This article was medically reviewed by Kate Holcomb, MD. Dr. Kate Zibilich Holcomb is a Board Certified Dermatologist and the Founder of Pure Dermatology. She has over 15 years of experience in the field and specializes in cosmetic dermatology. Dr. Holcomb earned an MS in Public Health and Parasitology from The Tulane University School of Public Health and Tropical Medicine and an MD from Tulane University School of Medicine. She also completed her residency in dermatology as Chief Resident at Saint Luke’s-Roosevelt Hospital Mount Sinai. Dr. Holcomb is a member of the American Academy of Dermatology, American Society of Dermatologic Surgeons, American Acne and Rosacea Society, Skin of Color Society, North American Contact Dermatitis Society, Louisiana Dermatological Society, and Women’s Dermatologic Society.
There are 11 references cited in this article, which can be found at the bottom of the page.
wikiHow marks an article as reader-approved once it receives enough positive feedback. In this case, 100% of readers who voted found the article helpful, earning it our reader-approved status.
This article has been viewed 595,417 times.
Melasma is a chronic skin condition that causes discoloration on the face. It usually appears as brown, tan, or blue-gray patches along the upper cheeks, upper lip, forehead, and chin. The primary factors causing melasma are hormonal changes and external sun exposure, so the most effective and long-lasting treatments are aimed reducing or eliminating these causes. Many women experience melasma during pregnancy, and, in these case, the condition will generally improve naturally after the pregnancy is over.
Steps
Treating Melasma with Prescription Medication
-
1See your primary care physician. Talk to your primary care physician about any hormonal medication changes and creams you can try for melasma before going to see a dermatologist. Treatment for melasma may be considered elective and it may not be covered by your insurance. Find out the costs of any treatments and procedures before you schedule them.
-
2Stop taking medications that could be to blame. Certain medications, like birth control pills and hormone replacement therapy, can affect your hormones and induce melasma. Talk to your doctor about stopping these medications.[1]
- Even though pregnancy is the condition most commonly associated with melasma, melasma has also been known to occur with medications and conditions that impact your hormones. Oral contraceptives and hormone replacement therapy are the next two most common causes of melasma, after pregnancy. You can stop use or try switching to a different product to determine if your melasma will fade naturally afterward.
Advertisement -
3Alter your hormone replacement therapy. Often, it is impossible to stop a hormone replacement therapy. Consider why you are on hormone replacement therapy to determine if you may be able to stop or adjust the dosage. However, there are ways that you can change your therapy so that it is less likely to cause melasma. Consult with your doctor before making any changes.
- Begin taking hormone replacements at night. If you take the hormone replacement in the morning, it will be at its peak potency when the sun is out, maximizing the risk of melasma. Shifting your regimen to the night can help alleviate the problem.
- Creams and patches might be slightly less inclined to cause melasma than oral versions of the treatment.
- Ask your doctor to administer the lowest dose feasible.[2]
-
4Ask your doctor for a prescription hydroquinone cream. While some treatments containing this ingredient can be purchased over-the-counter, your dermatologist or primary care physician can prescribe a stronger version that will be more effective at lightening the skin.
- Hydroquinone comes as a cream, lotion, gel, or liquid. It works by blocking the natural chemical process in your skin responsible for creating melanin, and since melanin produces dark skin pigmentation, the amount of dark pigmentation related to melasma will also be reduced.
- Prescription hydroquinone typically has a concentration of 4 percent. Concentrations of hydroquinone higher than 4 percent are unlikely to be prescribed in the United States and can be dangerous. They can cause ochronosis, a permanent form of skin discoloration. [3]
-
5Talk to your doctor about a second skin lightener. While hydroquinone is used as a first treatment in many cases, your dermatologist might be willing to prescribe a secondary skin lightener that can help enhance the effect.[4]
- Tretinoins and corticosteroids are among the most frequently used secondary treatments. Both are used to speed up the body's process of shedding and replacing skin cells. Some dermatologists may even prescribe "triple creams," which contain tretinoin, a corticosteroid, and hydroquinone in one formula.
- Other options include azelaic acid or kojic acid, which slow down the production of skin-darkening pigment.
Treating Melasma with Professional Procedures
-
1Get a chemical peel. A chemical peel is a procedure that uses glycolic acid or another similar chemical abrasive to peel the melasma-affected top layer of skin away.[5]
- The liquid chemical is applied to the skin, creating a mild chemical burn. As the burned layers peel off, they leave behind fresh, melasma-free skin. This will not, however, prevent melasma if you have not treated underlying hormonal imbalances.
- While glycolic acid is one of the most common options used, another common option is trichloroacetic acid, which is a compound similar to vinegar. Peels done with this chemical can be slightly more painful afterward, however, but they may present a good option for severe cases of melasma.
-
2Discuss microdermabrasion and dermabrasion. During these treatments, the top layer of skin is gradually stripped away, leaving clean, melasma-free skin in its place.[6]
- Both dermabrasion and microdermabrasion are medical procedures that essentially "sand off" the surface layer of skin using abrasive materials. During microdermabrasion, fine crystals are vacuumed across the skin. These crystals are abrasive enough to forcibly strip away dead skin cells, thereby lifting away the affected skin.
- You can usually get about five procedures done, each two to four weeks apart. You may also opt for a maintenance treatment that every four to eight weeks if the underlying cause of your melasma has not been treated.
-
3Be careful with lasers. While some laser treatments might be able to help strip away the skin affected by melasma, some can worsen the mask. Only get a laser treatment if it is administered by a credentialed professional. Look for a restorative or fractional dual laser that only targets pigmentation on the surface of the skin
- Fractional laser treatments tend to be expensive and may cost $1000 or more. Keep in mind that you will probably need three to four treatments over the course of three to six months.[7]
-
4Try treatment with platelet-rich plasma. For this treatment plasma that has been enriched to encourage recovery is injected into the body. It is an experimental recovery, still not well understood. Early evidence, however, suggests that it might not only be able to treat melasma, but even help prevent against its recurrence.[8]
Treating Melasma with Non-Prescription Home Treatment
-
1Protect your skin from the sun. Apply broad spectrum sunscreen and take other measures to protect your skin from the sun. Doing so can prevent an outbreak of melasma and may reduce the risk of current melasma getting worse.[9]
- Apply sunscreen 20 minutes before you anticipate being out in the sun. Look for a sunscreen with an SPF of 30 or higher, and consider getting one with added nutrients, like zinc, to benefit your skin.
- You could try “double” sun screening, as well. Layer an SPF 15 sunscreen on beneath an SPF 30 sunscreen for even more protection.
- Wear a wide-brimmed hat and large sunglasses to provide your face with additional protection. If your melasma is especially bad, you might also want to consider wearing long-sleeved shirts and pants. Try to stay out of direct sunlight as much as possible.
-
2Calm down. Stress can worsen hormonal imbalances, and if a hormonal imbalance is the cause of your melasma, finding ways to stress less can help treat your melasma.
- If you have difficulty relaxing, try techniques like meditation or yoga. If these do not work for you or do not appeal to you, simply make time for more things you enjoy—whether that includes walks through the park, reading, or taking a bubble bath.
-
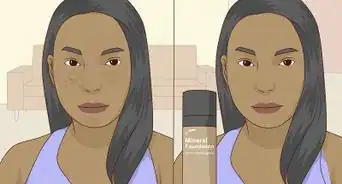
3Look for an over-the-counter hydroquinone cream. These medicated ointments lighten the skin, causing melasma outbursts to fade.[10]
- Hydroquinone comes as a cream, lotion, gel, or liquid. It works by blocking the natural chemical process in your skin responsible for creating melanin, and since melanin produces dark skin pigmentation, the amount of dark pigmentation related to melasma will also be reduced.
- There are even hydroquinone creams that contain a little sunblock, so if you want to protect your skin while treating it for melasma, these options provide an all-in-one opportunity for you to do so.
- Nonprescription hydroquinone creams usually have a concentration of 2 percent or less.
-
4Try a cream containing cysteamine. Naturally present in human body cells, cysteamine is safe and proven to treat melasma.[11]
- Cysteamine, is the natural product of L-cysteine metabolism in the human body. It acts as an intrinsic antioxidant and is known for its protective role against ionizing radiation and as an antimutagenic agent. Cysteamine acts via the inhibition of melanin synthesis to produce depigmentation.
-
5Use a cream containing kojic acid or melaplex. Both ingredients are skin brighteners, but they tend to be less harsh and less of an irritant than hydroquinone. These ingredients slow down the production of skin-darkening pigmentation in your skin. As a result, new skin cells being produced will be less dark, making it more difficult for melasma to set in.[12]
-
6Take tretinoin. This is a type of vitamin A that increases the rate at which your skin sheds dead cells. This can help patches of melasma fade faster.[13]
- Note, however, that this alone may not cure your melasma if the underlying cause has not also been remedied. The affected skin will shed quicker, but that will have no impact if your new skill cells are all affected.
-
7Try paper mulberry. This plant grows as a small tree or shrub, and while it has many non-medical uses, the extract or products containing the extract can be used orally and topically to treat melasma, as long as you follow the instructions provided on the product.[14]
-
8Experiment with other holistic treatments. Other ingredients that have been known to help when applied topically include bearberry, watercress, mandelic acid, lactic acid, lemon peel extract, apple cider vinegar, and Vitamin C. These are all capable of relaxing pigment-producing compounds in your skin without completely nullifying them and causing irritation or sensitivity to light.
-
9Wait it out. If your melasma has been induced by pregnancy, it will pass when the pregnancy is over. However, it will be more likely to occur in subsequent pregnancies.
- Cases of melasma not caused by pregnancy can last longer and might require more active intervention to treat.[15]
Expert Q&A
-
QuestionHow can I prevent melasma?
 Kate Holcomb, MDDr. Kate Zibilich Holcomb is a Board Certified Dermatologist and the Founder of Pure Dermatology. She has over 15 years of experience in the field and specializes in cosmetic dermatology. Dr. Holcomb earned an MS in Public Health and Parasitology from The Tulane University School of Public Health and Tropical Medicine and an MD from Tulane University School of Medicine. She also completed her residency in dermatology as Chief Resident at Saint Luke’s-Roosevelt Hospital Mount Sinai. Dr. Holcomb is a member of the American Academy of Dermatology, American Society of Dermatologic Surgeons, American Acne and Rosacea Society, Skin of Color Society, North American Contact Dermatitis Society, Louisiana Dermatological Society, and Women’s Dermatologic Society.
Kate Holcomb, MDDr. Kate Zibilich Holcomb is a Board Certified Dermatologist and the Founder of Pure Dermatology. She has over 15 years of experience in the field and specializes in cosmetic dermatology. Dr. Holcomb earned an MS in Public Health and Parasitology from The Tulane University School of Public Health and Tropical Medicine and an MD from Tulane University School of Medicine. She also completed her residency in dermatology as Chief Resident at Saint Luke’s-Roosevelt Hospital Mount Sinai. Dr. Holcomb is a member of the American Academy of Dermatology, American Society of Dermatologic Surgeons, American Acne and Rosacea Society, Skin of Color Society, North American Contact Dermatitis Society, Louisiana Dermatological Society, and Women’s Dermatologic Society.
Board Certified Dermatologist Newer research suggests that even indoor light and blue light from our computers may worsen melasma, so limiting exposure to that is also a factor in helping treat melasma. To protect yourself from these visible lights, you need to use tint. Tint contains iron oxide and can be in sunscreen, or you can protect yourself with a bit of makeup or colored powder, if your favorite sunscreen is clear.
Newer research suggests that even indoor light and blue light from our computers may worsen melasma, so limiting exposure to that is also a factor in helping treat melasma. To protect yourself from these visible lights, you need to use tint. Tint contains iron oxide and can be in sunscreen, or you can protect yourself with a bit of makeup or colored powder, if your favorite sunscreen is clear. -
QuestionCan melasma be permanent?
 Janice Litza, MDDr. Litza is a board certified Family Medicine Physician in Wisconsin. She is a practicing Physician and taught as a Clinical Professor for 13 years, after receiving her MD from the University of Wisconsin-Madison School of Medicine and Public Health in 1998.
Janice Litza, MDDr. Litza is a board certified Family Medicine Physician in Wisconsin. She is a practicing Physician and taught as a Clinical Professor for 13 years, after receiving her MD from the University of Wisconsin-Madison School of Medicine and Public Health in 1998.
Board Certified Family Medicine Physician Yes, it can be. You will notice it will increase in warmer months or with sun exposure and then fade, but might not disappear completely.
Yes, it can be. You will notice it will increase in warmer months or with sun exposure and then fade, but might not disappear completely.
Warnings
- If you experience skin irritation, darkening of the skin, or other skin-related problems after you begin treatment for melasma, contact your dermatologist to determine what should be done to stop these problems.⧼thumbs_response⧽
References
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4155956//
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4155956/
- ↑ http://www.medicinenet.com/melasma/page4.htm#what_is_the_treatment_for_melasma
- ↑ http://www.aad.org/dermatology-a-to-z/diseases-and-treatments/m---p/melasma/diagnosis-treatment
- ↑ https://www.aad.org/public/diseases/color-problems/melasma#treatment
- ↑ https://www.aad.org/public/diseases/color-problems/melasma#treatment
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4155956/
- ↑ https://journals.lww.com/dermatologicsurgery/Abstract/2022/01000/Platelet_Rich_Plasma_in_Melasma_A_Systematic.27.aspx
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4155956/
- ↑ https://www.aad.org/public/diseases/color-problems/melasma#treatment
- ↑ https://www.ncbi.nlm.nih.gov/pubmed/25251767
- ↑ https://my.clevelandclinic.org/health/diseases/21454-melasma
- ↑ https://www.drugs.com/health-guide/melasma-chloasma.html
- ↑ https://www.mdedge.com/dermatology/article/77722/pigmentation-disorders/mulberry
- ↑ https://www.mdedge.com/dermatology/article/77722/pigmentation-disorders/mulberry
About This Article
If you have melasma, a chronic condition that causes discoloration on your face, try using over-the-counter hydroquinone cream, which is a medicated ointment you can apply to lighten your skin pigmentation. Additionally, you can look for a non-prescription cream with cysteamine, which is an antioxidant that can prevent depigmentation. You can also try a cream with kojic acid or melaplex, which are both skin brighteners. If your over-the-counter cream isn’t working, you may want to visit a physician to get a prescription for stronger hydroquinone cream. As an alternative to medication, you can get a professional procedure like a chemical peel, microdermabrasion, or dermabrasion to remove the top layer of skin affected by melasma. For more help from our Medical co-author, including how to protect your skin from the sun to prevent your melasma from getting worse, keep reading!








































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...