Pandemic
A pandemic (/pænˈdɛmɪk/ pan-DEM-ik) is an epidemic of an infectious disease that has spread across a large region, for instance multiple continents or worldwide, affecting a substantial number of individuals. Widespread endemic diseases with a stable number of infected individuals such as recurrences of seasonal influenza are generally excluded as they occur simultaneously in large regions of the globe rather than being spread worldwide.
.jpg.webp)
Throughout human history, there have been a number of pandemics of diseases such as smallpox. The most fatal pandemic in recorded history was the Black Death—also known as The Plague—which killed an estimated 75–200 million people in the 14th century.[2][3][4][5] The term had not been used then but was used for later epidemics, including the 1918 influenza pandemic—more commonly known as the Spanish flu.[6][7][8] The most recent pandemics include the HIV/AIDS pandemic,[lower-alpha 1][9] the 2009 H1N1 pandemic and the COVID-19 pandemic. Almost all these diseases still circulate among humans though their impact now is far less.
In response to the COVID-19 pandemic, recently 194 member states of the World Health Organization began negotiations on an International Treaty on Pandemic Prevention, Preparedness and Response with a requirement to submit a draft of this treaty to the 77th World Health Assembly during its 2024 convention. This is expected to set rules for dealing with a pandemic by the international community.[10][11]
Definition
A medical dictionary definition of pandemic is "an epidemic occurring on a scale that crosses international boundaries, usually affecting people on a worldwide scale".[12] A disease or condition is not a pandemic merely because it is widespread or kills many people; it must also be infectious. For instance, cancer is responsible for many deaths but is not considered a pandemic because the disease is not contagious—i.e. easily transmissible—and not even simply infectious.[13] This definition differs from colloquial usage in that it encompasses outbreaks of relatively mild diseases.[14][15]
The World Health Organization's (WHO) nearest equivalent of "pandemic" is what is known as a Public Health Emergency of International Concern, defined as "an extraordinary event which is determined to constitute a public health risk to other States through the international spread of disease and to potentially require a coordinated international response".[16] There is a rigorous process underlying this categorization and a clearly defined trajectory of responses.[17]
A WHO-sponsored international body, tasked with preparing an international agreement on pandemic prevention, preparedness and response has defined a pandemic as "the global spread of a pathogen or variant that infects human populations with limited or no immunity through sustained and high transmissibility from person to person, overwhelming health systems with severe morbidity and high mortality, and causing social and economic disruptions, all of which require effective national and global collaboration and coordination for its control".[18]
The word comes from the Greek παν- pan- meaning "all", or "every" and δῆμος demos "people".
Parameters
A common early characteristic of a pandemic is a rapid, sometimes exponential, growth in the number of infections, coupled with a widening geographical spread.[19]
WHO utilises different criteria to declare a Public Health Emergency of International Concern (PHEIC), its nearest equivalent to the term pandemic.[20] The potential consequences of an incident are considered, rather than its current status.[21] For example, polio was declared a PHEIC in 2014 even though only 482 cases were reported globally in the previous year;[22] this was justified by concerns that polio might break out of its endemic areas and again become a significant health threat globally.[23] The PHEIC status of polio is reviewed regularly and is ongoing, despite the small number of cases annually.[lower-alpha 2][24]
The end of a pandemic is more difficult to delineate. Generally, past epidemics & pandemics have faded out as the diseases become accepted into people's daily lives and routines, becoming endemic.[25] The transition from pandemic to endemic may be defined based on: -
- a high proportion of the global population having immunity (through either natural infection or vaccination)
- fewer deaths
- health systems step down from emergency status
- perceived personal risk is lessened
- restrictive measures such as travel restrictions removed
- less coverage in public media.[26][27]
An endemic disease is always present in a population, but at a relatively low and predictable level. There may be periodic spikes of infections or seasonality, (e.g. influenza) but generally the burden on health systems is manageable.[26]
Prevention and preparedness

Pandemic prevention comprises activities such as anticipatory research and development of therapies and vaccines, as well as monitoring for pathogens and disease outbreaks which may have pandemic potential.[28] Routine vaccination programs are a type of prevention strategy, holding back diseases such as influenza and polio which have caused pandemics in the past, and could do so again if not controlled.[29] Prevention overlaps with preparedness which aims to curtail an outbreak and prevent it getting out of control - it involves strategic planning, data collection and modelling to measure the spread, stockpiling of therapies, vaccines, and medical equipment, as well as public health awareness campaigning.[30] By definition, a pandemic involves many countries so international cooperation, data sharing, and collaboration are essential; as is universal access to tests and therapies.[28]
Collaboration - In response to the COVID-19 pandemic, WHO established a Pandemic Hub in September 2021 in Berlin, aiming to address weaknesses around the world in how countries detect, monitor and manage public health threats. The Hub's initiatives include using artificial intelligence to analyse more than 35,000 data feeds for indications of emerging health threats, as well as improving facilities and coordination between academic institutions and WHO member countries.[31]
Detection - In May 2023, WHO launched the International Pathogen Surveillance Network (IPSN) (hosted by the Pandemic Hub) aiming to detect and respond to disease threats before they become epidemics and pandemics, and to optimize routine disease surveillance. The network provides a platform to connect countries, improving systems for collecting and analysing samples of potentially harmful pathogens.[32]
Therapies and Vaccines - The Coalition for Epidemic Preparedness Innovations (CEPI) is developing a program to condense new vaccine development timelines to 100 days, a third of the time it took to develop a COVID-19 vaccine. CEPI aims to reduce global epidemic and pandemic risk by developing vaccines against known pathogens as well as enabling rapid response to Disease X.[33][34] In the US, the National Institute of Allergy and Infectious Diseases (NIAID) has developed a Pandemic Preparedness Plan which focuses on identifying viruses of concern and developing diagnostics and therapies (including prototype vaccines) to combat them.[35][36]
Modeling is important to inform policy decisions. It helps to predict the burden of disease on healthcare facilities, the effectiveness of control measures, projected geographical spread, and timing and extent of future pandemic waves.[37]
Public Awareness involves disseminating reliable information, ensuring consistency on message, transparency, and steps to discredit misinformation.[38]
Stockpiling involves maintaining strategic stockpiles of emergency supplies such as personal protective equipment, drugs and vaccines, and equipment such as respirators. Many of these items have limited shelf life, so they require stock rotation even though they may be rarely used.[39]
Pandemic management strategies

The basic strategies in the control of an outbreak are containment and mitigation. Containment may be undertaken in the early stages of the outbreak, including contact tracing and isolating infected individuals to stop the disease from spreading to the rest of the population, other public health interventions on infection control, and therapeutic countermeasures such as vaccinations which may be effective if available.[47] When it becomes apparent that it is no longer possible to contain the spread of the disease, management will then move on to the mitigation stage, in which measures are taken to slow the spread of the disease and mitigate its effects on society and the healthcare system. In reality, containment and mitigation measures may be undertaken simultaneously.[48]
A key part of managing an infectious disease outbreak is trying to decrease the epidemic peak, known as "flattening the curve".[40][43] This helps decrease the risk of health services being overwhelmed and provides more time for a vaccine and treatment to be developed.[40][43] A broad group of non-pharmaceutical interventions may be taken to manage the outbreak.[43] In a flu pandemic, these actions may include personal preventive measures such as hand hygiene, wearing face-masks, and self-quarantine; community measures aimed at social distancing such as closing schools and canceling mass gatherings; community engagement to encourage acceptance and participation in such interventions; and environmental measures such as cleaning of surfaces.[41]
Another strategy, suppression, requires more extreme long-term non-pharmaceutical interventions to reverse the pandemic by reducing the basic reproduction number to less than 1. The suppression strategy, which includes stringent population-wide social distancing, home isolation of cases, and household quarantine, was undertaken by China during the COVID-19 pandemic where entire cities were placed under lockdown; such a strategy may carry with it considerable social and economic costs.[49]
Frameworks for influenza pandemics
WHO system
For a novel influenza virus, WHO previously applied a six-stage classification to delineate the process by which the virus moves from the first few infections in humans through to a pandemic. Starting with phase 1 (infections identified in animals only), it moves through phases of increasing infection and spread to phase 6 (pandemic).[50] In February 2020, a WHO spokesperson clarified that the system is no longer in use.[51]
CDC Frameworks
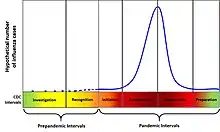
In 2014, the United States Centers for Disease Control and Prevention (CDC) introduced a framework for characterising the progress of an influenza pandemic titled the Pandemic Intervals Framework.[52] The six intervals of the framework are as follows:
- investigation of cases of novel influenza,
- recognition of increased potential for ongoing transmission,
- initiation of a pandemic wave,
- acceleration of a pandemic wave,
- deceleration of a pandemic wave, and
- preparation for future pandemic waves.
At the same time, the CDC adopted the Pandemic Severity Assessment Framework (PSAF) to assess the severity of influenza pandemics.[52] The PSAF rates the severity of an influenza outbreak on two dimensions: clinical severity of illness in infected persons; and the transmissibility of the infection in the population.[53] This tool was not applied during the COVID-19 pandemic.[54]
Notable pandemics and outbreaks
COVID-19

SARS-CoV-2, a new strain of coronavirus, was first detected in the city of Wuhan, Hubei Province, China, in December 2019.[56] The outbreak was characterized as a Public Health Emergency of International Concern (PHEIC) between January 2020 and May 2023 by WHO.[57][58] The number of people infected with COVID-19 has reached more than 767 million worldwide, with a death toll of 6.9 million.[lower-alpha 3][59] It is considered likely that the virus will eventually become endemic and, like the common cold, cause less severe disease for most people.[60]
HIV/AIDS
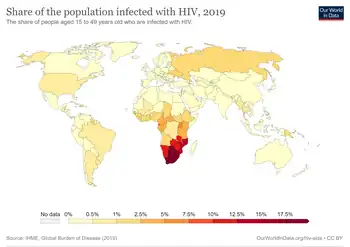
HIV/AIDS was first identified as a disease in 1981, and is an ongoing worldwide public health issue.[61][62] Since then HIV/AIDS has killed an estimated 40 million people with a further 630,000 deaths annually; 39 million people are currently living with HIV infection.[lower-alpha 4][61] HIV has a zoonotic origin, having originated in nonhuman primates in Central Africa and transferred to humans in the early 20th century.[63] The most frequent mode of transmission of HIV is through sexual contact with an infected person. There may be a short period of mild, nonspecific symptoms followed by an asymptomatic (but nevertheless infectious) stage called clinical latency - without treatment, this stage can last between 3 and 20 years. The only way to detect infection is by means of a HIV test.[64] There is no vaccine to prevent HIV infection, but the disease can be held in check by means of antiretroviral therapy.[65]
Pandemics in history
Historical accounts of epidemics are often vague or contradictory in describing how victims were affected. A rash accompanied by a fever might be smallpox, measles, scarlet fever, or varicella, and it is possible that epidemics overlapped, with multiple infections striking the same population at once. It is often impossible to know the exact causes of mortality, although ancient DNA studies can sometimes detect residues of certain pathogens.[66]


It is assumed that, prior to the neolithic revolution around 10,000 BC, disease outbreaks were limited to a single family or clan. and did not spread widely before dying out. The domestication of animals increased human-animal contact, increasing the possibility of zoonotic infections. The advent of agriculture, and trade between settled groups, made it possible for pathogens to spread widely. As population increased, contact between groups became more frequent. A history of epidemics maintained by the Chinese Empire from 243 B.C. to 1911 A.C. shows an approximate correlation between the frequency of epidemics and the growth of the population.[68]
Here is an incomplete list of known epidemics which spread widely enough to merit the title "pandemic".
- Plague of Athens (430 to 426 BC): During the Peloponnesian War, an epidemic killed a quarter of the Athenian troops and a quarter of the population. This disease fatally weakened the dominance of Athens, but the sheer virulence of the disease prevented its wider spread; i.e., it killed off its hosts at a rate faster than they could spread it. The exact cause of the plague was unknown for many years. In January 2006, researchers from the University of Athens analyzed teeth recovered from a mass grave underneath the city and confirmed the presence of bacteria responsible for typhoid fever.[69]
- Antonine Plague (165 to 180 AD): Possibly measles or smallpox brought to the Italian peninsula by soldiers returning from the Near East, it killed a quarter of those infected, up to five million in total.[70]
- Plague of Cyprian (251–266 AD): A second outbreak of what may have been the same disease as the Antonine Plague killed (it was said) 5,000 people a day in Rome.[71]
- Plague of Justinian (541 to 549 AD): Also known as the First Plague Pandemic. This epidemic started in Egypt and reached Constantinople the following spring, killing (according to the Byzantine chronicler Procopius) 10,000 a day at its height, and perhaps 40% of the city's inhabitants. The plague went on to eliminate a quarter to half the human population of the known world and was identified in 2013 as being caused by bubonic plague.[72][73]
- Black Death (1331 to 1353): Also known as the Second Plague Pandemic. The total number of deaths worldwide is estimated at 75 to 200 million. Starting in Asia, the disease reached the Mediterranean and western Europe in 1348 (possibly from Italian merchants fleeing fighting in Crimea) and killed an estimated 20 to 30 million Europeans in six years;[74] a third of the total population,[75] and up to a half in the worst-affected urban areas.[76] It was the first of a cycle of European plague epidemics that continued until the 18th century;[77] there were more than 100 plague epidemics in Europe during this period,[78] including the Great Plague of London of 1665–66 which killed approximately 100,000 people, 20% of London's population.[79]
- 1817–1824 cholera pandemic. Previously endemic in the Indian subcontinent, the pandemic began in Bengal, then spread across India by 1820. The deaths of 10,000 British troops were documented - it is assumed that tens of thousands of Indians must have died.[80] The disease spread as far as China, Indonesia (where more than 100,000 people succumbed on the island of Java alone)[81] and the Caspian Sea before receding. Subsequent cholera pandemics during the 19th century are estimated to have caused many millions of deaths globally.[82][83]
 Great Plague of Marseille in 1720 killed a total of 100,000 people
Great Plague of Marseille in 1720 killed a total of 100,000 people - Third plague pandemic (1855–1960): Starting in China, it is estimated to have caused over 12 million deaths in total, the majority of them in India.[84][85] During this pandemic, the United States saw its first outbreak: the San Francisco plague of 1900–1904.[86] The causative bacterium, Yersinia pestis, was identified in 1894.[87] The association with fleas, and in particular rat fleas in urban environments, led to effective control measures. The pandemic was considered to be over in 1959 when annual deaths due to plague dropped below 200. The disease is nevertheless present in the rat population worldwide and isolated human cases still occur.[88]
- The 1918–1920 Spanish flu infected half a billion people[89] around the world, including on remote Pacific islands and in the Arctic—killing 20 to 100 million.[89][90] Most influenza outbreaks disproportionately kill the very young and the very old, but the 1918 pandemic had an unusually high mortality rate for young adults.[91] It killed more people in 25 weeks than AIDS did in its first 25 years.[92][93] Mass troop movements and close quarters during World War I caused it to spread and mutate faster, and the susceptibility of soldiers to the flu may have been increased by stress, malnourishment and chemical attacks.[94] Improved transportation systems made it easier for soldiers, sailors and civilian travelers to spread the disease.[95]
Pandemics in indigenous populations

Beginning from the Middle Ages, encounters between European settlers and native populations in the rest of the world often introduced epidemics of extraordinary virulence. Settlers introduced novel diseases which were endemic in Europe, such as smallpox, measles, pertussis.and influenza, to which the indigenous peoples had no immunity.[96][97] The Europeans infected with such diseases typically carried them in a dormant state, were actively infected but asymptomatic, or had only mild symptoms.[98]
Smallpox was the most destructive disease that was brought by Europeans to the Native Americans, both in terms of morbidity and mortality. The first well-documented smallpox epidemic in the Americas began in Hispaniola in late 1518 and soon spread to Mexico.[98] Estimates of mortality range from one-quarter to one-half of the population of central Mexico.[99] It is estimated that over the 100 years after European arrival in 1492, the indigenous population of the Americas dropped from 60 million to only 6 million, due to a combination of disease, war, and famine. The majority these deaths are attributed to successive waves of introduced diseases such as smallpox, measles, and typhoid fever.[100][101][102]
In Australia, smallpox was introduced by European settlers in 1789 devastating the Australian Aboriginal population, killing an estimated 50% of those infected with the disease during the first decades of colonisation.[103] In the early 1800s, measles, smallpox and intertribal warfare killed an estimated 20,000 New Zealand Māori.[104]
In 1848–49, as many as 40,000 out of 150,000 Hawaiians are estimated to have died of measles, whooping cough and influenza. Measles killed more than 40,000 Fijians, approximately one-third of the population, in 1875,[105] and in the early 19th century devastated the Great Andamanese population.[106] In Hokkaido, an epidemic of smallpox introduced by Japanese settlers is estimated to have killed 34% of the native Ainu population in 1845.[107]
Concerns about future pandemics
Prevention of future pandemics requires steps to identify future causes of pandemics and to take preventive measures before the disease moves uncontrollably into the human population.
For example, influenza is a rapidly evolving disease which has caused pandemics in the past and has potential to cause future pandemics. WHO collates the findings of 144 national influenza centres worldwide which monitor emerging flu viruses. Virus variants which are assessed as likely to represent a significant risk are identified and can then be incorporated into the next seasonal influenza vaccine program.[108]
In a press conference on 28 December 2020, Mike Ryan, head of the WHO Emergencies Program, and other officials said the current COVID-19 pandemic is "not necessarily the big one" and "the next pandemic may be more severe." They called for preparation.[109] WHO and the UN have warned the world must tackle the cause of pandemics and not just the health and economic symptoms.[110]
Diseases with pandemic potential
There is always a possibility that a disease which has caused epidemics in the past may return in the future.[68] It is also possible that little known diseases may become more virulent; in order to encourage research, a number of organisations which monitor global health have drawn up lists of diseases which may have pandemic potential; see table below.[lower-alpha 5]
| WHO[111] | CEPI[112] | GAVI[113] | |
|---|---|---|---|
| Chikungunya | Yes | ||
| COVID-19 | Yes | ||
| Crimean-Congo haemorrhagic fever | Yes | Yes | |
| Ebola virus disease | Yes | Yes | Yes |
| Lassa fever | Yes | Yes | Yes |
| Marburg virus disease | Yes | Yes | |
| Mpox | Yes | ||
| Middle East respiratory syndrome coronavirus (MERS-CoV) | Yes | Yes | |
| Nipah and other henipaviral diseases | Yes | Yes | Yes |
| Rift Valley fever | Yes | Yes | Yes |
| Severe Acute Respiratory Syndrome (SARS) | Yes | Yes | Yes |
| Zika | Yes | Yes | |
| Disease X [lower-alpha 6] | Yes | Yes |
Coronaviruses
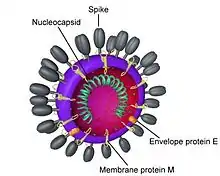
Coronavirus diseases are a family of usually mild illnesses in humans, including those such as the common cold, that have resulted in outbreaks and pandemics such as the 1889-1890 pandemic,[114][115] the 2002–2004 SARS outbreak, Middle East respiratory syndrome–related coronavirus and the COVID-19 pandemic. There is widespread concern that members of the coronavirus family, particularly SARS and MERS have the potential to cause future pandemics.[116] Many human coronaviruses have zoonotic origin, their with natural reservoir in bats or rodents,[117] leading to concerns for future spillover events.[118]
Following the end of the COVID-19 pandemic Public Health Emergency of International Concern deceleration by WHO, WHO Director General Tedros Ghebreyesus stated he would not hesitate to re-declare COVID-19 a PHEIC should the global situation worsen in the coming months or years.
Influenza

Influenza was first described by the Greek physician Hippocrates in 412 BC.[120] Since the Middle Ages, influenza pandemics have been recorded every 10 to 30 years as the virus mutates to evade immunity.[121][122]
Influenza is an endemic disease, with a fairly constant number of cases which vary seasonally and can, to a certain extent, be predicted.[123] In a typical year, 5–15% of the population contracts influenza. There are 3–5 million severe cases annually, with up to 650,000 respiratory-related deaths globally each year.[124] The 1889–1890 pandemic is estimated to have caused around a million fatalities,[125] and the "Spanish flu" of 1918–1920 eventually infected about one-third of the world's population and caused an estimate 50 million fatalities.[89]
The Global Influenza Surveillance and Response System is a global network of laboratories that has for purpose to monitor the spread of influenza with the aim to provide WHO with influenza control information.[126] More than two million respiratory specimens are tested by GISRS annually to monitor the spread and evolution of influenza viruses through a network of about 150 laboratories in 114 countries representing 91% of the world's population.[127]
Antibiotic resistance
Antibiotic-resistant microorganisms, which sometimes are referred to as "superbugs", may contribute to the re-emergence of diseases with pandemic potential that are currently well controlled.[128]
For example, cases of tuberculosis that are resistant to traditionally effective treatments remain a cause of great concern to health professionals. Every year, nearly half a million new cases of multidrug-resistant tuberculosis (MDR-TB) are estimated to occur worldwide.[129] China and India have the highest rate of MDR-TB.[130] WHO reports that approximately 50 million people worldwide are infected with MDR-TB, with 79 percent of those cases resistant to three or more antibiotics. Extensively drug-resistant tuberculosis (XDR-TB) was first identified in Africa in 2006 and subsequently discovered to exist in 49 countries. During 2021 there were estimated to be around 25,000 cases XDR-TB worldwide.[131]
In the past 20 years, other common bacteria including Staphylococcus aureus, Serratia marcescens and Enterococcus, have developed resistance to a wide range of antibiotics. Antibiotic-resistant organisms have become an important cause of healthcare-associated (nosocomial) infections.[132]
Climate change

There are two groups of infectious disease that may be affected by climate change. The first group are vector-borne diseases which are transmitted via insects such as mosquitos or ticks.[133] Some of these diseases, such as malaria, yellow fever, and dengue fever, can have potentially severe health consequences. Climate can affect the distribution of these diseases due to the changing geographic range of their vectors, with the potential to cause serious outbreaks in areas where the disease has not previously been known.[134] The other group comprises water-borne diseases such as cholera, dysentery, and typhoid which may increase in prevalence due to changes in rainfall patterns.[135]
Encroaching into wildlands
The October 2020 'era of pandemics' report by the United Nations' Intergovernmental Science-Policy Platform on Biodiversity and Ecosystem Services, written by 22 experts in a variety of fields, said the anthropogenic destruction of biodiversity is paving the way to the pandemic era and could result in as many as 850,000 viruses being transmitted from animals—in particular birds and mammals—to humans. The "exponential rise" in consumption and trade of commodities such as meat, palm oil, and metals, largely facilitated by developed nations, and a growing human population, are the primary drivers of this destruction. According to Peter Daszak, the chair of the group who produced the report, "there is no great mystery about the cause of the Covid-19 pandemic or any modern pandemic. The same human activities that drive climate change and biodiversity loss also drive pandemic risk through their impacts on our environment." Proposed policy options from the report include taxing meat production and consumption, cracking down on the illegal wildlife trade, removing high-risk species from the legal wildlife trade, eliminating subsidies to businesses that are harmful to the natural world, and establishing a global surveillance network.[136][137][138]
In June 2021, a team of scientists assembled by the Harvard Medical School Center for Health and the Global Environment warned that the primary cause of pandemics so far, the anthropogenic destruction of the natural world through such activities including deforestation and hunting, is being ignored by world leaders.[139]
Economic consequences
In 2016, the commission on a Global Health Risk Framework for the Future estimated that pandemic disease events would cost the global economy over $6 trillion in the 21st century—over $60 billion per year.[140] The same report recommended spending $4.5 billion annually on global prevention and response capabilities to reduce the threat posed by pandemic events, a figure that the World Bank Group raised to $13 billion in a 2019 report.[141] It has been suggested that such costs be paid from a tax on aviation rather than from, e.g., income taxes,[142] given the crucial role of air traffic in transforming local epidemics into pandemics (being the only factor considered in state-of-the-art models of long-range disease transmission [143]).
The COVID-19 pandemic is expected to have a profound negative effect on the global economy, potentially for years to come, with substantial drops in GDP accompanied by increases in unemployment noted around the world.[43] The slowdown of economic activity early in the COVID-19 pandemic had a profound effect on emissions of pollutants and greenhouse gases.[144][145][146] Analysis of ice cores taken from the Swiss Alps have revealed a reduction in atmospheric lead pollution over a four-year period corresponding to the years 1349 to 1353 (when the Black Death was ravaging Europe), indicating a reduction in mining and economic activity generally.[147]
See also
- Asian Flu of 1957
- Biological hazard
- Compartmental models in epidemiology
- Contagious disease
- Crowdmapping
- Disease X
- European Centre for Disease Prevention and Control (ECDC)
- Hong Kong Flu of 1968
- Immunization
- Index case
- Mortality from infectious diseases
- List of pandemics and epidemics
- Mathematical modelling of infectious disease
- Medieval demography
- Pandemic fatigue
- Pandemic severity index
- Public health emergency of international concern
- Super-spreader
- Syndemic
- Tropical disease
- Timeline of global health
- Twindemic
- Vaccination
- WHO pandemic phases
Notes
- Most medical sources including the WHO do not refer to HIV/AIDS as a pandemic, those that do refer to it in the past-tense to separate the acute and chronic phases.
- As of August 2023
- Statistics as of August 2023
- Statistics as at the end of 2022
- As of June 2023, the WHO is reviewing its list
- Disease X represents the knowledge that a serious international epidemic could be caused by a pathogen currently unknown to cause human disease.
References
- Serbu J (27 March 2020). "Army Corps sees convention centers as good option to build temporary hospitals". Federal News Network. Archived from the original on 14 April 2020.
- "Black death 'discriminated' between victims (ABC News in Science)". Australian Broadcasting Corporation. 29 January 2008. Archived from the original on 20 December 2016. Retrieved 3 November 2008.
- "Black Death's Gene Code Cracked". Wired. 3 October 2001. Archived from the original on 26 April 2015. Retrieved 12 February 2015.
- "Health: De-coding the Black Death". BBC. 3 October 2001. Archived from the original on 7 July 2017. Retrieved 3 November 2008.
- DeLeo FR, Hinnebusch BJ (September 2005). "A plague upon the phagocytes". Nature Medicine. 11 (9): 927–928. doi:10.1038/nm0905-927. PMID 16145573. S2CID 31060258.
- 1918 Pandemics (H1N1 virus). Centers for Disease Control and Prevention. Retrieved 18 April 2020.
- Rosenwald MS (7 April 2020). "History's deadliest pandemics, from ancient Rome to modern America". The Washington Post. Archived from the original on 7 April 2020. Retrieved 11 April 2020.
- "Weekly Virological Update on 05 August 2010". World Health Organization (WHO). 5 August 2010. Archived from the original on 7 August 2015. Retrieved 8 April 2020.
- Roychoudhury S, Das A, Sengupta P, Dutta S, Roychoudhury S, Choudhury AP, et al. (December 2020). "Viral Pandemics of the Last Four Decades: Pathophysiology, Health Impacts and Perspectives". International Journal of Environmental Research and Public Health. 17 (24): 9411. doi:10.3390/ijerph17249411. PMC 7765415. PMID 33333995.
- "World Health Assembly agrees to launch process to develop historic global accord on pandemic prevention, preparedness and response". World Health Organization. 1 December 2021. Retrieved 2 December 2021.
- Cumming-Bruce N (1 December 2021). "W.H.O. members agree to begin talks on a global pandemic treaty". The New York Times. ISSN 0362-4331. Retrieved 2 December 2021.
- Porta M, ed. (2008). Dictionary of Epidemiology. Oxford University Press. p. 179. ISBN 978-0-19-531449-6. Retrieved 14 September 2012.
- Dumar AM (2009). Swine Flu: What You Need to Know. Wildside Press LLC. p. 7. ISBN 978-1434458322.
- Morens D, Folkers G, Fauci A (1 October 2009). "What Is a Pandemic?". Oxford University Press. The Journal of Infectious Diseases. Retrieved 7 June 2023.
- Doshi P (July 2011). "The elusive definition of pandemic influenza". Bulletin of the World Health Organization. 89 (7): 532–538. doi:10.2471/BLT.11.086173. PMC 3127275. PMID 21734768.
- "Emergencies: International health regulations and emergency committees". World Health Organization. 19 December 2019. Retrieved 7 June 2023.
- Ross E (20 October 2022). "What is the difference between a pandemic and a PHEIC? (Video)". Chatham House, The Royal Institute of International Affairs. Retrieved 7 June 2023.
- "Zero draft of the WHO convention, agreement or other international instrument on pandemic prevention, preparedness and response ("WHO CA+")" (PDF). World Health Organization – Intergovernmental Negotiating Body. 1 February 2023. Retrieved 7 June 2023.
- Foster, Grant; Elderd, Bret D; Richards, Robert L; Dallas, Tad (1 September 2022). Wilson, Ian (ed.). "Estimating R 0 from early exponential growth: parallels between 1918 influenza and 2020 SARS-CoV-2 pandemics". PNAS Nexus. 1 (4): pgac194. doi:10.1093/pnasnexus/pgac194. ISSN 2752-6542. PMC 9802102. PMID 36714850.
- Ross, Emma (20 October 2022). "What is the difference between a pandemic and a PHEIC (Video explainer)". Chatham House, The Royal Institute of International Affairs. Retrieved 25 August 2023.
There's a whole infrastructure and official process around designating something a PHEIC and designating that an outbreak is no longer a PHEIC. There's none of that when it comes to calling an outbreak pandemic.
- Wilder-Smith, Annelies; Osman, Sarah (23 December 2020). "Public health emergencies of international concern: a historic overview". Journal of Travel Medicine. 27 (8). doi:10.1093/jtm/taaa227. ISSN 1195-1982. PMC 7798963. PMID 33284964.
- "GHO | By category | Poliomyelitis - Reported cases by country". WHO. Retrieved 25 August 2023.
- "WHO statement on the meeting of the International Health Regulations Emergency Committee concerning the international spread of wild poliovirus". World Health Organization. 5 May 2014. Retrieved 25 August 2023.
- "Statement of the Thirty-sixth Meeting of the Polio IHR Emergency Committee". www.who.int. Retrieved 25 August 2023.
- Charters, Erica; Heitman, Kristin (February 2021). "How epidemics end". Centaurus. 63 (1): 210–224. doi:10.1111/1600-0498.12370. ISSN 0008-8994. PMC 8014506. PMID 33821019.
- Ioannidis, John P. A. (June 2022). "The end of the COVID‐19 pandemic". European Journal of Clinical Investigation. 52 (6): e13782. doi:10.1111/eci.13782. ISSN 0014-2972. PMC 9111437. PMID 35342941.
- Steenhuysen, Julie (17 November 2021). "Fauci says boosters for all key to U.S. reaching COVID-19 endemic level". Reuters. Retrieved 22 August 2023.
- Williams N (6 July 2022). "What is Pandemic Preparedness and Why is it Important?". News Medical Network. Retrieved 20 August 2023.
- "14 Diseases You Almost Forgot About (Thanks to Vaccines)". Centers for Disease Control and Prevention. 15 September 2022. Retrieved 21 August 2023.
- Campbell K (15 November 2022). "3 Steps to Detect and Stop Disease Outbreaks before They Become Pandemics". Scientific American. Retrieved 21 August 2023.
- Morgan O, Pebody R (May 2022). "The WHO Hub for Pandemic and Epidemic Intelligence; supporting better preparedness for future health emergencies". Euro Surveillance. 27 (20): 2200385. doi:10.2807/1560-7917.ES.2022.27.20.2200385. PMC 9121660. PMID 35593162.
- "WHO launches global network to detect and prevent infectious disease threats". World Health Organization. 20 May 2023. Retrieved 17 August 2023.
- "Bill & Melinda Gates Foundation and Wellcome pledge $300 million to CEPI". CEPI. 19 January 2022. Retrieved 20 August 2023.
- "Delivering pandemic vaccines in 100 days - what will it take?". Coalition for Epidemic Preparedness Innovations. 2022.
- "Pandemic Preparedness". NIH: National Institute of Allergy and Infectious Diseases. December 2021. Retrieved 21 August 2023.
- "NIAID Pandemic Preparedness Plan (pdf)" (PDF). National Institute of Allergy and Infectious Diseases. December 2021. Retrieved 21 August 2023.
- "Technical report on the COVID-19 pandemic in the UK - Chapter 5: modelling". Department of Health & Social Care. 1 December 2022. Retrieved 21 August 2023.
- Bellantoni A, Badr K, Alfonsi C (3 July 2020). Transparency, communication and trust: The role of public communication in responding to the wave of disinformation about the new Coronavirus (Report). OECD Policy Responses to Coronavirus (COVID-19). Organisation for Economic Co-operation and Development. doi:10.1787/bef7ad6e-en. Retrieved 21 August 2023.
- Lovelace Jr B, Bauer T, Torres J (28 July 2022). "A rare look inside the Strategic National Stockpile — and how it went wrong at the start of the pandemic". NBC News. Retrieved 21 August 2023.
- Anderson RM, Heesterbeek H, Klinkenberg D, Hollingsworth TD (March 2020). "How will country-based mitigation measures influence the course of the COVID-19 epidemic?". Lancet. 395 (10228): 931–934. doi:10.1016/S0140-6736(20)30567-5. PMC 7158572. PMID 32164834.
A key issue for epidemiologists is helping policymakers decide the main objectives of mitigation—e.g., minimizing morbidity and associated mortality, avoiding an epidemic peak that overwhelms health-care services, keeping the effects on the economy within manageable levels, and flattening the epidemic curve to wait for vaccine development and manufacture on the scale and antiviral drug therapies.
- "Community Mitigation Guidelines to Prevent Pandemic Influenza—United States, 2017". Recommendations and Reports. Centers for Disease Control and Prevention. 66 (1). 12 April 2017.
- Barclay E, Scott D, Animashaun A (7 April 2020). "The US doesn't just need to flatten the curve. It needs to "raise the line."". Vox. Archived from the original on 7 April 2020.
- Stawicki SP, Jeanmonod R, Miller AC, Paladino L, Gaieski DF, Yaffee AQ, et al. (2020). "The 2019–2020 Novel Coronavirus (Severe Acute Respiratory Syndrome Coronavirus 2) Pandemic: A Joint American College of Academic International Medicine-World Academic Council of Emergency Medicine Multidisciplinary COVID-19 Working Group Consensus Paper". Journal of Global Infectious Diseases. 12 (2): 47–93. doi:10.4103/jgid.jgid_86_20. PMC 7384689. PMID 32773996. S2CID 218754925.
- Anderson RM, Heesterbeek H, Klinkenberg D, Hollingsworth TD (March 2020). "How will country-based mitigation measures influence the course of the COVID-19 epidemic?". Lancet. 395 (10228): 931–934. doi:10.1016/S0140-6736(20)30567-5. PMC 7158572. PMID 32164834.
- Maier BF, Brockmann D (May 2020). "Effective containment explains subexponential growth in recent confirmed COVID-19 cases in China". Science. 368 (6492): 742–746. arXiv:2002.07572. Bibcode:2020Sci...368..742M. doi:10.1126/science.abb4557. PMC 7164388. PMID 32269067. ("...initial exponential growth expected for an unconstrained outbreak.")
- "Gauze Mask to Halt Spread of Plague". The Washington Times. 27 September 1918. p. 3.
- "3. Strategies for Disease Containment". Ethical and Legal Considerations in Mitigating Pandemic Disease: Workshop Summary. National Academies Press (US). 2007.
- Baird RP (11 March 2020). "What It Means to Contain and Mitigate the Coronavirus". The New Yorker.
- "Impact of non-pharmaceutical interventions (NPIs) to reduce COVID19 mortality and healthcare demand" (PDF). Imperial College COVID-19 Response Team. 16 March 2020.
- Pandemic influenza preparedness and response: a WHO guidance document (PDF). World Health Organization. 2009. pp. 24–27. ISBN 978-92-4-154768-0. Retrieved 17 August 2023.
- "WHO says it no longer uses 'pandemic' category, but virus still emergency". Reuters. 24 February 2020. Archived from the original on 18 March 2020.
For the sake of clarification, WHO does not use the old system of 6 phases—that ranged from phase 1 (no reports of animal influenza causing human infections) to phase 6 (a pandemic)—that some people may be familiar with from H1N1 in 2009.
- Holloway R, Rasmussen SA, Zaza S, Cox NJ, Jernigan DB (September 2014). "Updated preparedness and response framework for influenza pandemics" (PDF). MMWR. Recommendations and Reports. Center for Surveillance, Epidemiology, and Laboratory Services, Centers for Disease Control and Prevention. 63 (RR-06): 1–18. PMID 25254666. Retrieved 10 May 2020.
- Reed C, Biggerstaff M, Finelli L, Koonin LM, Beauvais D, Uzicanin A, et al. (January 2013). "Novel framework for assessing epidemiologic effects of influenza epidemics and pandemics". Emerging Infectious Diseases. 19 (1): 85–91. doi:10.3201/eid1901.120124. PMC 3557974. PMID 23260039.
- Bhatia R, Sledge I, Baral S (12 October 2022). "Missing science: A scoping study of COVID-19 epidemiological data in the United States". PLOS ONE. 17 (10): e0248793. doi:10.1371/journal.pone.0248793. PMC 9555641. PMID 36223335.
- "Total confirmed cases of COVID-19 per million people". Our World in Data. Archived from the original on 19 March 2020. Retrieved 10 April 2020.
- "WHO Statement Regarding Cluster of Pneumonia Cases in Wuhan, China". WHO. 31 December 2019. Retrieved 12 March 2020.
- "WHO Director-General's opening remarks at the media briefing on COVID-19—11 March 2020". WHO. 11 March 2020. Retrieved 12 March 2020.
- "WHO – Statement on the fifteenth meeting of the IHR (2005) Emergency Committee on the COVID-19 pandemic". World Health Organization. Retrieved 10 May 2023.
- "WHO Coronavirus (COVID-19) Dashboard". World Health Organization. 19 June 2023. Retrieved 19 June 2023.
- Harrison CM, Doster JM, Landwehr EH, Kumar NP, White EJ, Beachboard DC, Stobart CC (February 2023). "Evaluating the Virology and Evolution of Seasonal Human Coronaviruses Associated with the Common Cold in the COVID-19 Era". Microorganisms. 11 (2): 445. doi:10.3390/microorganisms11020445. PMC 9961755. PMID 36838410.
After evaluating the biology, pathogenesis, and emergence of the human coronaviruses that cause the common cold, we can anticipate that with increased vaccine immunity to SARS-CoV-2, it will become a seasonal, endemic coronavirus that causes less severe disease in most individuals. Much like the common cold CoVs, the potential for severe disease will likely be present in those who lack a protective immune response or are immunocompromised.
- "HIV/AIDS Factsheet". World Health Organization. 2 August 2023. Retrieved 2 August 2023.
- "Why the HIV epidemic is not over". www.who.int. Retrieved 11 March 2022.
- Sharp PM, Hahn BH (September 2011). "Origins of HIV and the AIDS pandemic". Cold Spring Harbor Perspectives in Medicine. 1 (1): a006841. doi:10.1101/cshperspect.a006841. PMC 3234451. PMID 22229120.
- "What Are HIV and AIDS?". HIV.gov. U.S. Department of Health & Human Services. 15 May 2017. Retrieved 2 August 2023.
- "HIV Treatment: The Basics | NIH". hivinfo.nih.gov (a service of the U.S. Department of Health and Human Services). 16 August 2021. Retrieved 2 August 2023.
- Alchon S (2003). A Pest in the Land: New World Epidemics in a Global Perspective. University of New Mexico Press. p. 62. ISBN 978-0-8263-2871-7. Retrieved 9 March 2019.
- Hauck G (22 November 2020). "We're celebrating Thanksgiving amid a pandemic. Here's how we did it in 1918 – and what happened next". USA Today. Graphics by Karl Gelles. Archived from the original on 21 November 2020.
- Høiby N (July 2021). "Pandemics: past, present, future: That is like choosing between cholera and plague". APMIS. 129 (7): 352–371. doi:10.1111/apm.13098. PMC 7753327. PMID 33244837.
- "Ancient Athenian Plague Proves to Be Typhoid". Scientific American. 25 January 2006.
- Past pandemics that ravaged Europe. BBC News, 7 November. 2005
- Horgan J. "Plague of Cyprian, 250–270 CE". World History Encyclopedia. Retrieved 16 July 2023.
- "Modern lab reaches across the ages to resolve plague DNA debate". phys.org. 20 May 2013.
- Little LK (2007). Plague and the end of Antiquity: the pandemic of 541-750. Cambridge (Mass.): Cambridge University Press. ISBN 978-0-521-84639-4.
- Death on a Grand Scale. MedHunters.
- Stéphane Barry and Norbert Gualde, in L'Histoire No. 310, June 2006, pp. 45–46, say "between one-third and two-thirds"; Robert Gottfried (1983). "Black Death" in Dictionary of the Middle Ages, volume 2, pp. 257–267, says "between 25 and 45 percent".
- Chisholm, Hugh, ed. (1911). . Encyclopædia Britannica. Vol. 21 (11th ed.). Cambridge University Press. pp. 693–705.
- "A List of National Epidemics of Plague in England 1348–1665". Urbanrim.org.uk. 4 August 2010. Archived from the original on 8 May 2009. Retrieved 26 August 2010.
- Revill J (16 May 2004). "Black Death blamed on man, not rats". The Observer. London. Retrieved 3 November 2008.
- The Great Plague of London, 1665. The Harvard University Library, Open Collections Program: Contagion.
- Cholera's seven pandemics Archived 2008-05-13 at the Wayback Machine, cbc.ca, December 2, 2008.
- "Cholera - Pandemic, Waterborne, 19th Century | Britannica". www.britannica.com. Retrieved 27 August 2023.
- Pollitzer, R. (1954). "Cholera studies". Bulletin of the World Health Organization. 10 (3): 421–461. ISSN 0042-9686. PMC 2542143. PMID 13160764.
- McNeill, William Hardy (1998). Plagues and peoples (Reprint [der Ausg.] Garden City, NY, 1976 ed.). New York: Anchor Books. ISBN 978-0-385-12122-4.
- "History's Seven Deadliest Plagues | Gavi, the Vaccine Alliance". www.gavi.org. Retrieved 16 July 2023.
- "Zoonotic Infections: Plague". World Health Organization. Archived from the original on 20 April 2009. Retrieved 5 July 2014.
- Bubonic plague hits San Francisco 1900–1909. A Science Odyssey. Public Broadcasting Service (PBS).
- Yersin A (1894). "La peste bubonique à Hong-Kong". Annales de l'Institut Pasteur (in French). 8: 662–67.
- "Plague". World Health Organization. 7 July 2022. Retrieved 16 July 2023.
- Taubenberger JK, Morens DM (January 2006). "1918 Influenza: the mother of all pandemics". Emerging Infectious Diseases. 12 (1): 15–22. doi:10.3201/eid1201.050979. PMC 3291398. PMID 16494711. Archived from the original on 6 October 2009. Retrieved 7 September 2017.
- "Historical Estimates of World Population". Archived from the original on 9 July 2012. Retrieved 29 March 2013.
- Gagnon A, Miller MS, Hallman SA, Bourbeau R, Herring DA, Earn DJ, Madrenas J (2013). "Age-specific mortality during the 1918 influenza pandemic: unravelling the mystery of high young adult mortality". PLOS ONE. 8 (8): e69586. Bibcode:2013PLoSO...869586G. doi:10.1371/journal.pone.0069586. PMC 3734171. PMID 23940526.
- "The 1918 Influenza Pandemic". virus.stanford.edu.
- Spanish flu facts | work = Channel 4 News.
- Qureshi AI (2016). Ebola Virus Disease: From Origin to Outbreak. Academic Press. p. 42. ISBN 978-0128042427.
- Spanish flu strikes during World War I, 14 January 2010
- "The Story Of ... Smallpox—and other Deadly Eurasian Germs". Pbs.org. Retrieved 26 August 2010.
- "Stacy Goodling, "Effects of European Diseases on the Inhabitants of the New World"". Archived from the original on 10 May 2008.
- Francis JM (2005). Iberia and the Americas culture, politics, and history: A Multidisciplinary Encyclopedia. Santa Barbara, California: ABC-CLIO. ISBN 1851094210.
- Hays J (2005). Epidemics and Pandemics: Their Impacts on Human History. Bloomsbury Publishing. ISBN 9781851096589.
- Gunderman R (19 February 2019). "How smallpox devastated the Aztecs – and helped Spain conquer an American civilization 500 years ago". The Conversation. Retrieved 1 December 2022.
- Koch A (1 December 2019). "'Great Dying' in Americas disturbed Earth's climate". University College London – News. Retrieved 26 July 2023.
- "500 years later, scientists discover what probably killed the Aztecs". The Guardian. AFP. 18 January 2018. Retrieved 16 January 2018.
- Dowling P (2021). Fatal contact: How epidemics nearly wiped out Australia's first peoples. Clayton, Victoria: Monash University Publishing. pp. 30–31, 60–63. ISBN 9781922464460.
- "New Zealand Historical Perspective". Canr.msu.edu. 31 March 1998. Archived from the original on 12 June 2010. Retrieved 26 August 2010.
- Derrick RA (18 April 1955). "Fiji's darkest hour – an account of the Measles Epidemic of 1875" (PDF). Transactions and Proceedings of the Fiji Society. for the years 1955–1957: 6(1): 3–16.
- "Measles hits rare Andaman tribe". BBC News. 16 May 2006.
- Walker BL (2001). The Conquest of Ainu Lands: Ecology and Culture in Japanese Expansion, 1590–1800. University of California Press. ISBN 978-0-520-93299-9.
- "Selecting Viruses for the Seasonal Flu Vaccine". Centers for Disease Control and Prevention. 3 November 2022. Retrieved 30 June 2023.
- "WHO official: 'Next pandemic may be more severe'". Arab News. 29 December 2020. Retrieved 30 December 2020.
- Carrington D (9 March 2021). "Inaction leaves world playing 'Russian roulette' with pandemics, say experts". The Guardian. Retrieved 10 March 2021.
- "Prioritizing diseases for research and development in emergency contexts (Published 2018, revision in progress 2023)". World Health Organization. Retrieved 23 June 2023.
- "Targeting diseases with epidemic and pandemic potential". CEPI, Coalition for Epidemic Preparedness Innovations. 23 June 2023. Retrieved 23 June 2023.
- "10 infectious diseases that could be the next pandemic | Gavi, the Vaccine Alliance". Gavi, the Vaccine Alliance. 7 May 2020. Retrieved 23 June 2023.
- Berche P (September 2022). "The enigma of the 1889 Russian flu pandemic: A coronavirus?". Presse Médicale. 51 (3): 104111. doi:10.1016/j.lpm.2022.104111. PMC 8813723. PMID 35124103.
- Kolata, Gina (14 February 2022). "An Undiscovered Coronavirus? The Mystery of the 'Russian Flu' (Published 2022)". The New York Times. Retrieved 29 July 2023.
- Heymann D, Ross E, Wallace J (23 February 2022). "The next pandemic – when could it be?". Chatham House, The Royal Institute of International Affairs. Retrieved 24 July 2023.
- Forni D, Cagliani R, Clerici M, Sironi M (January 2017). "Molecular Evolution of Human Coronavirus Genomes". Trends in Microbiology. 25 (1): 35–48. doi:10.1016/j.tim.2016.09.001. PMC 7111218. PMID 27743750.
Specifically, all HCoVs are thought to have a bat origin, with the exception of lineage A beta-CoVs, which may have reservoirs in rodents [2].
- Holmes EC (March 2022). "COVID-19-lessons for zoonotic disease". Science. 375 (6585): 1114–1115. doi:10.1126/science.abn2222. PMID 35271309. S2CID 247384213.
- "Swine flu has killed up to 17,000 in U.S.: report". Reuters. 12 February 2010.
- "50 Years of Influenza Surveillance". World Health Organization. Archived from the original on 1 May 2009.
- Potter CW (October 2001). "A history of influenza". Journal of Applied Microbiology. 91 (4): 572–579. doi:10.1046/j.1365-2672.2001.01492.x. PMID 11576290. S2CID 26392163.
- "How Flu Viruses Can Change". Centers for Disease Control and Prevention. 12 December 2022. Retrieved 12 July 2023.
- "Key Facts About Influenza (Flu)". Centers for Disease Control and Prevention. 2 May 2023. Retrieved 12 July 2023.
- "Influenza (Seasonal)". World Health Organization. Retrieved 12 July 2023.
- Shally-Jensen M, ed. (2010). "Influenza". Encyclopedia of Contemporary American Social Issues. Vol. 2. ABC-CLIO. p. 1510. ISBN 978-0-31339205-4.
The Asiatic flu killed roughly one million individuals
- Lee K, Fang J (2013). Historical Dictionary of the World Health Organization. Rowman & Littlefield. ISBN 9780810878587.
- Broor S, Campbell H, Hirve S, Hague S, Jackson S, Moen A, et al. (November 2020). "Leveraging the Global Influenza Surveillance and Response System for global respiratory syncytial virus surveillance-opportunities and challenges". Influenza and Other Respiratory Viruses. 14 (6): 622–629. doi:10.1111/irv.12672. PMC 7578328. PMID 31444997.
 This article incorporates text available under the CC BY 4.0 license.
This article incorporates text available under the CC BY 4.0 license. - "Researchers sound the alarm: the multidrug resistance of the plague bacillus could spread". Pasteur.fr. Archived from the original on 14 October 2007.
- Health ministers to accelerate efforts against drug-resistant TB. World Health Organization.
- Bill Gates joins Chinese government in tackling TB 'timebomb'. Guardian.co.uk. 1 April 2009
- "Global Tuberculosis Report". World Health Organization. Retrieved 30 June 2023.
- Murray CJ, Ikuta KS, Sharara F, Swetschinski L, Aguilar GR, Gray A, et al. (Antimicrobial Resistance Collaborators) (February 2022). "Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis". Lancet. 399 (10325): 629–655. doi:10.1016/S0140-6736(21)02724-0. PMC 8841637. PMID 35065702. S2CID 246077406.
- Intergovernmental Panel on Climate Change (IPCC) (29 June 2023). Climate Change 2022 – Impacts, Adaptation and Vulnerability: Working Group II Contribution to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change (1 ed.). Cambridge University Press. pp. 1041–1170. doi:10.1017/9781009325844.009. ISBN 978-1-009-32584-4.
- Epstein PR, Ferber D (2011). "The Mosquito's Bite". Changing Planet, Changing Health: How the Climate Crisis Threatens Our Health and what We Can Do about it. University of California Press. pp. 29–61. ISBN 978-0-520-26909-5.
- Jung YJ, Khant NA, Kim H, Namkoong S (January 2023). "Impact of Climate Change on Waterborne Diseases: Directions towards Sustainability". Water. 15 (7): 1298. doi:10.3390/w15071298. ISSN 2073-4441.
- Woolaston K, Fisher JL (29 October 2020). "UN report says up to 850,000 animal viruses could be caught by humans, unless we protect nature". The Conversation. Retrieved 1 December 2020.
- Carrington D (29 October 2020). "Protecting nature is vital to escape 'era of pandemics' – report". The Guardian. Retrieved 1 December 2020.
- "Escaping the 'Era of Pandemics': experts warn worse crises to come; offer options to reduce risk". EurekAlert!. 29 October 2020. Retrieved 1 December 2020.
- Carrington D (4 June 2021). "World leaders 'ignoring' role of the destruction of nature in causing pandemics". The Guardian. Retrieved 4 June 2021.
- "Global Health Risk Framework—The Neglected Dimension of Global Security: A Framework to Counter Infectious Disease Crises" (PDF). National Academy of Medicine. 16 January 2016. Retrieved 2 August 2016.
- World Bank Group (September 2019). Pandemic Preparedness Financing. Status Update (PDF). Washington: World Bank Group. Archived from the original (PDF) on 1 March 2020.
- Pueyo S (12 May 2020). "Jevons' paradox and a tax on aviation to prevent the next pandemic". SocArXiv. doi:10.31235/osf.io/vb5q3. S2CID 219809283.
- Wang L, Wu JT (January 2018). "Characterizing the dynamics underlying global spread of epidemics". Nature Communications. 9 (1): 218. Bibcode:2018NatCo...9..218W. doi:10.1038/s41467-017-02344-z. PMC 5768765. PMID 29335536.
- Le Quéré C, Jackson RB, Jones MW, Smith AJ, Abernethy S, Andrew RM, et al. (2020). "Temporary reduction in daily global CO2 emissions during the COVID-19 forced confinement". Nature Climate Change. 10 (7): 647–653. Bibcode:2020NatCC..10..647L. doi:10.1038/s41558-020-0797-x.
- "Pollution made COVID-19 worse. Now, lockdowns are clearing the air". National Geographic Magazine. 8 April 2020. Retrieved 22 June 2020.
- Bauwens M, Compernolle S, Stavrakou T, Müller JF, van Gent J, Eskes H, et al. (June 2020). "Impact of Coronavirus Outbreak on NO2 Pollution Assessed Using TROPOMI and OMI Observations". Geophysical Research Letters. 47 (11): e2020GL087978. Bibcode:2020GeoRL..4787978B. doi:10.1029/2020GL087978. PMC 7261997. PMID 32836515.
- "The Black Death helped reveal how long humans have polluted the planet". Popular Science Magazine. 25 September 2017. Retrieved 22 June 2020.
Further reading
- American Lung Association (April 2007). "Multidrug Resistant Tuberculosis Fact Sheet". Archived from the original on 30 November 2006. Retrieved 29 November 2007.
- Bancroft EA (October 2007). "Antimicrobial resistance: it's not just for hospitals". JAMA. 298 (15): 1803–1804. doi:10.1001/jama.298.15.1803. PMC 2536104. PMID 17940239.
- Brilliant L, Smolinski M, Danzig L, Lipkin WI (January–February 2023). "Inevitable Outbreaks: How to Stop an Age of Spillovers from Becoming an Age of Pandemics". Foreign Affairs. 102 (1): 126–130, 132–140.
- Brook T (November 2020). "Comparative pandemics: the Tudor–Stuart and Wanli–Chongzhen years of pestilence, 1567–1666". Journal of Global History. 15 (3): 363–379. doi:10.1017/S174002282000025X. S2CID 228979855.
- Eisenberg M, Mordechai L (December 2020). "The Justinianic plague and global pandemics: The making of the plague concept". The American Historical Review. 125 (5): 1632–1667. doi:10.1093/ahr/rhaa510.
- Honigsbaum M (18 October 2020). "How do pandemics end? In different ways, but it's never quick and never neat". The Guardian. ISSN 0261-3077. Retrieved 28 October 2020.
- Larson E (2007). "Community factors in the development of antibiotic resistance". Annual Review of Public Health. 28: 435–447. doi:10.1146/annurev.publhealth.28.021406.144020. PMID 17094768.
- Lietaert Peerbolte BJ (September 2021). "The Book of Revelation: Plagues as Part of the Eschatological Human Condition". Journal for the Study of the New Testament. SAGE Publications. 44 (1): 75–92. doi:10.1177/0142064X211025496. ISSN 1745-5294. S2CID 237332665.
- McKenna N (September 2020). "Return of the Germs: For more than a century drugs and vaccines made astounding progress against infectious diseases. Now our best defenses may be social changes". Scientific American. 323 (3): 50–56.
What might prevent or lessen [the] possibility [of a virus emerging and finding a favorable human host] is more prosperity more equally distributed – enough that villagers in South Asia need not trap and sell bats to supplement their incomes and that, low-wage workers in the U.S. need not go to work while ill because they have no sick leave
- Quammen D (24 August 202). "Did Pangolin Trafficking Cause the Coronavirus Pandemic". The New Yorker. pp. 26–31 (31).
More field research is needed [...]. More sampling of wild animals. More scrutiny of genomes. More cognizance of the fact that animal infections can become human infections because humans are animals. We live in a world of viruses, and we have scarcely begun to understand this one. [ COVID-19
- "Escaping the 'Era of Pandemics': Experts Warn Worse Crises to Come Options Offered to Reduce Risk". Intergovernmental Science-Policy Platform on Biodiversity and Ecosystem Services. 2020.


.gif)


_-_The_Washington_Times.jpg.webp)