This article was co-authored by Jurdy Dugdale, RN. Jurdy Dugdale is a Registered Nurse in Florida. She received her Nursing License from the Florida Board of Nursing in 1989.
There are 13 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 19,726 times.
An air embolism, also called a gas embolism, is a blood clot caused by an air bubble. Air embolisms are rare but potentially life-threatening medical complications. The most common cause of an air embolism is decompression sickness, which results from ascending too quickly from a deep water dive. In rare cases, air bubbles can get trapped in the bloodstream during medical procedures, such as surgery, catheterization, and IV injection. Fortunately, it's usually possible to treat an air embolism, and safety precautions can prevent one from occurring in the first place.
Steps
Administering Emergency Care
-
1Call emergency services as soon as possible. Embolisms can outwardly look a lot like a heart attack or stroke, and they are just as serious. Call emergency services as soon as possible, as medical intervention will be necessary to treat an embolism. Signs of an embolism include low blood pressure, dizziness, rapid breathing, muscle pain, tingling skin, paralysis, cyanosis, and loss of consciousness.[1]
- If you notice any of these symptoms in a person, call emergency services immediately. You do not have to be sure it is an embolism before you call. A doctor can make the diagnosis, you just need to help get the symptomatic individual to the hospital.
- Provide 100% oxygen through a close-fitting mask. Breathing 100% oxygen as early as possible will help mitigate any breathing issues caused by the embolism. Begin administering emergency oxygen as soon as an embolism is suspected. If you do not have emergency oxygen training, follow the instructions in the emergency oxygen kit closely as you begin to administer the gas.[2]
- If you do not have access to an emergency oxygen kit, let your emergency services contact know. The coming first responders will supply pure oxygen as soon as possible.
-
2Keep the patient horizontal if an arterial embolism is suspected. Shortness of breath, chest pain, dizziness, confusion, and loss of consciousness are signs of an arterial embolism. In order to prevent air bubbles from migrating to the brain, the person should lie horizontally on their back.[3]
- An arterial embolism is when an air bubble blocks an artery, which is the type of blood vessel that supplies oxygen-rich blood to organs and tissues. It may seem like a heart attack based on the symptoms.
- If air bubbles cut off the brain’s blood supply, death or permanent brain damage could result. You do not need to be able to positively diagnose an arterial embolism yourself. If you suspect one,adjust the position of the individual.
Advertisement -
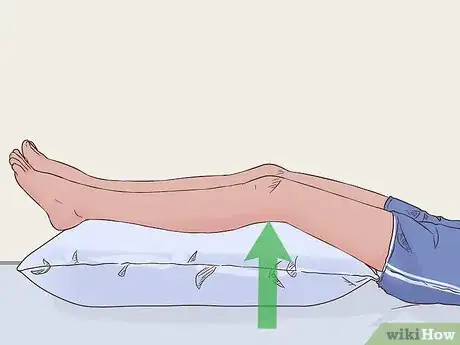
3Elevate the patient’s feet if a venous embolism is suspected. Venous embolisms are especially common in a person’s lower extremities. The symptoms may be similar to those of a blood clot, and include swelling, hardness, and redness. If you notice these symptoms in conjunction with other air embolism symptoms, adjust the person’s position so that they are lying on their left side, and their feet are 15 to 30 degrees above their head.[4]
- As with an arterial embolism, you do not need to be able to diagnose a venous embolism with 100% certainty to adjust their position. A doctor can make that diagnosis in the hospital using a CT scan or other imaging tests. Treatment for a venous embolism often requires surgery.
- A venous embolism is when an air bubble blocks a vein, which is the type of blood vessel that carries oxygen-depleted blood back to the heart.
- The purpose of the side-lying, feet-elevated position is to lower the risk of air traveling from a vein to the heart and into an artery. If air bubbles clot an artery, a major organ’s blood supply might become blocked.
-
4Administer CPR and manual ventilation, if necessary. If the person with concerning symptoms stops breathing, the first step is to stabilize them. Place 1 hand directly over the center of their chest, and your other hand over the first. Press down firmly and quickly at a rate of about 100 compressions per minute.[5]
- Do a quick check of the airway to make sure there is not a block before starting CPR. If there is a block, focus on clearing it instead of starting CPR.
- If you aren’t confident in your ability to administer CPR, see if someone nearby is certified. If you cannot find a certified individual, begin chest compressions. If the person needs CPR, it’s often a life or death situation so you become the first responder.
Getting Medical Treatment After a Trauma
-
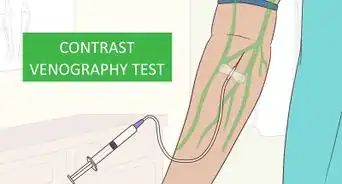
1Sit for any diagnostic testing required by your doctor. An air embolism can have symptoms similar to a heart attack or blot clot. That’s why your doctor will require testing such as a CT scan, x-rays, or an ultrasound to positively diagnose and locate an embolism. These tests will often be performed as soon as you are checked into the hospital.[6] [Image:Treat an Air Embolism Step 5.jpg|center]]
- If an embolism occurs during surgery and the patient is under anesthetic, the attending anesthesiologist may be able to detect in decrease in the amount of carbon dioxide released while monitoring the procedure.
-
2Be prepared for repositioning. If your healthcare providers suspect that a venous embolism has occurred during surgery, they’ll pause the procedure as is necessary and safe. They will then place the patient on their left side in the Trendelenburg position, which is when the feet are elevated 15 to 30 degrees above the head.[7]
-
3Prepare for surgery. Embolisms caused by trauma or while in surgery may need surgical treatment, themselves. The exact nature of the surgery will depend on the location and progression of the embolism. Be prepared for emergency surgery if you receive a diagnosis for an embolism at the hospital.[8]
Caring for an Air Embolism in a Diver
-
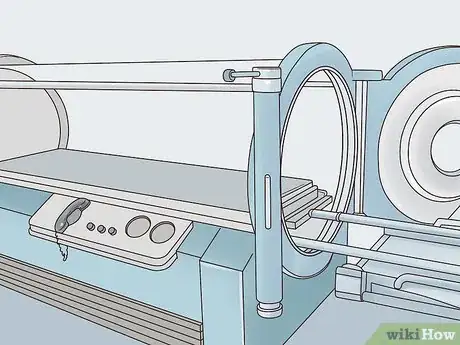
1Get to a facility equipped with a recompression chamber. Recompression in a hyperbaric chamber is the primary form of treatment for an embolism caused by decompression illness.[9] A diver who ascended too quickly or had an uncontrolled or panicked ascent and who reports any symptoms that could be attributed to an embolism should be taken to a hospital with a recompression chamber immediately.
- Not all hospitals have recompression chambers. Be sure to call ahead to any hospital and make sure they have hyperbaric facilities before an injured diver is transported there.
- In many cases, your nearest hyperbaric facility should be listed on your group’s dive plan or be on file with the company or group coordinating your dive.
- A diver who is unconscious upon ascent should also be rushed to a facility with a recompression chamber. Since they cannot say for themselves if they are experiencing symptoms, decompression sickness should be assumed until a medical professional can confirm otherwise.
-
2Remove potential fire hazards before entering the chamber. If you’re undergoing recompression therapy, your healthcare provider may ask you to wash away or remove petroleum-based skin or hair products. Additionally, you can’t have a lighter, battery-operated device, or any other object that could potentially spark while in the chamber.[10]
- Pure oxygen is highly flammable, and petroleum-based products and objects that can spark are fire hazards.
-
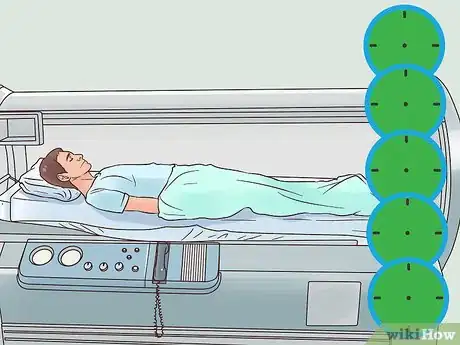
3Lie vertically in the recompression chamber for up to 5 hours. Depending on the facility, the hyperbaric chamber will either be a small room or a table that slides into a clear tube. Once you enter the chamber, the pressure is increased to at least 2 to 3 times normal air pressure. Depending on your condition’s severity, you’ll spend 45 minutes to 5 hours in the chamber. Your attending doctor will let you know exactly how long you need to stay in recompression.[11]
- The high pressure causes the nitrogen to be reabsorbed by your blood stream. This will restore normal blood flow and reduce the size of the embolism. Then, the pressure will be slowly lowered, mimicking a slow, controlled ascent and preventing the embolism from returning.
- When you enter the chamber, your ears might pop, as if you were ascending in an airplane. Swallowing or yawning can offer relief.[12]
- Additional recompression sessions may be necessary if you have severe symptoms. Your doctor will talk you through any additional sessions you may need after your initial recompression.
-
4Use safe diving guidelines to help prevent future embolisms. Always dive with a buddy, and never exceed your skill level. Plan your dive in advance, and ensure you have enough oxygen for a slow ascent, and take both safety and mandatory decompression stops.
- Check your equipment before diving, and make sure your dive computer, depth gauge, tank gauge, and timer are functioning.[13]
- Avoid flying for at least 12 hours after a no-decompression dive. If you did need to take decompression stops, don’t fly for 24 hours after diving. Additionally, try to stay close to sea level for 12 to 24 hours after diving.[14]
-
5Ascend slowly from a dive and take decompression stops to prevent embolisms. Always ascend at a rate no faster than 30 feet (9.1 m) per minute. Familiarize yourself with maximum dive times for specific depths, take decompression stops when necessary, and never exceed recommended depth or duration limits.[15]
- For example, if you stay at a depth of 60 feet (18 m) for 60 minutes, you need to make a decompression stop for 5 minutes every 15 feet (4.6 m). If you ascend at 30 feet (9.1 m) per minute and take 3 decompression stops, it'll take a minimum of 17 minutes to resurface.
- Always round up when estimating depths and duration. If you’ve spent 51 minutes at 53 feet (16 m), round up to 60 minutes at 60 feet (18 m).
- For dive tables that list maximum depths, times, and guidelines for decompression stops, see https://www.naui.org/resources/dive-tables-review.
References
- ↑ https://www.nhs.uk/conditions/air-embolism/
- ↑ https://www.nhs.uk/conditions/air-embolism/
- ↑ https://www.merckmanuals.com/professional/injuries-poisoning/injury-during-diving-or-work-in-compressed-air/arterial-gas-embolism
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3665124/
- ↑ https://www.youtube.com/watch?v=-NodDRTsV88
- ↑ https://www.heart.org/en/health-topics/venous-thromboembolism/symptoms-and-diagnosis-of-venous-thromboembolism-vte
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5126790/
- ↑ https://www.annalsthoracicsurgery.org/article/S0003-4975(99)00822-X/pdf
- ↑ https://www.ncbi.nlm.nih.gov/pubmed/2675253
- ↑ https://www.mayoclinic.org/tests-procedures/hyperbaric-oxygen-therapy/about/pac-20394380?p=1
- ↑ https://www.merckmanuals.com/professional/injuries-poisoning/injury-during-diving-or-work-in-compressed-air/recompression-therapy
- ↑ https://medlineplus.gov/ency/article/002375.htm
- ↑ https://www.nhs.uk/conditions/air-embolism/#treating-an-air-or-gas-embolism-caused-by-diving
- ↑ https://familydoctor.org/scuba-diving-safety/?adfree=true
- ↑ https://www.nhs.uk/conditions/air-embolism/#treating-an-air-or-gas-embolism-caused-by-diving











-Step-13.webp)


-Step-16.webp)














































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...