This article was medically reviewed by Sarah Gehrke, RN, MS and by wikiHow staff writer, Jessica Gibson. Sarah Gehrke is a Registered Nurse and Licensed Massage Therapist in Texas. Sarah has over 10 years of experience teaching and practicing phlebotomy and intravenous (IV) therapy using physical, psychological, and emotional support. She received her Massage Therapist License from the Amarillo Massage Therapy Institute in 2008 and a M.S. in Nursing from the University of Phoenix in 2013.
There are 13 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 23,578 times.
You've probably heard tinea called by one of its other names. This fungal infection, typically a non-yeast type, can affect your feet (athlete's foot), your groin (jock itch), or any part of your skin (ringworm).[1] Tinea can also appear as discolored patches known as tinea versicolor, which is a type of yeast infection.[2] Once you've identified what kind of tinea you have, apply over-the-counter antifungal medications. These creams, lotions, or sprays can treat your tinea within a few weeks. If they don't, talk with your doctor about prescription antifungal medications that you can apply or take orally.
Steps
Treating Athlete's Foot (Tinea Pedis) and Jock Itch (Tinea Cruris)
-
1Look for blisters, rash, dry skin, and signs of athlete's foot. If your feet smell foul, are painful and red, or have blisters, you might have athlete's foot.[3] You should also check to see if the skin on your feet is peeling or if the skin between your toes is white or soggy.[4]
- You may develop a rash on your hands, known as tinea manuum, if you touch feet that are infected with athlete's foot.[5] Consider wearing gloves when examining your feet.
-
2Examine your skin for irritation, swelling, or rash to diagnose jock itch. If you have jock itch, you'll first notice a red, swollen, itchy rash at the crease between your leg and groin.[6] The rash will slowly spread up to your groin and down to your inner thigh. It can also spread around your waist and bottom. Pay attention to:[7]
- Scaly or cracked skin
- Bumpy skin with a raised border
- Itchy and painful skin, if it's infected.
Advertisement -
3Wash and dry your skin before you apply antifungal medication. If you have athlete's foot or jock itch, remember to wash your hands after you've touched your infected skin. Spread an over-the-counter antifungal cream on the affected areas or spray an antifungal medication on them.[8]
- Buy an antifungal medication that contains clotrimazole, terbinafine, or butenafine.
- Follow the manufacturer's instructions about how often to reapply the treatment throughout the day.
-
4Get medical treatment, if necessary. Your tinea should improve within 2 weeks of starting OTC medication. If your athlete's foot or jock itch doesn't clear up, remains painful, or spreads, schedule an appointment with your doctor or dermatologist. They'll examine your skin and prescribe a stronger medication.[9]
-
5Keep your skin dry to prevent tinea from returning. Moisture will make the fungus that causes tinea grow, so it's important to keep your skin dry.[10] If you had athlete's foot, wear breathable socks made of cotton and change your socks every day. If you had jock itch, change your underwear every day.[11] Consider sprinkling a talc-free powder on the skin to reduce moisture.[12]
- Wear flip flops or sandals when you're in public showers or locker rooms to prevent athlete's foot from returning.
Curing Ringworm (Tinea Corporis)
-
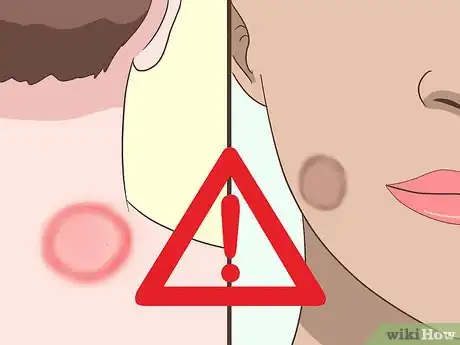
1Check your skin for scaly, round patches if you have ringworm. Because ringworm can develop anywhere on your body, look all over your body for round patches of scaly skin. If your skin is light, the patches might appear red or pink. If you have a dark skin tone, the patches will be brown or gray. Ringworm patches are often very itchy and can get bigger in size.[13]
- If ringworm isn't treated, it can spread to other parts of your body so you may want to monitor your skin for changes.
-
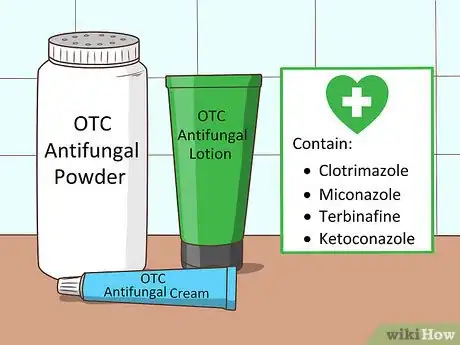
2Apply over-the-counter antifungal medications. Buy OTC antifungal cream, lotion, or powder from a pharmacy, grocery store, or supermarket. Follow the manufacturer's instructions and use the product for 2 to 4 weeks. Look for an antifungal that contains one of these active ingredients:[14]
- Clotrimazole
- Miconazole
- Terbinafine
- Ketoconazole
-
3Get an exam if the ringworm doesn't improve or gets worse. If you use an OTC medication for 2 to 4 weeks and the patches of ringworm remain or spread, schedule an appointment with your doctor. The doctor will look at your skin and scrape off a few skin cells to look at under a microscope. The doctor can use the diagnosis of ringworm to prescribe stronger medication.[15]
- If the ringworm covers a large area of your body, you might need prescription medication.
-
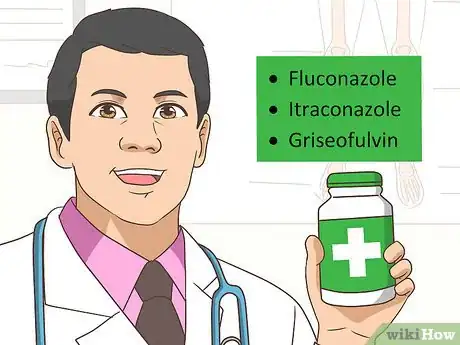
4Use prescription antifungal medications. Your doctor will prescribe an oral antifungal medication such as fluconazole, itraconazole, or griseofulvin. You could also apply a prescription lotion, cream, gel, or spray. Follow your doctor's instructions regarding dosing. For example, if you're told to finish the course of treatment, continue to take the medication even if your symptoms have improved.[16]
- The doctor might prescribe an antifungal and corticosteroid medication if you have severe or painful ringworm. Since you should only use corticosteroids in the short term, you'll likely only take the medication for less than 2 weeks.
-
5Keep your skin clean and dry to prevent spreading ringworm. Wash your skin regularly with soap and water. Dry it thoroughly after you've finished washing and wear loose clothing so you don't trap moisture next to your skin.
- To prevent spreading ringworm to others, don't share clothes, towels, or other personal items.
Treating Tinea Versicolor
-
1Pay attention to changes to your skin's color. If you notice spots appear on your body, monitor their appearance and color. The spots may be itchy and will slowly grow together to make larger patches. This tinea versicolor could disappear or fade in cooler temperatures and reappear in hot, humid weather.[17]
- The tinea versicolor spots may be white, pink, salmon, red, tan, or brown. The can show up on any part of your skin.
-
2Spread over-the-counter antifungal medication on the tinea. Go to the pharmacy, drug store, or supermarket and buy OTC antifungal shampoo, cream, soap, or lotion. Use the antifungal product on your skin a few times a day or according to the manufacturer's instructions. Use the treatments for at least 2 to 4 weeks. Look for products that contain at least one of these active ingredients:[18]
- Selenium sulfide
- Ketoconazole
- Pyrithione zinc
-
3Get a prescription for oral antifungal pills. If your skin doesn't improve 4 weeks of treatment or the tinea versicolor covers a large area, talk with your doctor or dermatologist about prescribing oral medication. Most oral antifungal pills should only be taken for a short period of time because of the risk for side effects.[19]
- Side effects of oral antifungal pills include gas, diarrhea, abdominal pain, indigestion, and headaches.[20]
-
4Wash 1 to 2 times a month with a medicated cleanser. If you live somewhere that's hot and humid, your tinea versicolor may come back. To prevent tinea versicolor from returning, wash your skin with a medicated cleanser. You can buy tinea versicolor cleansers to use or apply antifungal shampoo to your skin for 10 minutes before rinsing it off.[21]
- Note that your skin may be discolored for weeks or months after treating tinea versicolor.
- Speak to your healthcare provider about continued use of medicated cleansers for prevention of tinea versicolor.
Things You'll Need
Treating Athlete's Foot (Tinea Pedis) and Jock Itch (Tinea Cruris)
- Over-the-counter antifungal medication
- Prescription antifungal medication
- Talc-free powder
Curing Ringworm (Tinea Corporis)
- Over-the-counter antifungal medication
- Prescription antifungal medication
Treating Tinea Versicolor
- Over-the-counter antifungal medication
- Tinea versicolor cleanser
- Antifungal shampoo
- Oral antifungal pills
References
- ↑ https://www.aafp.org/afp/1998/0701/p163.html
- ↑ https://www.aad.org/public/diseases/color-problems/tinea-versicolor
- ↑ https://www.aafp.org/afp/1998/0701/p163.html
- ↑ https://www.aad.org/public/diseases/contagious-skin-diseases/ringworm#symptoms
- ↑ https://www.aafp.org/afp/2003/0101/p101.html
- ↑ https://www.aafp.org/afp/1998/0701/p163.html
- ↑ https://www.aad.org/public/diseases/contagious-skin-diseases/ringworm#symptoms
- ↑ https://www.nhs.uk/conditions/athletes-foot/
- ↑ https://www.aad.org/public/diseases/contagious-skin-diseases/ringworm#treatment
- ↑ https://www.aafp.org/afp/2003/0101/p101.html
- ↑ https://www.nhs.uk/conditions/athletes-foot/
- ↑ https://www.cancer.org/cancer/cancer-causes/talcum-powder-and-cancer.html
- ↑ https://www.aad.org/public/diseases/contagious-skin-diseases/ringworm#symptoms
- ↑ https://www.cdc.gov/fungal/diseases/ringworm/treatment.html
- ↑ https://www.aad.org/public/diseases/contagious-skin-diseases/ringworm#treatment
- ↑ https://www.cigna.com/healthwellness/hw/medical-topics/ringworm-of-the-skin-hw65253#hw65414
- ↑ https://www.aad.org/public/diseases/color-problems/tinea-versicolor#symptoms
- ↑ https://www.aad.org/public/diseases/color-problems/tinea-versicolor#treatment
- ↑ https://www.westlakedermatology.com/dermatology-procedures/tinea-versicolor/
- ↑ https://www.nhs.uk/conditions/antifungal-medicines/
- ↑ https://www.westlakedermatology.com/dermatology-procedures/tinea-versicolor/





































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...