough for transplant surgery, visit a transplant center to get on a waitlist or discuss donor options with your family.
Steps
Treating Acute Kidney Failure
-
1Get immediate help if you experience symptoms. Acute kidney failure is usually diagnosed in people who are already hospitalized. However, if you’re not in the hospital, have a common underlying cause of kidney failure, and experience symptoms, you’ll need to see a doctor immediately.[1]
- Common causes of acute kidney failure include injury, blood clots, urethral blockages, severe dehydration, drug overdose, alcohol abuse, and infection.
- Symptoms of kidney failure include urination changes (such as producing little or no urine), fatigue or sluggish movements, metallic taste in your mouth, pain between your ribs and hips, seizures, and swelling due to water retention, especially in your legs, ankles and feet.
-
2Start treatment for the underlying cause. Your doctor will need to perform tests to diagnose the underlying cause.[2] They’ll then clear a blockage or clot, administer antibiotics, or take other steps to treat the underlying condition.
- While treating the underlying cause, you’ll receive medication to help control your fluid levels and blood potassium.
Advertisement -
3Make kidney-friendly dietary changes. During and after treatment, you’ll need to eat more healthy carbohydrates, such as fruits and vegetables. You’ll also need to limit the amounts of protein, salt, and potassium in your diet.[3]
- High-protein foods include red meat, poultry, and eggs. Instead of these, you’d need to eat more fruits, vegetables, and foods that are high in fiber, like brown rice, lentils, and raspberries. [4]
- You’ll also need to swap high-potassium foods, such as bananas, oranges, and potatoes, for low-potassium options, such as apples, cabbage, grapes, green beans, and strawberries.[5]
- Always read the label on prepackaged and processed foods to make sure you’re not eating things with high amounts of sodium.
-
4Ask your doctor if you need dialysis. Some people who experience acute kidney failure require dialysis, which is a procedure that filters blood when your kidneys can’t function. It’s often only temporary, but cases of severe kidney damage might require long-term dialysis.[6]
Starting Dialysis
-
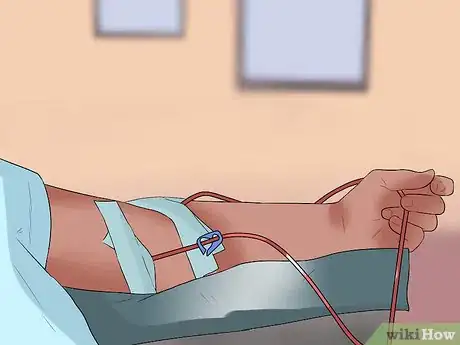
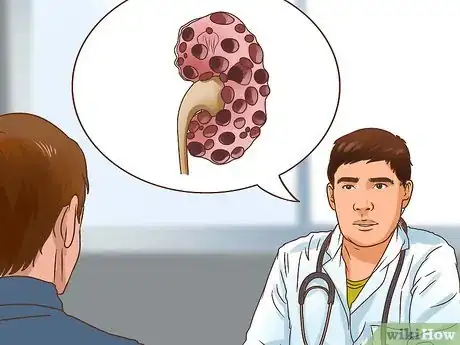
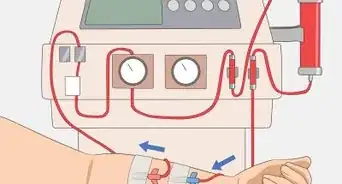
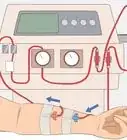
1Discuss dialysis options with your doctor. There are 2 types of dialysis, and your doctor will help you decide which option is best.[7]
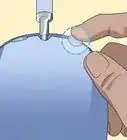
- In hemodialysis, blood is pumped through a filtration machine. You can get hemodialysis at a dialysis center or learn to do it at home. Your doctor will need to implant a fistula in your arm, which is a passage that allows blood to pass to the machine.[8]
- In peritoneal dialysis, a machine pumps a cleansing fluid into your belly, then pumps the fluid out after the filtration process is finished. Peritoneal dialysis is usually administered at home. Your doctor will need to place a catheter in your belly to allow for the fluid exchange.[9]
- The filtration process can take several hours. Depending on the type of dialysis, you’ll need it several times a week or every day. Typically, hemodialysis occurs 3 to 5 times per week. Peritoneal dialysis is often administered daily.
-
2Apply for Medicare if you live in the US and are uninsured. Dialysis is expensive but, in the United States, all dialysis patients qualify for Medicare. Medicare will pay for 80 percent of your dialysis costs. You’ll need to pay for the rest out of pocket or through private insurance.[10]
- If you have trouble covering the remainder of dialysis expenses, you can apply for financial aid through the American Kidney Fund: http://www.kidneyfund.org/financial-assistance/.
-
3Get training if you choose home dialysis. In order to do dialysis at home, you and a friend or family member need to complete a training program, which takes several weeks. You’ll visit a dialysis center and learn how to safely perform hemodialysis or peritoneal dialysis. Your center will continue to offer support, maintain equipment, and follow your care.[11]
- Home dialysis is convenient, but can be more expensive. Additionally, in the event of a complication, such as an air bubble or bleeding, you won’t have trained professionals present who can quickly respond.
-
4Go to a dialysis center if you want a medical professional present. You’ll have less flexibility if you go to a dialysis center. Depending on how you respond to treatments, you might need someone to drive you home. However, you’ll have trained professionals on duty who can respond to any complications.[12]
- Some people also find it helpful to talk to other patients at dialysis centers. Sharing your experiences with someone in similar circumstances might help you adjust.
-
5Maintain a kidney-friendly diet. A dietitian on staff at your dialysis center will help you develop a kidney-friendly meal plan. You’ll need to stick to your diet for as long as you undergo dialysis. A kidney-friendly diet consists of:[13]
- Healthy carbohydrates (fruits, veggies, and whole-grain pasta) instead of proteins (red meat, poultry, and eggs)
- Low-potassium foods (apples, grapes, and green beans) instead of high-potassium foods (bananas, oranges, and potatoes)
- Lower sodium and fat consumption
- Smaller portion sizes
Getting a Kidney Transplant
-
1Ask your doctor for a referral to a local transplant center. In order to get a transplant, you’ll need to undergo medical and psychological evaluations at a transplant center. Ask your doctor for information about your local transplant center.[14]
- You can also track one down on the Organ Procurement and Transplantation Network: https://optn.transplant.hrsa.gov/members/member-directory. Select “Transplant Centers by Organ” and “Kidney,” then select your state or region.
-
2Visit the center for a medical evaluation. When you go to the center, doctors will perform a physical exam and administer tests to determine if you’re a transplant candidate. They need to make sure you’re healthy enough for transplant surgery and recovery.[15]
- You might be ineligible if you have serious heart disease, cancer, or a chronic infection, or if you smoke.
- If you’re a transplant candidate, you’ll be added to a waitlist. Wait times depend on numerous factors, but the average wait is 3 to 5 years.[16]
-
3Discuss living donor options with your family. In addition to getting on a transplant waitlist, you could discuss your situation with someone in your family. Tell them about your medical condition, mention that you’re on dialysis, and that your long-term goal is to find a donor.[17]
- Instead of asking someone point blank, it’s usually best to share your story, educate your loved ones about your condition, and allow them to volunteer to be a donor.
- If a friend or family member volunteers to be a donor, you’ll both need to be evaluated for compatibility.
-
4Review your transplant center’s procedures if you’re on a waitlist. If you’re on a waitlist, the transplant center could call you about an organ match at any time. You’d need to get to the designated hospital as soon as possible, so make sure you know exactly what to do in the event you get the call.[18]
- Every center has its own procedure, so review the steps you’d need to take with them. Make sure you know which hospital will perform the procedure, how quickly you’ll need to arrive, and what you’ll need to bring.
-
5Schedule and undergo surgery when you have a donor. If you have a living donor, schedule the surgery at a date convenient for both of you. Surgery takes about 4 hours, and you’ll recover in the hospital for up to a week.[19]
- Doctors will monitor you to make sure your body doesn’t reject the new kidney.
-
6Take immunosuppressants and other prescribed medications. You’ll need to take immunosuppressants, or anti-rejection medicine, for as long as you have the new kidney. These will help prevent your body from rejecting the new organ. Take these and any other prescribed medications according to your doctor’s instructions.[20]
- Since your immune system will be suppressed, you’ll be at a higher risk of getting sick. Handwashing and good hygiene are essential, and you should try to stay away from sick people.
-
7Maintain a low-fat, low-salt diet. Dietary restrictions after a transplant aren’t as strict as during dialysis. Immunosuppressants can cause weight gain, so you’ll need to keep your calorie intake in check. You’ll also need to limit your salt and fat consumption, especially if you have other medical issues, such as diabetes.[21]
- Instead of butter or animal fats, use olive, peanut, and vegetable oils.
- Use dried or fresh herbs and lemon juice instead of salt when you cook. Don’t add extra salt to your meals, and avoid processed foods like deli meat, bacon, and canned vegetables. Avoid pickled foods, and limit your consumption of ketchup, barbecue sauce, and other salty condiments.[22]
References
- ↑ https://medlineplus.gov/ency/article/000501.htm
- ↑ https://www.kidney.org/atoz/content/about-chronic-kidney-disease#what-are-main-causes-chronic-kidney-disease
- ↑ https://medlineplus.gov/ency/article/000501.htm
- ↑ http://www.kidneyfund.org/kidney-disease/chronic-kidney-disease-ckd/kidney-friendly-diet-for-ckd.html#healthy_diet_basics
- ↑ https://www.kidney.org/atoz/content/potassium
- ↑ https://medlineplus.gov/ency/article/000501.htm
- ↑ https://www.niddk.nih.gov/health-information/kidney-disease/kidney-failure/choosing-treatment
- ↑ https://www.kidney.org/atoz/content/hemodialysis
- ↑ https://www.kidney.org/atoz/content/peritoneal
- ↑ https://www.niddk.nih.gov/health-information/kidney-disease/kidney-failure/financial-help-treatment
- ↑ https://www.niddk.nih.gov/health-information/kidney-disease/kidney-failure/hemodialysis/home-hemodialysis
- ↑ https://www.niddk.nih.gov/health-information/kidney-disease/kidney-failure/choosing-treatment
- ↑ http://www.kidneyfund.org/kidney-disease/chronic-kidney-disease-ckd/kidney-friendly-diet-for-ckd.html#healthy_diet_basics
- ↑ https://www.kidney.org/atoz/content/kidney-transplant
- ↑ https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/kidney-transplant
- ↑ https://www.kidney.org/atoz/content/transplant-waitlist
- ↑ https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/kidney-transplant
- ↑ https://www.kidney.org/atoz/content/transplant-waitlist
- ↑ https://www.niddk.nih.gov/health-information/kidney-disease/kidney-failure/kidney-transplant#process
- ↑ https://www.kidney.org/atoz/content/kidney-transplant
- ↑ https://www.niddk.nih.gov/health-information/kidney-disease/kidney-failure/kidney-transplant
- ↑ http://www.kidneyfund.org/kidney-disease/chronic-kidney-disease-ckd/kidney-friendly-diet-for-ckd.html#healthy_diet_basics




































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...