Haemophilus influenzae
Haemophilus influenzae (formerly called Pfeiffer's bacillus or Bacillus influenzae) is a Gram-negative, non-motile, coccobacillary, facultatively anaerobic, capnophilic pathogenic bacterium of the family Pasteurellaceae. The bacteria are mesophilic and grow best at temperatures between 35-37℃.[1]
| Haemophilus influenzae | |
|---|---|
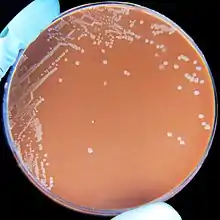 | |
| H. influenzae on a chocolate agar plate | |
| Scientific classification | |
| Domain: | Bacteria |
| Phylum: | Pseudomonadota |
| Class: | Gammaproteobacteria |
| Order: | Pasteurellales |
| Family: | Pasteurellaceae |
| Genus: | Haemophilus |
| Species: | H. influenzae |
| Binomial name | |
| Haemophilus influenzae (Lehmann & Neumann 1896) Winslow et al. 1917 | |
H. influenzae was first described in 1892 by Richard Pfeiffer during an influenza pandemic[2] when he incorrectly described Haemophilus influenzae as the causative microbe, which is why the bacteria retain the name "influenza".[3][4] H. influenzae is responsible for a wide range of localized and invasive infections, typically in infants and children,[5] including pneumonia, meningitis, or bloodstream infections.[6] Treatment consists of antibiotics, however H. influenzae is often resistant to the penicillin family but Augmentin can be used in mild cases.[7] The recommended form of prevention is a series of the Hib vaccine and boosters, which are most often given under the age of 5, and sometimes in conjunction with other vaccines in the form of the DTaP-IPV/Hib vaccine.[8]
This species was the first free-living microorganism to have its entire genome sequenced.[9]
Serotypes
In 1930, two major categories of H. influenzae were defined: the unencapsulated strains and the encapsulated strains. Encapsulated strains were classified on the basis of their distinct capsular antigens. The six generally recognized types of encapsulated H. influenzae are: a, b, c, d, e, and f.[10] H. Influenzae type b, also known as Hib, is the most common form, recognizable by it's polyribosyl ribitol phosphate (PRP) capsule, and found mostly in children.[11] Types a, e, and f have been isolated infrequently, while types d and c are rarely isolated. Unencapsulated strains have a greater number of isolates and genetic diversity than the encapsulated group. Unencapsulated strains are termed nontypable (NTHi) because they lack capsular serotypes; however, they can be classified by multilocus sequence typing. NTHi strains are considered to be part of the normal human flora in the upper and lower respiratory tract, genitals, and conjunctivae (mucous membranes of the eye).[11]
Diagnosis

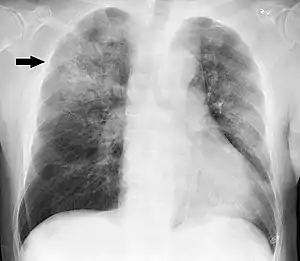

Clinical features may include initial symptoms of an upper respiratory tract infection mimicking a viral infection, usually associated with low-grade fevers. This may progress to the lower respiratory tract within a few days, with features often resembling those of wheezy bronchitis. Sputum may be difficult to expectorate and is often grey or creamy in color. The cough may persist for weeks without appropriate treatment. Many cases are diagnosed after presenting chest infections that do not respond to penicillins or first-generation cephalosporins. A chest X-ray can identify alveolar consolidation.[12]
Clinical diagnosis of H. influenzae is typically performed by bacterial culture or latex particle agglutinations. Diagnosis is considered confirmed when the organism is isolated from a sterile body site. In this respect, H. influenzae cultured from the nasopharyngeal cavity or sputum would not indicate H. influenzae disease, because these sites are colonized in disease-free individuals.[13] However, H. influenzae isolated from cerebrospinal fluid or blood would indicate H. influenzae infection.
Culture

Bacterial culture of H. influenzae is performed on agar plates, the preferable one being chocolate agar, with added X (hemin) and V (nicotinamide adenine dinucleotide) factors at 37 °C in a CO2-enriched incubator.[14] The ideal CO2 concentration for the culture is ~5%.[15] Blood agar growth is only achieved as a satellite phenomenon around other bacteria. Colonies of H. influenzae appear as convex, smooth, pale, grey, or transparent colonies.[15]
Gram stained and microscopic observation of a specimen of H. influenzae will show Gram-negative coccobacillus. The cultured organism can be further characterized using catalase and oxidase tests, both of which should be positive. Further serological testing is necessary to distinguish the capsular polysaccharide and differentiate between H. influenzae b and nonencapsulated species.
Although highly specific, bacterial culture of H. influenzae lacks sensitivity. Use of antibiotics prior to sample collection greatly reduces the isolation rate by killing the bacteria before identification is possible.[16] Recent work has shown that H.influenzae uses a highly specialized spectrum of nutrients where lactate is a preferred carbon source.[17]
H. influenzae will grow in the hemolytic zone of Staphylococcus aureus on blood agar plates; the hemolysis of cells by S. aureus releases factor V which is needed for its growth. H. influenzae will not grow outside the hemolytic zone of S. aureus due to the lack of nutrients such as factor V in these areas.[18]
Latex particle agglutination
The latex particle agglutination test (LAT) is a more sensitive method to detect H. influenzae than is culture.[19] Because the method relies on antigen rather than viable bacteria, the results are not disrupted by prior antibiotic use. It also has the added benefit of being much quicker than culture methods. However, antibiotic sensitivity testing is not possible with LAT alone, so a parallel culture is necessary.[20]
Molecular methods
Polymerase chain reaction (PCR) assays have been proven to be more sensitive than either LAT or culture tests, and are highly specific.[21] These PCR tests can be used for capsular typing of encapsulated H. influenzae strains.[22]
Pathogenicity
Most strains of H. influenzae are opportunistic pathogens; that is, they usually live in their host without causing disease, but cause problems only when other factors (such as a viral infection, reduced immune function or chronically inflamed tissues, e.g. from allergies) create an opportunity. They infect the host by sticking to the host cell using trimeric autotransporter adhesins.[23]
The pathogenesis of H. influenzae infections is not completely understood, although the presence of the polyribosyl ribitol phosphate (PRP) capsule in encapsulated type b (Hib), a serotype causing conditions such as epiglottitis, is known to be a major factor in virulence.[24] Their capsule allows them to resist phagocytosis and complement-mediated lysis in the nonimmune host. The unencapsulated strains are almost always less invasive; however, they can produce an inflammatory response in humans, which can lead to many symptoms. Vaccination with Hib conjugate vaccine is effective in preventing Hib infection but does not prevent infection with NTHi strains.[25]
Haemophilus influenzae can cause respiratory tract infections including pneumonia, otitis media, epiglottitis (swelling in the throat), eye infections and bloodstream infection, meningitis. It can also cause cellulitis (skin infection) and infectious arthritis (inflammation of the joint).[26]
Haemophilus influenzae type b (Hib) infection
Naturally acquired disease caused by H. influenzae seems to occur in humans only. In healthy children under the age of 5, H. influenzae type b was responsible for more than 80% of aggressive infections, before the introduction of the [Hib] vaccine.[27] In infants and young children, H. influenzae type b (Hib) causes bacteremia, pneumonia, epiglottitis and acute bacterial meningitis.[28] On occasion, it causes cellulitis, osteomyelitis, and infectious arthritis. It is one cause of neonatal infection.[29]
Due to routine use of the Hib vaccine in the U.S. since 1990, the incidence of invasive Hib disease has decreased to 1.3/100,000 in children.[28] However, Hib remains a major cause of lower respiratory tract infections in infants and children in developing countries where the vaccine is not widely used. Unencapsulated H. influenzae strains are unaffected by the Hib vaccine and cause ear infections (otitis media), eye infections (conjunctivitis), and sinusitis in children, and are associated with pneumonia.[28]
Haemophilus influenzae colonization
Many microbes colonize within a host organism. Colonization occurs when a microorganism continues to multiply within the host, without interaction, causing no visible signs of illness or infection. Haemophilus influenzae colonizes differently in adults than it does young children. Because this bacterium colonizes more rapidly in young children, they are capable of carrying more than one strain of the same bacterium. Once in the adult stage of life, a human is likely to only be carrying one strain as this bacterium does not colonize as aggressively in adults. Nearly all infants will undergo colonization of this bacteria within their first year of life.[30]
Treatment
Some strains of Haemophilus influenzae produce beta-lactamases, and are also able to modify its penicillin-binding proteins, so the bacteria have gained resistance to the penicillin family of antibiotics. In severe cases, cefotaxime and ceftriaxone delivered directly into the bloodstream are the elected antibiotics, and, for the less severe cases, an association of ampicillin and sulbactam, cephalosporins of the second and third generation, or fluoroquinolones are preferred. (Fluoroquinolone-resistant Haemophilus influenzae have been observed.)[31]
Macrolides and fluoroquinolones have activity against non-typeable H. influenzae and could be used in patients with a history of allergy to beta-lactam antibiotics.[32] However, macrolide resistance has also been observed.[33]
Serious and chronic complications
The serious complications of HiB are brain damage, hearing loss, and even death. This is commonly associated with HiB but however the Hi non-typable doesn't often cause serious conditions but it has more risks to a chronic infection because it has the ability to change its surface antigens. Chronic infections are usually not as serious than acute infections.[34]
Prevention

Effective vaccines for Haemophilus influenzae Type B have been available since the early 1990s, and are recommended for children under age 5 and asplenic patients. The World Health Organization recommends a pentavalent vaccine, combining vaccines against diphtheria, tetanus, pertussis, hepatitis B and Hib. There is not yet sufficient evidence on how effective this pentavalent vaccine is in relation to the individual vaccines.[35]
Hib vaccines cost about seven times the total cost of vaccines against measles, polio, tuberculosis, diphtheria, tetanus, and pertussis. Consequently, whereas 92% of the populations of developed countries were vaccinated against Hib as of 2003, vaccination coverage was 42% for developing countries, and only 8% for least-developed countries.[36]
The Hib vaccines do not provide cross-protection to any other Haemophilus influenzae serotypes like Hia, Hic, Hid, Hie or Hif.[37]
An oral vaccination has been developed for non-typeable Haemophilus influenzae (NTHi) for patients with chronic bronchitis but it has not shown to be effective in reducing the number and severity of COPD exacerbations.[38] However, there is no effective vaccine for the other types of capsulated Haemophilus inflenzae or Haemophilus inflenzae nontypeable.
Genome
H. influenzae was the first free-living organism to have its entire genome sequenced. Completed by Craig Venter and his team at The Institute for Genomic Research, now part of the J. Craig Venter Institute. Haemophilus was chosen because one of the project leaders, Nobel laureate Hamilton Smith, had been working on it for decades and was able to provide high-quality DNA libraries. The sequencing method used was whole-genome shotgun, which was completed and published in Science in 1995.[39]
The genome of strain Rd KW20 consists of 1,830,138 base pairs of DNA in a single circular chromosome that contains 1604 protein-coding genes, 117 pseudogenes, 57 tRNA genes, and 23 other RNA genes.[40] About 90% of the genes have homologs in E. coli, another gamma-proteobacterium. In fact, the similarity between genes of the two species ranges from 18% to 98% protein sequence identity, with the majority sharing 40-80% of their amino acids (with an average of 59%).[41]
Conjugative plasmids (DNA molecules that are capable of horizontal transfer between different species of bacteria) can frequently be found in H. influenzae. It is common that the F+ plasmid of a competent Escherichia coli bacterium conjugates into the H. influenzae bacterium, which then allows the plasmid to transfer among H. influenzae strands via conjugation.[42]
Likely protective role of transformation
Unencapsulated H. influenzae is often observed in the airways of patients with chronic obstructive pulmonary disease (COPD). Neutrophils are also observed in large numbers in sputum from patients with COPD. The neutrophils phagocytize H. influenzae, thereby activating an oxidative respiratory burst.[43] However instead of killing the bacteria the neutrophils are themselves killed (though such an oxidative burst likely causes DNA damage in the H. influenzae cells). Dearth of killing the bacteria appears to explain the persistence of infection in COPD.[43]
H. influenzae mutants defective in the rec1 gene (a homolog of recA) are very sensitive to killing by the oxidizing agent hydrogen peroxide.[44] This finding suggests that rec1 expression is important for H. influenzae survival under conditions of oxidative stress. Since it is a homolog of recA, rec1 likely plays a key role in recombinational repair of DNA damage. Thus H. influenzae may protect its genome against the reactive oxygen species produced by the host's phagocytic cells through recombinational repair of oxidative DNA damages.[45] Recombinational repair of a damaged site of a chromosome requires, in addition to rec1, a second homologous undamaged DNA molecule. Individual H. influenzae cells are capable of taking up homologous DNA from other cells by the process of transformation. Transformation in H. influenzae involves at least 15 gene products,[39] and is likely an adaptation for repairing DNA damage in the resident chromosome.
Vaccines that target unencapsulated H. influenzae serotypes are in development.[46]
See also
- Hattie Alexander
- Haemophilus influenzae cellulitis
- Haemophilus meningitis
- Maurice Hilleman
- Trimeric Autotransporter Adhesins (TAA)
References
- "Meningitis, Hib and Pneumococcal Conjugate Vaccines". AAP Grand Rounds. 3 (1): 3–4. 2000-01-01. doi:10.1542/gr.3-1-3-a. ISSN 1099-6605.
- Kuhnert P, Christensen H, eds. (2008). Pasteurellaceae: Biology, Genomics and Molecular Aspects. Caister Academic Press. ISBN 978-1-904455-34-9.
- Morens DM, Taubenberger JK, Folkers GK, Fauci AS (December 2010). "Pandemic influenza's 500th anniversary". Clinical Infectious Diseases. 51 (12): 1442–1444. doi:10.1086/657429. PMC 3106245. PMID 21067353.
- Taubenberger JK, Hultin JV, Morens DM (2007). "Discovery and characterization of the 1918 pandemic influenza virus in historical context". Antiviral Therapy. 12 (4 Pt B): 581–591. doi:10.1177/135965350701200S02.1. PMC 2391305. PMID 17944266.
- "Pinkbook: Haemophilus influenzae (Hib) | CDC". www.cdc.gov. 2022-09-22. Retrieved 2022-10-13.
- "Symptoms of Haemophilus influenzae | CDC". www.cdc.gov. 2022-04-04. Retrieved 2022-10-20.
- Chang AB, Upham JW, Masters IB, Redding GR, Gibson PG, Marchant JM, Grimwood K (March 2016). "Protracted bacterial bronchitis: The last decade and the road ahead". Pediatric Pulmonology. 51 (3): 225–242. doi:10.1002/ppul.23351. PMC 7167774. PMID 26636654.
- Bar-On ES, Goldberg E, Hellmann S, Leibovici L, et al. (Cochrane Acute Respiratory Infections Group) (April 2012). "Combined DTP-HBV-HIB vaccine versus separately administered DTP-HBV and HIB vaccines for primary prevention of diphtheria, tetanus, pertussis, hepatitis B and Haemophilus influenzae B (HIB)". The Cochrane Database of Systematic Reviews (4): CD005530. doi:10.1002/14651858.CD005530.pub3. PMID 22513932.
- About the J. Craig Venter Institute, J. Craig Venter Institute website, retrieved November 21, 2015
- Ryan KJ, Ray CG, eds. (2004). Sherris Medical Microbiology (4th ed.). McGraw Hill. pp. 396–401. ISBN 978-0-8385-8529-0.
- Khattak ZE, Anjum F (2022). "Haemophilus Influenzae". StatPearls. Treasure Island (FL): StatPearls Publishing. PMID 32965847. Retrieved 2022-10-27.
- "Measuring impact of Streptococcus pneumoniae and Haemophilus influenzae type b conjugate vaccination" (PDF). World Health Organization. September 2012
- Puri J, Talwar V, Juneja M, Agarwal KN, Gupta HC (October 1999). "Prevalence of anti-microbial resistance among respiratory isolates of Haemophilus influenzae". Indian Pediatrics. 36 (10): 1029–1032. PMID 10745313.
- Levine OS; Schuchat A; Schwartz B; Wenger JD; Elliott J; Centers for Disease Control (1997). "Generic protocol for population-based surveillance of Haemophilus influenzae type B" (PDF). World Health Organization. WHO/VRD/GEN/95.05. Archived from the original (PDF) on July 1, 2004.
- "Meningitis Lab Manual: ID and Characterization of Hib | CDC". www.cdc.gov. 2022-01-05. Retrieved 2022-09-21.
- John TJ, Cherian T, Steinhoff MC, Simoes EA, John M (1991). "Etiology of acute respiratory infections in children in tropical southern India". Reviews of Infectious Diseases. 13 (Suppl 6): S463–S469. doi:10.1093/clinids/13.supplement_6.s463. PMID 1862277.
- Hosmer J, Nasreen M, Dhouib R, Essilfie AT, Schirra HJ, Henningham A, et al. (January 2022). "Access to highly specialized growth substrates and production of epithelial immunomodulatory metabolites determine survival of Haemophilus influenzae in human airway epithelial cells". PLOS Pathogens. 18 (1): e1010209. doi:10.1371/journal.ppat.1010209. PMC 8794153. PMID 35085362.
- Xi Y, Wang H, Wang S, Wu X, Wang Z (February 2022). "A study of various factors affecting satellitism tests of Haemophilus influenzae and Haemophilus parainfluenzae using Staphylococcus aureus as the source of NAD". Journal of Microbiological Methods. 193: 106417. doi:10.1016/j.mimet.2022.106417. PMID 35033634. S2CID 245957339.
- Kennedy WA, Chang SJ, Purdy K, Le T, Kilgore PE, Kim JS, et al. (October 2007). "Incidence of bacterial meningitis in Asia using enhanced CSF testing: polymerase chain reaction, latex agglutination and culture". Epidemiology and Infection. 135 (7): 1217–1226. doi:10.1017/S0950268806007734. PMC 2870670. PMID 17274856.
- Camargos PA, Almeida MS, Cardoso I, Filho GL, Filho DM, Martins JI, et al. (October 1995). "Latex particle agglutination test in the diagnosis of Haemophilus influenzae type B, Streptococcus pneumoniae and Neisseria meningitidis A and C meningitis in infants and children". Journal of Clinical Epidemiology. 48 (10): 1245–1250. doi:10.1016/0895-4356(95)00016-w. PMID 7561986.
- Diallo K, Feteh VF, Ibe L, Antonio M, Caugant DA, du Plessis M, et al. (March 2021). "Molecular diagnostic assays for the detection of common bacterial meningitis pathogens: A narrative review". EBioMedicine. 65: 103274. doi:10.1016/j.ebiom.2021.103274. PMC 7957090. PMID 33721818.
- Buensalido JA, Malundo AF, Devarajan VR, Lim BA, Emmons WW (2021-06-26). Talavera F, Sanders CV (eds.). "Haemophilus Influenzae Infections: Practice Essentials, Background, Pathophysiology". Medscape.
- "Haemophilus influenzae Disease (Including Hib)". Centers For Disease Control And Prevention. 18 March 2021. Retrieved 20 July 2021.
- Buensalido JA, Malundo AF, Devarajan VR, Lim BA, Emmons WW (26 June 2021). Talavera F, Sanders CV (eds.). "What is Haemophilus influenzae?". Medscape. Archived from the original on 2 December 2021.
- Slack MP, Azzopardi HJ, Hargreaves RM, Ramsay ME (September 1998). "Enhanced surveillance of invasive Haemophilus influenzae disease in England, 1990 to 1996: impact of conjugate vaccines". The Pediatric Infectious Disease Journal. 17 (9 Suppl): S204–S207. doi:10.1097/00006454-199809001-00026. PMID 9781764.
- "Signs and Symptoms". Centers for Disease Control and Prevention (CDC). 2019-01-24.
- Ladhani S, Slack MP, Heath PT, von Gottberg A, Chandra M, Ramsay ME (March 2010). "Invasive Haemophilus influenzae Disease, Europe, 1996-2006". Emerging Infectious Diseases. 16 (3): 455–463. doi:10.3201/eid1603.090290. PMC 3322004. PMID 20202421.
- "Epiglottitis". The Lecturio Medical Concept Library. 22 June 2020. Retrieved 20 July 2021.
- Baucells BJ, Mercadal Hally M, Álvarez Sánchez AT, Figueras Aloy J (November 2016). "[Probiotic associations in the prevention of necrotising enterocolitis and the reduction of late-onset sepsis and neonatal mortality in preterm infants under 1,500g: A systematic review]". Anales de Pediatria. 85 (5): 247–255. doi:10.1016/j.anpedi.2015.07.038. PMID 26611880.
- King P (June 2012). "Haemophilus influenzae and the lung (Haemophilus and the lung)". Clinical and Translational Medicine. 1 (1): 10. doi:10.1186/2001-1326-1-10. PMC 3567431. PMID 23369277.
- Chang CM, Lauderdale TL, Lee HC, Lee NY, Wu CJ, Chen PL, et al. (August 2010). "Colonisation of fluoroquinolone-resistant Haemophilus influenzae among nursing home residents in southern Taiwan". The Journal of Hospital Infection. 75 (4): 304–308. doi:10.1016/j.jhin.2009.12.020. PMID 20356651.
- Murphy TF (2020). "Haemophilus Species, Including H. influenzae and H. ducreyi (Chancroid)". Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases (9th ed.). Philadelphia, PA: Elsevier. ISBN 978-0-323-48255-4.
- Roberts MC, Soge OO, No DB (January 2011). "Characterization of macrolide resistance genes in Haemophilus influenzae isolated from children with cystic fibrosis". The Journal of Antimicrobial Chemotherapy. 66 (1): 100–104. doi:10.1093/jac/dkq425. PMID 21081549.
- "Serious Complications-CDC website". www.cdc.gov.
- Bar-On ES, Goldberg E, Hellmann S, Leibovici L (April 2012). "Combined DTP-HBV-HIB vaccine versus separately administered DTP-HBV and HIB vaccines for primary prevention of diphtheria, tetanus, pertussis, hepatitis B and Haemophilus influenzae B (HIB)". The Cochrane Database of Systematic Reviews. 4 (4): CD005530. doi:10.1002/14651858.CD005530.pub3. PMID 22513932.
- "Haemophilus influenzae type B (HiB)". Health Topics A to Z. Retrieved 2011-03-29.
- Jin Z, Romero-Steiner S, Carlone GM, Robbins JB, Schneerson R (June 2007). "Haemophilus influenzae type a infection and its prevention". Infection and Immunity. 75 (6): 2650–2654. doi:10.1128/IAI.01774-06. PMC 1932902. PMID 17353280.
- Teo E, Lockhart K, Purchuri SN, Pushparajah J, Cripps AW, van Driel ML (June 2017). "Haemophilus influenzae oral vaccination for preventing acute exacerbations of chronic bronchitis and chronic obstructive pulmonary disease". The Cochrane Database of Systematic Reviews. 2017 (6): CD010010. doi:10.1002/14651858.CD010010.pub3. PMC 6481520. PMID 28626902.
- Fleischmann RD, Adams MD, White O, Clayton RA, Kirkness EF, Kerlavage AR, et al. (July 1995). "Whole-genome random sequencing and assembly of Haemophilus influenzae Rd". Science. 269 (5223): 496–512. Bibcode:1995Sci...269..496F. doi:10.1126/science.7542800. PMID 7542800. S2CID 10423613.
- "Haemophilus influenzae Rd KW20, complete sequence". U.S. National Library of Medicine. 2020-04-04.
- Tatusov RL, Mushegian AR, Bork P, Brown NP, Hayes WS, Borodovsky M, et al. (March 1996). "Metabolism and evolution of Haemophilus influenzae deduced from a whole-genome comparison with Escherichia coli". Current Biology. 6 (3): 279–291. doi:10.1016/S0960-9822(02)00478-5. PMID 8805245. S2CID 14057384.
- Poje G, Redfield RJ (2003). Herbert MA, Hood DW, Moxon ER (eds.). "Transformation of Haemophilus influenzae". Methods in Molecular Medicine. Haemophilus influenzae Protocols. Totowa, NJ: Humana Press. 71: 57–70. doi:10.1385/1-59259-321-6:57. ISBN 978-1-59259-321-7. PMID 12374031.
- Naylor EJ, Bakstad D, Biffen M, Thong B, Calverley P, Scott S, et al. (August 2007). "Haemophilus influenzae induces neutrophil necrosis: a role in chronic obstructive pulmonary disease?". American Journal of Respiratory Cell and Molecular Biology. 37 (2): 135–143. doi:10.1165/rcmb.2006-0375OC. PMID 17363778.
- Sánchez-Rincón DA, Cabrera-Juárez E (October 1991). "Lethal and mutagenic action of hydrogen peroxide on Haemophilus influenzae". Journal of Bacteriology. 173 (20): 6632–6634. doi:10.1128/jb.173.20.6632-6634.1991. PMC 209002. PMID 1917884.
- Michod RE, Bernstein H, Nedelcu AM (May 2008). "Adaptive value of sex in microbial pathogens". Infection, Genetics and Evolution. 8 (3): 267–285. doi:10.1016/j.meegid.2008.01.002. PMID 18295550.} As PDF
- "A Study to Evaluate the Safety, Reactogenicity and Immunogenicity of GlaxoSmithkline (GSK) Biologicals' Investigational Vaccine GSK2838504A When Administered to Chronic Obstructive Pulmonary Disease (COPD) Patients With Persistent Airflow Obstruction". ClinicalTrials.gov. 2014-02-27. Retrieved 2016-09-20.
External links
- Hib information on the World Health Organization (WHO) site.
- Fact sheet on the Centers for Disease Control and Prevention (CDC) site.
- Hib Initiative—from Johns Hopkins University, London School of Hygiene & Tropical Medicine, CDC & WHO
- November 2nd: World Pneumonia Day Website
- Centers for Disease Control and Prevention (2012). "Ch. 7: Haemophilus influenzae". In Atkinson W; Wolfe S; Hamborsky J (eds.). Epidemiology and Prevention of Vaccine-Preventable Diseases (12th ed.). Washington, D.C.: Public Health Foundation. pp. 87–100. Archived from the original on 2017-03-10.
- "Haemophilus influenzae". NCBI Taxonomy Browser. 727.
- Type strain of Haemophilus influenzae at BacDive – the Bacterial Diversity Metadatabase
