Actinic keratosis
Actinic keratosis (AK), sometimes called solar keratosis or senile keratosis,[1][2] is a pre-cancerous[3] area of thick, scaly, or crusty skin.[4][5] Actinic keratosis is a disorder (-osis) of epidermal keratinocytes that is induced by ultraviolet (UV) light exposure (actin-).[6] These growths are more common in fair-skinned people and those who are frequently in the sun.[7] They are believed to form when skin gets damaged by UV radiation from the sun or indoor tanning beds, usually over the course of decades. Given their pre-cancerous nature, if left untreated, they may turn into a type of skin cancer called squamous cell carcinoma.[5] Untreated lesions have up to a 20% risk of progression to squamous cell carcinoma,[8] so treatment by a dermatologist is recommended.
| Actinic keratosis | |
|---|---|
| Other names | Solar keratosis, senile keratosis (SK) |
 | |
| Actinic keratosis seen on the back of the hands | |
| Specialty | Dermatology |
Actinic keratoses characteristically appear as thick, scaly, or crusty areas that often feel dry or rough. Size commonly ranges between 2 and 6 millimeters, but they can grow to be several centimeters in diameter. Notably, AKs are often felt before they are seen, and the texture is sometimes compared to sandpaper.[9] They may be dark, light, tan, pink, red, a combination of all these, or have the same color as the surrounding skin.
Given the causal relationship between sun exposure and AK growth, they often appear on a background of sun-damaged skin and in areas that are commonly sun-exposed, such as the face, ears, neck, scalp, chest, backs of hands, forearms, or lips. Because sun exposure is rarely limited to a small area, most people who have an AK have more than one.[10]
If clinical examination findings are not typical of AK and the possibility of in situ or invasive squamous cell carcinoma (SCC) cannot be excluded based on clinical examination alone, a biopsy or excision can be considered for definitive diagnosis by histologic examination of the lesional tissue.[11] Multiple treatment options for AK are available. Photodynamic therapy (PDT) is one option the treatment of numerous AK lesions in a region of the skin, termed field cancerization.[12] It involves the application of a photosensitizer to the skin followed by illumination with a strong light source. Topical creams, such as 5-fluorouracil or imiquimod, may require daily application to affected skin areas over a typical time course of weeks.[13]
Cryotherapy is frequently used for few and well-defined lesions,[14] but undesired skin lightening, or hypopigmentation, may occur at the treatment site.[15] By following up with a dermatologist, AKs can be treated before they progress to skin cancer. If cancer does develop from an AK lesion, it can be caught early with close monitoring, at a time when treatment is likely to have a high cure rate.
Signs and symptoms


Actinic keratoses (AKs) most commonly present as a white, scaly plaque of variable thickness with surrounding redness; they are most notable for having a sandpaper-like texture when felt with a gloved hand. Skin nearby the lesion often shows evidence of solar damage characterized by notable pigmentary alterations, being yellow or pale in color with areas of hyperpigmentation; deep wrinkles, coarse texture, purpura and ecchymoses, dry skin, and scattered telangiectasias are also characteristic.[16]
Photoaging leads to an accumulation of oncogenic changes, resulting in a proliferation of mutated keratinocytes that can manifest as AKs or other neoplastic growths.[17] With years of sun damage, it is possible to develop multiple AKs in a single area on the skin. This condition is termed field cancerization.
The lesions are usually asymptomatic, but can be tender, itch, bleed, or produce a stinging or burning sensation.[18] AKs are typically graded in accordance with their clinical presentation: Grade I (easily visible, slightly palpable), Grade II (easily visible, palpable), and Grade III (frankly visible and hyperkeratotic).[19]
Variants

Actinic keratoses can have various clinical presentations, often characterized as follows:
- Classic (or common): Classic AKs present as white, scaly macules, papules or plaques of various thickness, often with surrounding erythema. They are usually 2–6mm in diameter but can sometimes reach several centimeters in diameter.[18]
- Hypertrophic (or hyperkeratotic): Hypertrophic AKs (HAKs) appears as a thicker scale or rough papule or plaque, often adherent to an erythematous base. Classic AKs can progress to become HAKs, and HAKs themselves can be difficult to distinguish from malignant lesions.
- Atrophic: Atrophic AKs lack an overlying scale, and therefore appear as a nonpalpable change in color (or macule). They are often smooth and red and are less than 10mm in diameter.
- AK with cutaneous horn: A cutaneous horn is a keratinic projection with its height at least one-half of its diameter, often conical in shape. They can be seen in the setting of actinic keratosis as a progression of an HAK, but are also present in other skin conditions.[18] 38–40% of cutaneous horns represent AKs.[20]
- Pigmented AK: Pigmented AKs are rare variants that often present as macules or plaques that are tan to brown in color. They can be difficult to distinguish from a solar lentigo or lentigo maligna.[21]
- Actinic cheilitis: When an AK forms on the lip, it is called actinic cheilitis. This usually presents as a rough, scaly patch on the lip, often accompanied by the sensation of dry mouth and symptomatic splitting of the lips.
- Bowenoid AK: Usually presents as a solitary, erythematous, scaly patch or plaque with well-defined borders. Bowenoid AKs are differentiated from Bowen's disease by degree of epithelial involvement as seen on histology.[22]
The presence of ulceration, nodularity, or bleeding should raise concern for malignancy.[23] Specifically, clinical findings suggesting an increased risk of progression to squamous cell carcinoma can be recognized as "IDRBEU": I (induration/inflammation), D (diameter > 1 cm), R (rapid enlargement), B (bleeding), E (erythema), and U (ulceration).[24] AKs are usually diagnosed clinically, but because they are difficult to clinically differentiate from squamous cell carcinoma, any concerning features warrant biopsy for diagnostic confirmation.[25]
Causes
The most important cause of AK formation is solar radiation, through a variety of mechanisms. Mutation of the p53 tumor suppressor gene, induced by UV radiation, has been identified as a crucial step in AK formation.[26] This tumor suppressor gene, located on chromosome 17p132, allows for cell cycle arrest when DNA or RNA is damaged. Dysregulation of the p53 pathway can thus result in unchecked replication of dysplastic keratinocytes, thereby serving as a source of neoplastic growth and the development of AK, as well as possible progression from AK to skin cancer.[27] Other molecular markers that have been associated with the development of AK include the expression of p16ink4, p14, the CD95 ligand, TNF-related apoptosis-inducing ligand (TRAIL) and TRAIL receptors, and loss of heterozygosity.[28][27]
Evidence also suggests that the human papillomavirus (HPV) plays a role in the development of AKs. The HPV virus has been detected in AKs, with measurable HPV viral loads (one HPV-DNA copy per less than 50 cells) measured in 40% of AKs.[29] Similar to UV radiation, higher levels of HPV found in AKs reflect enhanced viral DNA replication. This is suspected to be related to the abnormal keratinocyte proliferation and differentiation in AKs, which facilitate an environment for HPV replication. This in turn may further stimulate the abnormal proliferation that contributes to the development of AKs and carcinogenesis.
Ultraviolet radiation
It is thought that ultraviolet (UV) radiation induces mutations in the keratinocytes of the epidermis, promoting the survival and proliferation of these atypical cells. Both UV-A and UV-B radiation have been implicated as causes of AKs. UV-A radiation (wavelength 320–400 nm) reaches more deeply into the skin and can lead to the generation of reactive oxygen species, which in turn can damage cell membranes, signaling proteins, and nucleic acids. UV-B radiation (wavelength 290–320 nm) causes thymidine dimer formation in DNA and RNA, leading to significant cellular mutations.[30] In particular, mutations in the p53 tumor suppressor gene have been found in 30–50% of AK lesion skin samples.[26][28]
UV radiation has also been shown to cause elevated inflammatory markers such as arachidonic acid, as well as other molecules associated with inflammation.[27] Eventually, over time these changes lead to the formation of AKs. Several predictors for increased AK risk from UV radiation have been identified:
- Extent of sun exposure: Cumulative sun exposure leads to an increased risk for development of AKs. In one U.S. study, AKs were found in 55% of fair-skinned men with high cumulative sun exposure, and in only 19% of fair-skinned men with low cumulative sun exposure in an age-matched cohort (the percents for women in this same study were 37% and 12% respectively).[31] Furthermore, the use of sunscreen (SPF 17 or higher) has been found to significantly reduce the development of AK lesions, and also promotes the regression of existing lesions.[32]
- History of sunburn: Studies show that even a single episode of painful sunburn as a child can increase an individual's risk of developing AK as an adult.[33] Six or more painful sunburns over the course of a lifetime was found to be significantly associated with the likelihood of developing AK.[33]
Skin pigmentation

Melanin is a pigment in the epidermis that functions to protect keratinocytes from the damage caused by UV radiation; it is found in higher concentrations in the epidermis of darker-skinned individuals, affording them protection against the development of AKs.
Fair-skinned individuals have a significantly increased risk of developing AKs when compared to olive-skinned individuals (odds ratios of 14.1 and 6.5, respectively),[33] and AKs are uncommon in dark-skinned people of African descent.[31] Other phenotypic features seen in fair-skinned individuals that are associated with an increased propensity to develop AKs include:[31]
Other risk factors
- Immunosuppression: People with a compromised immune system from medical conditions (such as AIDS) or immunosuppressive therapy (such as chronic immunosuppression after organ transplantation, or chemotherapy for cancer) are at increased risk for developing AKs.[34] They may develop AK at an earlier age or have an increased number of AK lesions compared to immunocompetent people.[35]
- Human papillomavirus (HPV): The role of HPV in the development of AK remains unclear, but evidence suggests that infection with the betapapillomavirus type of HPV may be associated with an increased likelihood of AK.[36]
- Genodermatoses: Certain genetic disorders interfere with DNA repair after sun exposure, thereby putting these individuals at higher risk for the development of AKs. Examples of such genetic disorders include xeroderma pigmentosum and Bloom syndrome.
- Balding: AKs are commonly found on the scalps of balding men. The degree of baldness seems to be a risk factor for lesion development, as men with severe baldness were found to be seven times more likely to have 10 or more AKs when compared to men with minimal or no baldness.[37] This observation can be explained by an absence of hair causing a larger proportion of scalp to be exposed to UV radiation if other sun protection measures are not taken.
Diagnosis

Physicians usually diagnose actinic keratosis by doing a thorough physical examination, through a combination of visual observation and touch. However a biopsy may be necessary when the keratosis is large in diameter, thick, or bleeding, in order to make sure that the lesion is not a skin cancer. Actinic keratosis may progress to invasive squamous cell carcinoma (SCC) but both diseases can present similarly upon physical exam and can be difficult to distinguish clinically.[6] Histological examination of the lesion from a biopsy or excision may be necessary to definitively distinguish AK from in situ or invasive SCC.[6] In addition to SCCs, AKs can be mistaken for other cutaneous lesions including seborrheic keratoses, basal cell carcinoma, lichenoid keratosis, porokeratosis, viral warts, erosive pustular dermatosis of the scalp, pemphigus foliaceus, inflammatory dermatoses like psoriasis, or melanoma.[38]
Biopsy
A lesion biopsy is performed if the diagnosis remains uncertain after a clinical physical exam, or if there is suspicion that the AK might have progressed to squamous cell carcinoma. The most common tissue sampling techniques include shave or punch biopsy. When only a portion of the lesion can be removed due to its size or location, the biopsy should sample tissue from the thickest area of the lesion, as SCCs are most likely to be detected in that area.
If a shave biopsy is performed, it should extend through to the level of the dermis in order to provide sufficient tissue for diagnosis; ideally, it would extend to the mid-reticular dermis. Punch biopsy usually extends to the subcutaneous fat when the entire length of the punch blade is utilized.
Histopathology
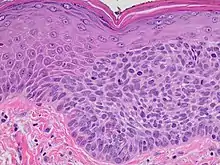
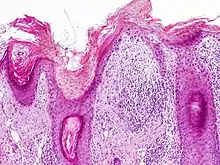
On histologic examination, actinic keratoses usually show a collection of atypical keratinocytes with hyperpigmented or pleomorphic nuclei, extending to the basal layer of the epidermis. A "flag sign" is often described, referring to alternating areas of orthokeratosis and parakeratosis. Epidermal thickening and surrounding areas of sun-damaged skin are often seen.[39] The normal ordered maturation of the keratinocytes is disordered to varying degrees: there may be widening of the intracellular spaces, cytologic atypia such as abnormally large nuclei, and a mild chronic inflammatory infiltrate.[40]
Specific findings depend on the clinical variant and particular lesion characteristics. The seven major histopathologic variants are all characterized by atypical keratinocytic proliferation beginning in the basal layer and confined to the epidermis; they include:[39]
- Hypertrophic: Notable for marked hyperkeratosis, often with evident parakeratosis.[39] Keratinocytes in the stratum malphigii may show a loss of polarity, pleomorphism, and anaplasia.[25] Some irregular downward proliferation into the uppermost dermis may be observed, but does not represent frank invasion.[25]
- Atrophic: With slight hyperkeratosis and overall atrophic changes to the epidermis; the basal layer shows cells with large, hyperchromatic nuclei in close proximity to each other. These cells have been observed to proliferate into the dermis as buds and duct-like structures.[25]
- Lichenoid: Demonstrate a band-like lymphocytic infiltrate in the papillary dermis, directly beneath the dermal-epidermal junction.[39]
- Achantholytic: Intercellular clefts or lacunae in the lowermost epidermal layer that result from anaplastic changes; these produce dyskeratotic cells with disrupted intercellular bridges.
- Bowenoid: This term is controversial and usually refers to full-thickness atypia, microscopically indistinguishable from Bowen's Disease.[25] However most dermatologists and pathologists will use it in reference to tissue samples that are notable for small foci of atypia that involve the full thickness of the epidermis, in the background of a lesion that is otherwise consistent with an AK.[39]
- Epidermolytic: With granular degeneration.[25]
- Pigmented: Show pigmentation in the basal layer of the epidermis, similar to a solar lentigo.[39]
Dermoscopy
Dermoscopy is a noninvasive technique utilizing a handheld magnifying device coupled with a transilluminating lift. It is often used in the evaluation of cutaneous lesions but lacks the definitive diagnostic ability of biopsy-based tissue diagnosis. Histopathologic exam remains the gold standard.
Polarized contact dermoscopy of AKs occasionally reveals a "rosette sign," described as four white points arranged in a clover pattern, often localized to within a follicular opening.[41] It is hypothesized that the "rosette sign" corresponds histologically to the changes of orthokeratosis and parakeratosis known as the "flag sign."[41]
- Non-pigmented AKs: linear or wavy vascular patterning, or a "strawberry pattern," described as unfocused vessels between hair follicles, with white-haloed follicular openings.[42]
- Pigmented AKs: gray to brown dots or globules surrounding follicular openings, and annular-granular rhomboidal structures; often difficult to differentiate from lentigo maligna.[43]
Prevention
Ultraviolet radiation is believed to contribute to the development of actinic keratoses by inducing mutations in epidermal keratinocytes, leading to proliferation of atypical cells.[44] Therefore, preventive measures for AKs are targeted at limiting exposure to solar radiation, including:
- Limiting extent of sun exposure
- Avoid sun exposure during noontime hours between 10:00 AM and 2:00 PM when UV light is most powerful
- Minimize all time in the sun, since UV exposure occurs even in the winter and on cloudy days[45]
- Using sun protection
- Applying sunscreens with SPF ratings 30 or greater that also block both UVA and UVB light, at least every 2 hours and after swimming or sweating[45]
- Applying sunscreen at least 15 minutes before going outside, as this allows time for the sunscreen to be absorbed appropriately by the skin[45]
- Wearing sun protective clothing such as hats, sunglasses, long-sleeved shirts, long skirts, or trousers
Recent research implicating human papillomavirus (HPV) in the development of AKs suggests that HPV prevention might in turn help prevent development of AKs, as UV-induced mutations and oncogenic transformation are likely facilitated in cases of active HPV infection.[29] A key component of HPV prevention includes vaccination, and the CDC currently recommends routine vaccination in all children at age 11 or 12.[46]
There is some data that in individuals with a history of non-melanoma skin cancer, a low-fat diet can serve as a preventative measure against future actinic keratoses.[38]
Management
There are a variety of treatment options for AK depending on the patient and the clinical characteristics of the lesion. AKs show a wide range of features, which guide decision-making in choosing treatment. As there are multiple effective treatments, patient preference and lifestyle are also factors that physicians consider when determining the management plan for actinic keratosis.[47] Regular follow-up is advisable after any treatment to make sure no new lesions have developed and that old ones are not progressing. Adding topical treatment after a procedure may improve outcomes.[48]
Medication
Topical medications are often recommended for areas where multiple or ill-defined AKs are present, as the medication can easily be used to treat a relatively large area.[47]
Fluorouracil cream
Topical fluorouracil (5-FU) destroys AKs by blocking methylation of thymidylate synthetase, thereby interrupting DNA and RNA synthesis.[49] This in turn prevents the proliferation of dysplastic cells in AK. Topical 5-FU is the most utilized treatment for AK, and often results in effective removal of the lesion.[50] Overall, there is a 50% efficacy rate resulting in 100% clearance of AKs treated with topical 5-FU.[51][52] 5-FU may be up to 90% effective in treating non-hyperkeratotic lesions.[53] While topical 5-FU is a widely used and cost-effective treatment for AKs and is generally well tolerated, its potential side-effects can include: pain, crusting, redness, and local swelling.[54] These adverse effects can be mitigated or minimized by reducing the frequency of application or taking breaks between uses.[54] The most commonly used application regimen consists of applying a layer of topical cream to the lesion twice a day after washing; duration of treatment is typically 2–4 weeks to thinner skin like the cheeks and up to 8 weeks for the arms; treatment of up to 8 weeks has demonstrated a higher cure rate.[55][56]
Imiquimod cream
Imiquimod is a topical immune-enhancing agent licensed for the treatment of genital warts.[25] Imiquimod stimulates the immune system through the release and up-regulation of cytokines.[55] Treatment with Imiquimod cream applied 2–3 times per week for 12 to 16 weeks was found to result in complete resolution of AKs in 50% of people, compared to 5% of controls.[57] The Imiquimod 3.75% cream has been validated in a treatment regimen consisting of daily application to entire face and scalp for two 2-week treatment cycles, with a complete clearance rate of 36%.[58]
While the clearance rate observed with the Imiquimod 3.75% cream was lower than that observed with the 5% cream (36 and 50 percent, respectively), there are lower reported rates of adverse reactions with the 3.75% cream: 19% of individuals using Imiquimod 3.75% cream reported adverse reactions including local erythema, scabbing, and flaking at the application site, while nearly a third of individuals using the 5% cream reported the same types of reactions with Imiquimod treatment.[57][58] However, it is ultimately difficult to compare the efficacy of the different strength creams directly, as current study data varies in methodology (e.g. duration and frequency of treatment, and amount of skin surface area covered).
Ingenol mebutate gel
Ingenol mebutate is a newer treatment for AK used in Europe and the United States. It works in two ways, first by disrupting cell membranes and mitochondria resulting cell death, and then by inducing antibody-dependent cellular cytotoxicity to eliminate remaining tumor cells.[59] A 3-day treatment course with the 0.015% gel is recommended for the scalp and face, while a 2-day treatment course with the 0.05% gel is recommended for the trunk and extremities.[60] Treatment with the 0.015% gel was found to completely clear 57% of AK, while the 0.05% gel had a 34% clearance rate.[61] Advantages of ingenol mebutate treatment include the short duration of therapy and a low recurrence rate.[62] Local skin reactions including pain, itching and redness can be expected during treatment with ingenol mebutate. This treatment was derived from the petty spurge, Euphorbia peplus which has been used as a traditional remedy for keratosis.
Diclofenac sodium gel
Topical diclofenac sodium gel is a nonsteroidal anti-inflammatory drug that is thought to work in the treatment of AK through its inhibition of the arachidonic acid pathway, thereby limiting the production of prostaglandins which are thought to be involved in the development of UVB-induced skin cancers.[40] Recommended duration of therapy is 60 to 90 days with twice daily application. Treatment of facial AK with diclofenac gel led to complete lesion resolution in 40% of cases.[63] Common side effects include dryness, itching, redness, and rash at the site of application.[63]
Retinoids
Topical retinoids have been studied in the treatment of AK with modest results, and the American Academy of Dermatology does not currently recommend this as first-line therapy.[64] Treatment with adapalene gel daily for 4 weeks, and then twice daily thereafter for a total of nine months led to a significant but modest reduction in the number AKs compared to placebo; it demonstrated the additional advantage of improving the appearance of photodamaged skin.[65]
Topical tretinoin is ineffective as treatment for reducing the number of AKs.[25] For secondary prevention of AK, systemic, low-dose acitretin was found to be safe, well tolerated and moderately effective in chemoprophylaxis for skin cancers in kidney transplant patients.[66] Acitretin is a viable treatment option for organ transplant patients according to expert opinion.[47]
Tirbanibulin
Tirbanibulin (Klisyri) was approved for medical use in the United States in December 2020, for the treatment of actinic keratosis on the face or scalp.[67][68][69][70]
Cryotherapy

Liquid nitrogen (−195.8 °C) is the most commonly used destructive therapy for the treatment of AK in the United States.[71] It is a well-tolerated office procedure that does not require anesthesia.[72]
Cryotherapy is particularly indicated for cases where there are fewer than 15 thin, well-demarcated lesions.[71] Caution is encouraged for thicker, more hyperkeratotic lesions, as dysplastic cells may evade treatment.[56] Treatment with both cryotherapy and field treatment can be considered for these more advanced lesions.[56] Cryotherapy is generally performed using an open-spray technique, wherein the AK is sprayed for several seconds.[25]
The process can be repeated multiple times in one office visit, as tolerated. Cure rates from 67 to 99 percent have been reported,[73][15] depending on freeze time and lesion characteristics. Disadvantages include discomfort during and after the procedure; blistering, scarring and redness; hypo- or hyperpigmentation; and destruction of healthy tissue.[74]
Photodynamic therapy

AKs are one of the most common dermatologic lesions for which photodynamic therapy, including topical methyl aminolevulinate (MAL) or 5-aminolevulinic acid (5-ALA), is indicated.[75]
Treatment begins with preparation of the lesion, which includes scraping away scales and crusts using a dermal curette. A thick layer of topical MAL or 5-ALA cream is applied to the lesion and a small area surrounding the lesion, which is then covered with an occlusive dressing and left for a period of time. During this time the photosensitizer accumulates in the target cells within the AK lesion. The dressings are then removed and the lesion is treated with light at a specified wavelength.
Multiple treatment regimens using different photosensitizers, incubation times, light sources, and pretreatment regimens have been studied and suggest that longer incubation times lead to higher rates of lesion clearance.[76] Photodynamic therapy is gaining in popularity. It has been found to have a 14% higher likelihood of achieving complete lesion clearance at 3 months compared to cryotherapy,[77] and seems to result in superior cosmetic outcomes when compared to cryotherapy or 5-FU treatment.[78] Photodynamic therapy can be particularly effective in treating areas with multiple AK lesions.[79]
Surgical techniques
- Surgical excision: Excision should be reserved for cases when the AK is a thick, horny papule, or when deeper invasion is suspected and histopathologic diagnosis is necessary.[25] It is a rarely utilized technique for AK treatment.
- Shave excision and curettage (sometimes followed by electrodesiccation when deemed appropriate by the physician[80][71]): This technique is often used for treatment of AKs, and particularly for lesions appearing more similar to squamous cell carcinoma, or those that are unresponsive to other treatments.[71] The surface of the lesion can be scraped away using a scalpel, or the base can be removed with a curette. Tissue can be evaluated histopathologically under the microscope, but specimens acquired using this technique are not often adequate to determine whether a lesion is invasive or intraepidermal.
- Dermabrasion: Dermabrasion is useful in the treatment of large areas with multiple AK lesions. The process involves using a hand-held instrument to "sand" the skin, removing the stratum corneum layer of the epidermis. Diamond fraises or wire brushes revolving at high speeds are used.[25] The procedure can be quite painful and requires procedural sedation and anesthetic, necessitating a hospital stay. One-year clearance rates with dermabrasion treatment are as high as 96%, but diminish drastically to 54% at five years.[81]
Laser therapy
Laser therapy using carbon dioxide (CO2) or erbium:yttrium aluminum garnet (Er:YAG) lasers is a treatment approach being utilized with increased frequency, and sometimes in conjunction with computer scanning technology.[82] Laser therapy has not been extensively studied, but current evidence suggests it may be effective in cases involving multiple AKs refractive to medical therapy, or AKs located in cosmetically sensitive locations such as the face.[83] The CO2 laser has been recommended for extensive actinic cheilitis that has not responded to 5-FU.[56]
Chemical peels
A chemical peel is a topically applied agent that wounds the outermost layer of the skin, promoting organized repair, exfoliation, and eventually the development of smooth and rejuvenated skin. Multiple therapies have been studied. A medium-depth peel may effectively treat multiple non-hyperkeratotic AKs.[84] It can be achieved with 35% to 50% trichloroacetic acid (TCA) alone or at 35% in combination with Jessner's solution in a once-daily application for a minimum of 3 weeks; 70% glycolic acid (α-hydroxy acid); or solid CO2.[85] When compared to treatment with 5-FU, chemical peels have demonstrated similar efficacy and increased ease of use with similar morbidity.[86] Chemical peels must be performed in a controlled clinic environment and are recommended only for individuals who are able to comply with follow-up precautions, including avoidance of sun exposure. Furthermore, they should be avoided in individuals with a history of HSV infection or keloids, and in those who are immunosuppressed or who are taking photosensitizing medications.
Prognosis

Untreated AKs follow one of three paths: they can either persist as AKs, regress, or progress to invasive skin cancer, as AK lesions are considered to be on the same continuum with squamous cell carcinoma (SCC).[17] AK lesions that regress also have the potential to recur.
- Progression: The overall risk of an AK turning into invasive cancer is low. In average-risk individuals, likelihood of an AK lesion progressing to SCC is less than 1% per year.[87][88] Despite this low rate of progression, studies suggest that a full 60% of SCCs arise from pre-existing AKs, reinforcing the idea that these lesions are closely related.[87][88]
- Regression: Reported regression rates for single AK lesions have ranged between 15 and 63% after one year.[89]
- Recurrence: Recurrence rates after 1 year for single AK lesions that have regressed range between 15 and 53%.[89]
Clinical course
Given the aforementioned differering clinical outcomes, it is difficult to predict the clinical course of any given actinic keratosis. AK lesions may also come and go—in a cycle of appearing on the skin, remaining for months, and then disappearing. Often they will reappear in a few weeks or months, particularly after unprotected sun exposure. Left untreated, there is a chance that the lesion will advance to become invasive. Although it is difficult to predict whether an AK will advance to become squamous cell carcinoma, it has been noted that squamous cell carcinomas originate in lesions formerly diagnosed as AKs with frequencies reported between 65 and 97%.[17]
Epidemiology
Actinic keratosis is very common, with an estimated 14% of dermatology visits related to AKs.[90] It is seen more often in fair-skinned individuals,[33] and rates vary with geographical location and age.[91] Other factors such as exposure to ultraviolet (UV) radiation,[92] certain phenotypic features, and immunosuppression can also contribute to the development of AKs.
Men are more likely to develop AK than women, and the risk of developing AK lesions increases with age. These findings have been observed in multiple studies, with numbers from one study suggesting that approximately 5% of women ages 20–29 develop AK compared to 68% of women ages 60–69, and 10% of men ages 20–29 develop AK compared to 79% of men ages 60–69.[93]
Geography seems to play a role in the sense that individuals living in locations where they are exposed to more UV radiation throughout their lifetime have a significantly higher risk of developing AK. Much of the literature on AK comes from Australia, where the prevalence of AK is estimated at 40–50% in adults over 40,[93] as compared to the United States and Europe, where prevalence is estimated at under 11–38% in adults.[37][92] One study found that those who immigrated to Australia after age 20 had fewer AKs than native Australians in all age groups.[94]
Research
Diagnostically, researchers are investigating the role of novel biomarkers to assist in determining which AKs are more likely to develop into cutaneous or metastatic SCC. Upregulation of matrix metalloproteinases (MMP) is seen in many different types of cancers, and the expression and production of MMP-7 in particular has been found to be elevated in SCC specifically.[95] The role of serin peptidase inhibitors (Serpins) is also being investigated. SerpinA1 was found to be elevated in the keratinocytes of SCC cell lines, and SerpinA1 upregulation was correlated with SCC tumor progression in vivo.[95] Further investigation into specific biomarkers could help providers better assess prognosis and determine best treatment approaches for particular lesions.
In terms of treatment, a number of medications are being studied. Resiquimod is a TLR 7/8 agonist that works similarly to imiquimod, but is 10 to 100 times more potent; when used to treat AK lesions, complete response rates have range from 40 to 74%.[96] Afamelanotide is a drug that induces the production of melanin by melanocytes to act as a protective factor against UVB radiation.[97] It is being studied to determine its efficacy in preventing AKs in organ transplant patients who are on immunosuppressive therapy. Epidermal growth factor receptor (EGFR) inhibitors such as gefitinib, and anti-EGFR antibodies such as cetuximab are used in the treatment of various types of cancers, and are currently being investigated for potential use in the treatment and prevention of AKs.[98]
References
- Rapini RP, Bolognia J, Jorizzo JL (2007). Dermatology: 2-Volume Set. St. Louis: Mosby. pp. Chapter 108. ISBN 978-1-4160-2999-1.
- Logan CM, Rice MK (1987). Logan's Medical and Scientific Abbreviations. J. B. Lippincott and Company. p. 512. ISBN 0-397-54589-4.
- Prajapati V, Barankin B (May 2008). "Dermacase. Actinic keratosis". Canadian Family Physician. 54 (5): 691, 699. PMC 2377206. PMID 18474700.
- Freedberg, et al. (2003). Fitzpatrick's Dermatology in General Medicine. (6th ed.). McGraw-Hill. ISBN 0-07-138076-0.
- Quaedvlieg PJ, Tirsi E, Thissen MR, Krekels GA (2006). "Actinic keratosis: how to differentiate the good from the bad ones?". European Journal of Dermatology. 16 (4): 335–9. PMID 16935787.
- Kang, Sewon (2019). Fitzpatrick's dermatology. Fitzpatrick, Thomas B. (Thomas Bernard), 1919-2003., Kang, Sewon (Ninth ed.). New York. ISBN 978-0-07-183778-1. OCLC 1055569130.
- "actinic keratosis" at Dorland's Medical Dictionary
- Weedon D (2010). Weedon's Skin Pathology (3rd ed.). Elsevier. ISBN 978-0-7020-3485-5.
- Moy RL (January 2000). "Clinical presentation of actinic keratoses and squamous cell carcinoma". Journal of the American Academy of Dermatology. 42 (1 Pt 2): 8–10. doi:10.1067/mjd.2000.103343. PMID 10607350.
- Stockfleth E, Kerl H (Nov–Dec 2006). "Guidelines for the management of actinic keratoses". European Journal of Dermatology. 16 (6): 599–606. PMID 17229598.
- "Actinic keratosis - Symptoms, diagnosis and treatment | BMJ Best Practice". bestpractice.bmj.com. Retrieved 2019-11-25.
- Werner RN, Stockfleth E, Connolly SM, Correia O, Erdmann R, Foley P, Gupta AK, Jacobs A, Kerl H, Lim HW, Martin G, Paquet M, Pariser DM, Rosumeck S, Röwert-Huber HJ, Sahota A, Sangueza OP, Shumack S, Sporbeck B, Swanson NA, Torezan L, Nast A (November 2015). "Evidence- and consensus-based (S3) Guidelines for the Treatment of Actinic Keratosis - International League of Dermatological Societies in cooperation with the European Dermatology Forum - Short version". Journal of the European Academy of Dermatology and Venereology. 29 (11): 2069–79. doi:10.1111/jdv.13180. PMID 26370093. S2CID 19644716.
- Szeimies RM, Torezan L, Niwa A, Valente N, Unger P, Kohl E, Schreml S, Babilas P, Karrer S, Festa-Neto C (July 2012). "Clinical, histopathological and immunohistochemical assessment of human skin field cancerization before and after photodynamic therapy". The British Journal of Dermatology. 167 (1): 150–9. doi:10.1111/j.1365-2133.2012.10887.x. PMID 22329784. S2CID 10970924.
- Ibrahim SF, Brown MD (July 2009). "Actinic keratoses: a comprehensive update". The Journal of Clinical and Aesthetic Dermatology. 2 (7): 43–8. PMC 2924136. PMID 20729970.
- Thai KE, Fergin P, Freeman M, Vinciullo C, Francis D, Spelman L, Murrell D, Anderson C, Weightman W, Reid C, Watson A, Foley P (September 2004). "A prospective study of the use of cryosurgery for the treatment of actinic keratoses". International Journal of Dermatology. 43 (9): 687–92. doi:10.1111/j.1365-4632.2004.02056.x. PMID 15357755. S2CID 24067576.
- Taylor CR, Stern RS, Leyden JJ, Gilchrest BA (January 1990). "Photoaging/photodamage and photoprotection". Journal of the American Academy of Dermatology. 22 (1): 1–15. doi:10.1016/0190-9622(90)70001-x. PMID 2405022.
- Rosen T, Lebwohl MG (January 2013). "Prevalence and awareness of actinic keratosis: barriers and opportunities". Journal of the American Academy of Dermatology. 68 (1 Suppl 1): S2-9. doi:10.1016/j.jaad.2012.09.052. PMID 23228302.
- Duncan KO, Geisse JK (2008). Epithelial precancerous lesions. In: Fitzpatrick's Dermatology in General Medicine. McGraw-Hill. p. 1007.
- Butani AK, Butani A, Arbesfeld DM, Schwartz RA (April 2005). "Premalignant and early squamous cell carcinoma". Clinics in Plastic Surgery. 32 (2): 223–35. doi:10.1016/j.cps.2004.11.001. PMID 15814119.
- Yu RC, Pryce DW, Macfarlane AW, Stewart TW (May 1991). "A histopathological study of 643 cutaneous horns". The British Journal of Dermatology. 124 (5): 449–52. doi:10.1111/j.1365-2133.1991.tb00624.x. PMID 2039721. S2CID 73180732.
- Zalaudek I, Ferrara G, Leinweber B, Mercogliano A, D'Ambrosio A, Argenziano G (December 2005). "Pitfalls in the clinical and dermoscopic diagnosis of pigmented actinic keratosis". Journal of the American Academy of Dermatology. 53 (6): 1071–4. doi:10.1016/j.jaad.2005.08.052. PMID 16310072.
- Bagazgoitia L, Cuevas J, Juarranz A (February 2010). "Expression of p53 and p16 in actinic keratosis, bowenoid actinic keratosis and Bowen's disease". Journal of the European Academy of Dermatology and Venereology. 24 (2): 228–30. doi:10.1111/j.1468-3083.2009.03337.x. PMID 19515076. S2CID 23353708.
- Casari, A; Chester, J; Pellacani, G (March 2018). "Actinic Keratosis and Non-Invasive Diagnostic Techniques: An Update". Biomedicines. 6 (1): 8. doi:10.3390/biomedicines6010008. PMC 5874665. PMID 29316678.
- Quaedvlieg PJ, Tirsi E, Thissen MR, Krekels GA (Jul–Aug 2006). "Actinic keratosis: how to differentiate the good from the bad ones?". European Journal of Dermatology. 16 (4): 335–9. PMID 16935787.
- Rossi R, Mori M, Lotti T (September 2007). "Actinic keratosis". International Journal of Dermatology. 46 (9): 895–904. doi:10.1111/j.1365-4632.2007.03166.x. PMID 17822489. S2CID 221808877.
- Taguchi M, Watanabe S, Yashima K, Murakami Y, Sekiya T, Ikeda S (October 1994). "Aberrations of the tumor suppressor p53 gene and p53 protein in solar keratosis in human skin". The Journal of Investigative Dermatology. 103 (4): 500–3. doi:10.1111/1523-1747.ep12395643. PMID 7930674.
- Dodds A, Chia A, Shumack S (June 2014). "Actinic keratosis: rationale and management". Dermatology and Therapy. 4 (1): 11–31. doi:10.1007/s13555-014-0049-y. PMC 4065271. PMID 24627245.
- Nelson MA, Einspahr JG, Alberts DS, Balfour CA, Wymer JA, Welch KL, Salasche SJ, Bangert JL, Grogan TM, Bozzo PO (September 1994). "Analysis of the p53 gene in human precancerous actinic keratosis lesions and squamous cell cancers". Cancer Letters. 85 (1): 23–9. doi:10.1016/0304-3835(94)90234-8. PMID 7923098.
- Weissenborn SJ, Nindl I, Purdie K, Harwood C, Proby C, Breuer J, Majewski S, Pfister H, Wieland U (July 2005). "Human papillomavirus-DNA loads in actinic keratoses exceed those in non-melanoma skin cancers". The Journal of Investigative Dermatology. 125 (1): 93–7. doi:10.1111/j.0022-202X.2005.23733.x. PMID 15982308.
- Röwert-Huber J, Patel MJ, Forschner T, Ulrich C, Eberle J, Kerl H, Sterry W, Stockfleth E (May 2007). "Actinic keratosis is an early in situ squamous cell carcinoma: a proposal for reclassification". The British Journal of Dermatology. 156 Suppl 3: 8–12. doi:10.1111/j.1365-2133.2007.07860.x. PMID 17488400. S2CID 1748119.
- Engel A, Johnson ML, Haynes SG (January 1988). "Health effects of sunlight exposure in the United States. Results from the first National Health and Nutrition Examination Survey, 1971-1974". Archives of Dermatology. 124 (1): 72–9. doi:10.1001/archderm.1988.01670010036018. PMID 3257372.
- Thompson SC, Jolley D, Marks R (October 1993). "Reduction of solar keratoses by regular sunscreen use". The New England Journal of Medicine. 329 (16): 1147–51. doi:10.1056/nejm199310143291602. PMID 8377777.
- Frost CA, Green AC, Williams GM (December 1998). "The prevalence and determinants of solar keratoses at a subtropical latitude (Queensland, Australia)". The British Journal of Dermatology. 139 (6): 1033–9. doi:10.1046/j.1365-2133.1998.02560.x. PMID 9990367. S2CID 21909024.
- Clinical practice guide: basal cell carcinoma, squamous cell carcinoma (and related lesions): a guide to clinical management in Australia. Cancer Council Australia., Australian Cancer Network. Sydney, N.S.W.: Cancer Council Australia. 2008. ISBN 978-0-9775060-6-4. OCLC 311871073.
{{cite book}}: CS1 maint: others (link) - "Actinic Keratosis (AK)". The Lecturio Medical Concept Library. 12 November 2020. Retrieved 26 June 2021.
- McBride P, Neale R, Pandeya N, Green A (July 2007). "Sun-related factors, betapapillomavirus, and actinic keratoses: a prospective study". Archives of Dermatology. 143 (7): 862–8. doi:10.1001/archderm.143.7.862. PMID 17638729.
- Flohil SC, van der Leest RJ, Dowlatshahi EA, Hofman A, de Vries E, Nijsten T (August 2013). "Prevalence of actinic keratosis and its risk factors in the general population: the Rotterdam Study". The Journal of Investigative Dermatology. 133 (8): 1971–8. doi:10.1038/jid.2013.134. PMID 23510990.
- James WD, Elston DM, Berger TG (2016). Andrews' Diseases of the Skin (12th ed.). Philadelphia, PA: Elsevier. ISBN 978-0-323-31967-6.
- Schaffer (2012). Jean L. Bolognia; Joseph L. Jorizzo; Julie V. (eds.). Dermatology (3rd ed.). [Philadelphia]: Elsevier Saunders. ISBN 9780723435716.
- Weedon D (2010). Weedon's Skin Pathology (3rd ed.). Elsevier. ISBN 978-0-7020-3485-5.
- Cuellar F, Vilalta A, Puig S, Palou J, Salerni G, Malvehy J (June 2009) [2009]. "New dermoscopic pattern in actinic keratosis and related conditions". Archives of Dermatology. 145 (6): 732. doi:10.1001/archdermatol.2009.86. PMID 19528439.
- Peris K, Micantonio T, Piccolo D, Fargnoli MC (November 2007). "Dermoscopic features of actinic keratosis". Journal der Deutschen Dermatologischen Gesellschaft. 5 (11): 970–6. doi:10.1111/j.1610-0387.2007.06318.x. PMID 17908179. S2CID 40465474.
- Akay BN, Kocyigit P, Heper AO, Erdem C (December 2010). "Dermatoscopy of flat pigmented facial lesions: diagnostic challenge between pigmented actinic keratosis and lentigo maligna". The British Journal of Dermatology. 163 (6): 1212–7. doi:10.1111/j.1365-2133.2010.10025.x. PMID 21083845. S2CID 205260667.
- Leffell DJ (January 2000). "The scientific basis of skin cancer". Journal of the American Academy of Dermatology. 42 (1 Pt 2): 18–22. doi:10.1067/mjd.2000.103340. PMID 10607352.
- "How to apply sunscreen". American Academy of Dermatology. Retrieved 13 December 2018.
- "HPV Vaccine Recommendations". CDC. Retrieved 13 December 2018.
- Fleming P, Zhou S, Bobotsis R, Lynde C (2017). "Comparison of the Treatment Guidelines for Actinic Keratosis: A Critical Appraisal and Review". Journal of Cutaneous Medicine and Surgery. 21 (5): 408–417. doi:10.1177/1203475417708166. PMID 28510496. S2CID 22467851.
- Heppt MV, Steeb T, Ruzicka T, Berking C (April 2019). "Cryosurgery combined with topical interventions for actinic keratosis: a systematic review and meta-analysis". The British Journal of Dermatology. 180 (4): 740–748. doi:10.1111/bjd.17435. PMID 30447074.
- Robins P, Gupta AK (August 2002). "The use of topical fluorouracil to treat actinic keratosis". Cutis. 70 (2 Suppl): 4–7. PMID 12353679.
- Gupta AK, Paquet M (August 2013). "Network meta-analysis of the outcome 'participant complete clearance' in nonimmunosuppressed participants of eight interventions for actinic keratosis: a follow-up on a Cochrane review". The British Journal of Dermatology. 169 (2): 250–9. doi:10.1111/bjd.12343. PMID 23550994. S2CID 207070300.
- Askew DA, Mickan SM, Soyer HP, Wilkinson D (May 2009). "Effectiveness of 5-fluorouracil treatment for actinic keratosis--a systematic review of randomized controlled trials". International Journal of Dermatology. 48 (5): 453–63. doi:10.1111/j.1365-4632.2009.04045.x. PMID 19416373. S2CID 13367783.
- Gupta AK, Davey V, Mcphail H (October 2005). "Evaluation of the effectiveness of imiquimod and 5-fluorouracil for the treatment of actinic keratosis: Critical review and meta-analysis of efficacy studies". Journal of Cutaneous Medicine and Surgery. 9 (5): 209–14. doi:10.1007/s10227-005-0148-6. PMID 16502198. S2CID 226134.
- "New treatments for actinic keratoses". The Medical Letter on Drugs and Therapeutics. 44 (1133): 57–8. June 2002. PMID 12080275.
- Berker, D.; McGregor, J.M.; Mohd Mustapa, M.F.; Exton, L.S.; Hughes, B.R.; McHenry, P.M.; Gibbon, K.; Buckley, D.A.; Nasr, I.; Duarte Williamson, C.E.; Swale, V.J. (January 2017). "British Association of Dermatologists' guidelines for the care of patients with actinic keratosis 2017". British Journal of Dermatology. 176 (1): 20–43. doi:10.1111/bjd.15107. ISSN 0007-0963. PMID 28098380.
- Correale CE (2002). "Actinic keratoses: new treatment options". Advances in Dermatology. 18: 339–55. PMID 12528411.
- Habif T (2016). Clinical Dermatology (Sixth ed.). Elsevier.
- Hadley G, Derry S, Moore RA (June 2006). "Imiquimod for actinic keratosis: systematic review and meta-analysis". The Journal of Investigative Dermatology. 126 (6): 1251–5. doi:10.1038/sj.jid.5700264. PMID 16557235.
- Swanson N, Abramovits W, Berman B, Kulp J, Rigel DS, Levy S (April 2010). "Imiquimod 2.5% and 3.75% for the treatment of actinic keratoses: results of two placebo-controlled studies of daily application to the face and balding scalp for two 2-week cycles". Journal of the American Academy of Dermatology. 62 (4): 582–90. doi:10.1016/j.jaad.2009.07.004. PMID 20133013.
- Rosen RH, Gupta AK, Tyring SK (March 2012). "Dual mechanism of action of ingenol mebutate gel for topical treatment of actinic keratoses: rapid lesion necrosis followed by lesion-specific immune response". Journal of the American Academy of Dermatology. 66 (3): 486–93. doi:10.1016/j.jaad.2010.12.038. PMID 22055282.
- "Picato Gel label" (PDF). Accessdate.fda.gov. Retrieved 30 March 2022.
- Lebwohl M, Swanson N, Anderson LL, Melgaard A, Xu Z, Berman B (March 2012). "Ingenol mebutate gel for actinic keratosis". The New England Journal of Medicine. 366 (11): 1010–9. doi:10.1056/nejmoa1111170. PMID 22417254. S2CID 481891.
- Lebwohl M, Shumack S, Stein Gold L, Melgaard A, Larsson T, Tyring SK (June 2013). "Long-term follow-up study of ingenol mebutate gel for the treatment of actinic keratoses". JAMA Dermatology. 149 (6): 666–70. doi:10.1001/jamadermatol.2013.2766. PMID 23553119.
- Pirard D, Vereecken P, Mélot C, Heenen M (November 2005). "Three percent diclofenac in 2.5% hyaluronan gel in the treatment of actinic keratoses: a meta-analysis of the recent studies". Archives of Dermatological Research. 297 (5): 185–9. doi:10.1007/s00403-005-0601-9. PMID 16235081. S2CID 20675689.
- Kim JY, Kozlow JH, Mittal B, Moyer J, Olenecki T, Rodgers P (March 2018). "Guidelines of care for the management of cutaneous squamous cell carcinoma". Journal of the American Academy of Dermatology. 78 (3): 560–578. doi:10.1016/j.jaad.2017.10.007. PMC 6652228. PMID 29331386.
- Kang S, Goldfarb MT, Weiss JS, Metz RD, Hamilton TA, Voorhees JJ, Griffiths CE (July 2003). "Assessment of adapalene gel for the treatment of actinic keratoses and lentigines: a randomized trial". Journal of the American Academy of Dermatology. 49 (1): 83–90. doi:10.1067/mjd.2003.451. PMID 12833014.
- Carneiro RV, Sotto MN, Azevedo LS, Ianhez LE, Rivitti EA (February 2005). "Acitretin and skin cancer in kidney transplanted patients. Clinical and histological evaluation and immunohistochemical analysis of lymphocytes, natural killer cells and Langerhans' cells in sun exposed and sun protected skin". Clinical Transplantation. 19 (1): 115–21. doi:10.1111/j.1399-0012.2004.00311.x. PMID 15659144. S2CID 27938071.
- "Klisyri: FDA-Approved Drugs". U.S. Food and Drug Administration (FDA). Retrieved 15 December 2020.
- "NDA APPROVAL" (PDF). U.S. Food and Drug Administration (FDA). Retrieved 30 March 2022.
- "FULL PRESCRIBING INFORMATION" (PDF). U.S. Food and Drug Administration (FDA). Retrieved 30 March 2022.
- "Athenex Announces FDA Approval of Klisyri (Tirbanibulin) for the Treatment of Actinic Keratosis on the Face or Scalp" (Press release). Athenex Inc. 15 December 2020. Retrieved 15 December 2020 – via GlobeNewswire.
- Dinehart SM (January 2000). "The treatment of actinic keratoses". Journal of the American Academy of Dermatology. 42 (1 Pt 2): 25–8. doi:10.1067/mjd.2000.103338. PMID 10607354.
- Zimmerman EE, Crawford P (December 2012). "Cutaneous cryosurgery". American Family Physician. 86 (12): 1118–24. PMID 23316984.
- Lubritz RR, Smolewski SA (November 1982). "Cryosurgery cure rate of actinic keratoses". Journal of the American Academy of Dermatology. 7 (5): 631–2. doi:10.1016/s0190-9622(82)70143-4. PMID 7142470.
- Kuflik EG (December 1994). "Cryosurgery updated". Journal of the American Academy of Dermatology. 31 (6): 925–44, quiz 944–6. doi:10.1016/s0190-9622(94)70261-6. PMID 7962774.
- Ericson MB, Wennberg AM, Larkö O (February 2008). "Review of photodynamic therapy in actinic keratosis and basal cell carcinoma". Therapeutics and Clinical Risk Management. 4 (1): 1–9. doi:10.2147/TCRM.S1769. PMC 2503644. PMID 18728698.
- Hauschild A, Popp G, Stockfleth E, Meyer KG, Imberger D, Mohr P, Itschert G, Kaufmann R, Neuber K, Frambach Y, Gollnick H, Brunnert M, Stocker M, Ortland C, Karrer S (February 2009). "Effective photodynamic therapy of actinic keratoses on the head and face with a novel, self-adhesive 5-aminolaevulinic acid patch". Experimental Dermatology. 18 (2): 116–21. doi:10.1111/j.1600-0625.2008.00770.x. PMID 18643849. S2CID 23405229.
- Patel G, Armstrong AW, Eisen DB (December 2014). "Efficacy of photodynamic therapy vs other interventions in randomized clinical trials for the treatment of actinic keratoses: a systematic review and meta-analysis". JAMA Dermatology. 150 (12): 1281–8. doi:10.1001/jamadermatol.2014.1253. PMID 25162181.
- Gupta AK, Paquet M, Villanueva E, Brintnell W (December 2012). "Interventions for actinic keratoses". The Cochrane Database of Systematic Reviews. 12: CD004415. doi:10.1002/14651858.CD004415.pub2. PMC 6599879. PMID 23235610.
- Kaufmann R, Spelman L, Weightman W, Reifenberger J, Szeimies RM, Verhaeghe E, Kerrouche N, Sorba V, Villemagne H, Rhodes LE (May 2008). "Multicentre intraindividual randomized trial of topical methyl aminolaevulinate-photodynamic therapy vs. cryotherapy for multiple actinic keratoses on the extremities". The British Journal of Dermatology. 158 (5): 994–9. doi:10.1111/j.1365-2133.2008.08488.x. PMID 18341663. S2CID 28246511.
- Feldman SR, Fleischer AB, Williford PM, Jorizzo JL (January 1999). "Destructive procedures are the standard of care for treatment of actinic keratoses". Journal of the American Academy of Dermatology. 40 (1): 43–7. doi:10.1016/s0190-9622(99)70526-8. PMID 9922011.
- Coleman WP, Yarborough JM, Mandy SH (January 1996). "Dermabrasion for prophylaxis and treatment of actinic keratoses". Dermatologic Surgery. 22 (1): 17–21. doi:10.1111/j.1524-4725.1996.tb00565.x. PMID 8556252. S2CID 9346937.
- Iyer S, Friedli A, Bowes L, Kricorian G, Fitzpatrick RE (February 2004). "Full face laser resurfacing: therapy and prophylaxis for actinic keratoses and non-melanoma skin cancer". Lasers in Surgery and Medicine. 34 (2): 114–9. doi:10.1002/lsm.20012. PMID 15004822. S2CID 11048857.
- Massey RA, Eliezri YD (June 1999). "A case report of laser resurfacing as a skin cancer prophylaxis". Dermatologic Surgery. 25 (6): 513–6. doi:10.1046/j.1524-4725.1999.08260.x. PMID 10469105.
- Monheit GD (July 2001). "Medium-depth chemical peels". Dermatologic Clinics. 19 (3): 413–25, vii. doi:10.1016/s0733-8635(05)70282-5. PMID 11599398.
- Drake LA, Ceilley RI, Cornelison RL, Dobes WL, Dorner W, Goltz RW, Graham GF, Lewis CW, Salasche SJ, Turner ML (January 1995). "Guidelines of care for actinic keratoses. Committee on Guidelines of Care". Journal of the American Academy of Dermatology. 32 (1): 95–8. doi:10.1016/0190-9622(95)90191-4. PMID 7529779.
- Lawrence N, Cox SE, Cockerell CJ, Freeman RG, Cruz PD (February 1995). "A comparison of the efficacy and safety of Jessner's solution and 35% trichloroacetic acid vs 5% fluorouracil in the treatment of widespread facial actinic keratoses". Archives of Dermatology. 131 (2): 176–81. doi:10.1001/archderm.131.2.176. PMID 7857114.
- Marks R, Rennie G, Selwood TS (April 1988). "Malignant transformation of solar keratoses to squamous cell carcinoma". Lancet. 1 (8589): 795–7. doi:10.1016/s0140-6736(88)91658-3. PMID 2895318. S2CID 10685710.
- Criscione VD, Weinstock MA, Naylor MF, Luque C, Eide MJ, Bingham SF (June 2009). "Actinic keratoses: Natural history and risk of malignant transformation in the Veterans Affairs Topical Tretinoin Chemoprevention Trial". Cancer. 115 (11): 2523–30. doi:10.1002/cncr.24284. PMID 19382202. S2CID 205654597.
- Werner RN, Sammain A, Erdmann R, Hartmann V, Stockfleth E, Nast A (September 2013). "The natural history of actinic keratosis: a systematic review". The British Journal of Dermatology. 169 (3): 502–18. doi:10.1111/bjd.12420. PMID 23647091. S2CID 24851936.
- Gupta AK, Cooper EA, Feldman SR, Fleischer AB (August 2002). "A survey of office visits for actinic keratosis as reported by NAMCS, 1990-1999. National Ambulatory Medical Care Survey". Cutis. 70 (2 Suppl): 8–13. PMID 12353680.
- Hensen P, Müller ML, Haschemi R, Ständer H, Luger TA, Sunderkötter C, Schiller M (2009). "Predisposing factors of actinic keratosis in a North-West German population". European Journal of Dermatology. 19 (4): 345–54. doi:10.1684/ejd.2009.0706. PMID 19470418.
- Salasche SJ (January 2000). "Epidemiology of actinic keratoses and squamous cell carcinoma". Journal of the American Academy of Dermatology. 42 (1 Pt 2): 4–7. doi:10.1067/mjd.2000.103342. PMID 10607349.
- Green A, Beardmore G, Hart V, Leslie D, Marks R, Staines D (December 1988). "Skin cancer in a Queensland population". Journal of the American Academy of Dermatology. 19 (6): 1045–52. doi:10.1016/s0190-9622(88)70270-4. PMID 3204179.
- Marks R, Jolley D, Lectsas S, Foley P (January 1990). "The role of childhood exposure to sunlight in the development of solar keratoses and non-melanocytic skin cancer". The Medical Journal of Australia. 152 (2): 62–6. doi:10.5694/j.1326-5377.1990.tb124456.x. PMID 2296232. S2CID 24283465.
- Kivisaari A, Kähäri VM (November 2013). "Squamous cell carcinoma of the skin: Emerging need for novel biomarkers". World Journal of Clinical Oncology. 4 (4): 85–90. doi:10.5306/wjco.v4.i4.85. PMC 4053710. PMID 24926428.
- Szeimies RM, Bichel J, Ortonne JP, Stockfleth E, Lee J, Meng TC (July 2008). "A phase II dose-ranging study of topical resiquimod to treat actinic keratosis". The British Journal of Dermatology. 159 (1): 205–10. doi:10.1111/j.1365-2133.2008.08615.x. PMID 18476957. S2CID 205257237.
- Barnetson RS, Ooi TK, Zhuang L, Halliday GM, Reid CM, Walker PC, Humphrey SM, Kleinig MJ (August 2006). "[Nle4-D-Phe7]-alpha-melanocyte-stimulating hormone significantly increased pigmentation and decreased UV damage in fair-skinned Caucasian volunteers". The Journal of Investigative Dermatology. 126 (8): 1869–78. doi:10.1038/sj.jid.5700317. PMID 16763547.
- Amini S, Viera MH, Valins W, Berman B (June 2010). "Nonsurgical innovations in the treatment of nonmelanoma skin cancer". The Journal of Clinical and Aesthetic Dermatology. 3 (6): 20–34. PMC 2921754. PMID 20725548.