Whooping cough
Whooping cough, also known as pertussis or the 100-day cough, is a highly contagious bacterial disease.[1][10] Initial symptoms are usually similar to those of the common cold with a runny nose, fever, and mild cough, but these are followed by two or three months of severe coughing fits.[1] Following a fit of coughing, a high-pitched whoop sound or gasp may occur as the person breathes in.[1] The violent coughing may last for 10 or more weeks, hence the phrase "100-day cough".[3] A person may cough so hard that they vomit, break ribs, or become very tired from the effort.[1][2] Children less than one year old may have little or no cough and instead have periods where they cannot breathe.[1] The time between infection and the onset of symptoms is usually seven to ten days.[11] Disease may occur in those who have been vaccinated, but symptoms are typically milder.[1]
| Whooping cough | |
|---|---|
| Other names | Pertussis, 100-day cough |
 | |
| A young boy coughing due to pertussis. | |
| Specialty | Infectious disease |
| Symptoms | Runny nose, fever, cough[1] |
| Complications | Vomiting, broken ribs, exhaustion[1][2] |
| Duration | ~ 10 weeks[3] |
| Causes | Bordetella pertussis (spread through the air)[4] |
| Diagnostic method | Nasopharyngeal swab[5] |
| Prevention | Pertussis vaccine[6] |
| Treatment | Antibiotics (if started early)[7] |
| Frequency | 16.3 million (2015)[8] |
| Deaths | 58,700 (2015)[9] |
Pertussis is caused by the bacterium Bordetella pertussis.[4] It is spread easily through the coughs and sneezes of an infected person.[4][12] People are infectious from the start of symptoms until about three weeks into the coughing fits.[7] Those treated with antibiotics are no longer infectious after five days.[7] Diagnosis is by collecting a sample from the back of the nose and throat.[5] This sample can then be tested by either culture or by polymerase chain reaction.[5]
Prevention is mainly by vaccination with the pertussis vaccine.[6] Initial immunization is recommended between six and eight weeks of age, with four doses to be given in the first two years of life.[13] Protection from pertussis decreases over time, so additional doses of vaccine are often recommended for older children and adults.[14] Vaccination during pregnancy is highly effective at protecting the infant from pertussis during their vulnerable early months of life, and is recommended in many countries.[15] Antibiotics may be used to prevent the disease in those who have been exposed and are at risk of severe disease.[16] In those with the disease, antibiotics are useful if started within three weeks of the initial symptoms, but otherwise have little effect in most people.[7] In pregnant women and children less than one year old, antibiotics are recommended within six weeks of symptom onset.[7] Antibiotics used include erythromycin, azithromycin, clarithromycin, or trimethoprim/sulfamethoxazole.[7] Evidence to support interventions for the cough, other than antibiotics, is poor.[17] About 50% of infected children less than a year old require hospitalization and nearly 0.5% (1 in 200) die.[1][2]
An estimated 16.3 million people worldwide were infected in 2015.[8] Most cases occur in the developing world, and people of all ages may be affected.[6][17] In 2015, pertussis resulted in 58,700 deaths – down from 138,000 deaths in 1990.[9][18] Outbreaks of the disease were first described in the 16th century.[11] The bacterium that causes the infection was discovered in 1906.[11] The pertussis vaccine became available in the 1940s.[11]
Signs and symptoms
The classic symptoms of pertussis are a paroxysmal cough, inspiratory whoop, and fainting, or vomiting after coughing.[19] The cough from pertussis has been documented to cause subconjunctival hemorrhages, rib fractures, urinary incontinence, hernias, and vertebral artery dissection.[19] Violent coughing can cause the pleura to rupture, leading to a pneumothorax. Vomiting after a coughing spell or an inspiratory whooping sound on coughing, almost doubles the likelihood that the illness is pertussis. The absence of a paroxysmal cough or posttussive emesis, though, makes it almost half as likely.[19]
The illness usually starts with mild respiratory symptoms include mild coughing, sneezing, or a runny nose (known as the catarrhal stage). After one or two weeks, the coughing classically develops into uncontrollable fits, sometimes followed by a high-pitched "whoop" sound, as the person tries to inhale. About 50% of children and adults "whoop" at some point in diagnosed pertussis cases during the paroxysmal stage.
This stage usually lasts two to eight weeks, or sometimes longer. A gradual transition then occurs to the convalescent stage, which usually lasts one to four weeks. This stage is marked by a decrease in paroxysms of coughing, although paroxysms may occur with subsequent respiratory infection for many months after the onset of pertussis.[20]
Symptoms of pertussis can be variable, especially between immunized and non-immunized people. Those that are immunized can present with a more mild infection; they may only have the paroxysmal cough for a couple of weeks, and it may lack the "whooping" characteristic.[21] Although immunized people have a milder form of the infection, they can spread the disease to others who are not immune.[21]
Incubation period
The time between exposure and the development of symptoms is on average 7–14 days (range 6–20 days),[22] rarely as long as 42 days.[23]
Cause
Pertussis is caused by the bacterium Bordetella pertussis. It is an airborne disease (through droplets) that spreads easily through the coughs and sneezes of an infected person.[4]
Spread from animals
Uncertainties have existed of B. pertussis and whooping cough as a zoonotic disease since around 1910,[24][25] but in the 1930s knowledge was gained that the bacteria lost their virulent power when repeatedly spread on agar media. This explained the difficulties to reproduce results from different studies as the pre-inoculating handlings of the bacteria were not standardized among scientists.[26]
Today it is established that at least some primate species are highly susceptible to B. pertussis and develop clinical whooping cough in high incidence when exposed to low inoculation doses.[27][28] The bacteria may be present in wild animal populations, but this is not confirmed by laboratory diagnosis, although whooping cough is known among wild gorillas.[29] Several zoos also have a long-standing custom of vaccinating their primates against whooping cough.[30]
Mechanism
After the bacteria are inhaled, they initially adhere to the ciliated epithelium in the nasopharynx. Surface proteins of B. pertussis, including filamentous hemaglutinin and pertactin, mediate attachment to the epithelium. The bacteria then multiply.[31][32] In infants, who experience more severe disease, the bacteria spread down to the lungs.[32]
The bacteria secretes a number of toxins. Tracheal cytotoxin, a fragment of peptidoglycan, kills ciliated epithelial cells and thereby inhibits the mucociliary elevator by which mucus and debris are removed.[33] TCT may contribute to the cough characteristic of pertussis.[34] The cough may also be caused by a yet-to-be identified "cough toxin".[35] Pertussis toxin causes lymphocytosis by an unknown mechanism. The elevated number of white blood cells leads to pulmonary hypertension, a major cause of death by pertussis.[33][32] In infants who develop encephalopathy, cerebral hemorrhage and cortical atrophy occur, likely due to hypoxia.[32]
Diagnosis
Based on symptoms
A physician's overall impression is most effective in initially making the diagnosis.[36] Single factors are much less useful.[36] In adults with a cough of less than 8 weeks, vomiting after coughing or a "whoop" is supportive.[37] If there are no bouts of coughing or there is a fever the diagnosis is unlikely.[37] In children who have a cough of less than 4 weeks vomiting after coughing is somewhat supportive but not definitive.[37]
Lab tests
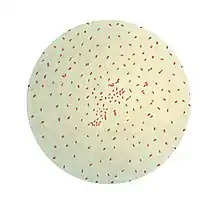
Methods used in laboratory diagnosis include culturing of nasopharyngeal swabs on a nutrient medium (Bordet–Gengou medium), polymerase chain reaction (PCR), direct fluorescent antibody (DFA), and serological methods (e.g. complement fixation test).[38] The bacteria can be recovered from the person only during the first three weeks of illness, rendering culturing and DFA useless after this period, although PCR may have some limited usefulness for an additional three weeks.
Serology may be used for adults and adolescents who have already been infected for several weeks to determine whether antibody against pertussis toxin or another virulence factor of B. pertussis is present at high levels in the blood of the person.[39]
Differential diagnosis
A similar, milder disease is caused by B. parapertussis.[40]
Prevention
The primary method of prevention for pertussis is vaccination.[41] Evidence is insufficient to determine the effectiveness of antibiotics in those who have been exposed, but are without symptoms.[42] Preventive antibiotics, however, are still frequently used in those who have been exposed and are at high risk of severe disease (such as infants).[6]
Vaccine
Pertussis vaccines are effective at preventing illness[43] and are recommended for routine use by the World Health Organization[44] and the United States Centers for Disease Control and Prevention.[45] The vaccine saved an estimated half a million lives in 2002.[44]
The multicomponent acellular pertussis vaccine is 71–85% effective, with greater effectiveness against more severe strains.[43] However, despite widespread vaccination, pertussis has persisted in vaccinated populations and is today "one of the most common vaccine-preventable diseases in Western countries".[46] The 21st-century resurgences in pertussis infections is attributed to a combination of waning immunity and bacterial mutations that elude vaccines.[46][47]
Immunization does not confer lifelong immunity; a 2011 CDC study indicated that protection may only last three to six years. This covers childhood, which is the time of greatest exposure and greatest risk of death from pertussis.[19][48]
An effect of widespread immunization on society has been the shift of reported infections from children aged 1–9 years to infants, adolescents, and adults, with adolescents and adults acting as reservoirs for B. pertussis and infecting infants who have had fewer than three doses of vaccine.[49]
Infection induces incomplete natural immunity that wanes over time.[50] A 2005 study said estimates of the duration of infection-acquired immunity range from 7 to 20 years and the different results could be the result of differences in levels of circulating B. pertussis, surveillance systems, and case definitions used. The study said protective immunity after vaccination wanes after 4–12 years.[51] One study suggested that the availability of vaccine exemptions increases the number of pertussis cases.[52]
Some studies have suggested that while acellular pertussis vaccines are effective at preventing the disease, they have a limited impact on infection and transmission, meaning that vaccinated people could spread pertussis even though they may have only mild symptoms or none at all.[53][54] Pertussis infection in these persons may be asymptomatic, or present as illness ranging from a mild cough to classic pertussis with persistent cough (i.e., lasting more than 7 days). Even though the disease may be milder in older persons, those who are infected may transmit the disease to other susceptible persons, including unimmunized or incompletely immunized infants. Older persons are often found to have the first case in a household with multiple pertussis cases, and are often the source of infection for children.[20]
Treatment
The antibiotics erythromycin, clarithromycin, or azithromycin are typically the recommended treatment.[42] Newer macrolides are frequently recommended due to lower rates of side effects.[6] Trimethoprim-sulfamethoxazole (TMP/SMX) may be used in those with allergies to first-line agents or in infants who have a risk of pyloric stenosis from macrolides.[6]
A reasonable guideline is to treat people age >1 year within 3 weeks of cough onset and infants age <1 year and pregnant women within 6 weeks of cough onset. If the person is diagnosed late, antibiotics will not alter the course of the illness, and even without antibiotics, they should no longer be spreading pertussis.[6] When used early, antibiotics decrease the duration of infectiousness, and thus prevent spread.[6] Short-term antibiotics (azithromycin for 3–5 days) are as effective as long-term treatment (erythromycin 10–14 days) in eliminating B. pertussis with fewer and less severe side effects.[42]
People with pertussis are most infectious during the first two weeks following the onset of symptoms.[55]
Effective treatments of the cough associated with this condition have not been developed.[56] The use of over the counter cough medications is discouraged and has not been found helpful.[21]
Prognosis

While most healthy older children and adults fully recover, infection in newborns is particularly severe. Pertussis is fatal in an estimated 0.5% of US infants under one year of age.[57] First-year infants are also more likely to develop complications, such as: apneas (31%), pneumonia (12%), seizures (0.6%) and encephalopathy (0.15%).[57] This may be due to the ability of the bacterium to suppress the immune system.[58]
Epidemiology

Worldwide, whooping cough affects around 16 million people yearly.[17] One estimate for 2013 stated it resulted in about 61,000 deaths – down from 138,000 deaths in 1990.[18] Another estimated 195,000 child deaths yearly from the disease worldwide.[59] This is despite generally high coverage with the DTP and DTaP vaccines. Pertussis is one of the leading causes of vaccine-preventable deaths worldwide.[60] About 90% of all cases occur in developing countries.[60]
Before vaccines, an average of 178,171 cases was reported in the U.S., with peaks reported every two to five years; more than 93% of reported cases occurred in children under 10 years of age. The actual incidence was likely much higher. After vaccinations were introduced in the 1940s, pertussis incidence fell dramatically to approximately 1,000 by 1976. Incidence rates have increased since 1980. In 2015, 20,762 people were reported to have been infected in the United States.[61]
Pertussis is the only vaccine-preventable disease that is associated with increasing deaths in the U.S. The number of deaths increased from four in 1996 to 17 in 2001, almost all of which were infants under one year.[62] In Canada, the number of pertussis infections has varied between 2,000 and 10,000 reported cases each year over the last ten years, and it is the most common vaccine-preventable illness in Toronto.[63]
In 2009 Australia reported an average of 10,000 cases a year, and the number of cases had increased.[64] In the U.S. pertussis in adults has increased significantly since about 2004.[65]
In 2017, India had a reported 23,766 reported pertussis cases, making it one of the highest reported number of cases of the year.[66] Other countries, such as Germany, had reported 16,183 cases, while Australia and China had a reported number of 12,114 and 10,390 pertussis cases.[66]
US outbreaks
.jpg.webp)
In 2010, 10 babies in California died and health authorities declared an epidemic with 5,978 confirmed, probable and suspected cases.[67][68] They found that doctors had failed to correctly diagnose the babies' condition during several visits.[69] Statistical analysis identified significant overlap in communities with a cluster of nonmedical child exemptions and cases. The number of exemptions varied widely among communities, but tended to be highly clustered. In some schools, more than 75 % of parents filed for vaccination exemptions. The data suggest vaccine refusal based on nonmedical reasons and personal belief exacerbated the outbreak. Other factors included reduced duration of immunity following the acellular vaccine and most vaccinated adults and older children not receiving a booster shot.[70][71]
In April and May 2012, pertussis was declared to be at epidemic levels in Washington, with 3,308 cases.[72][73][74] In December 2012 Vermont declared an epidemic of 522 cases.[75] Wisconsin had the highest incidence rate, with 3,877 cases, although it did not make an official epidemic declaration.[74]
History
Discovery
B. pertussis was discovered in 1906 by Jules Bordet and Octave Gengou, who also developed the first serology and vaccine. Efforts to develop an inactivated whole-cell vaccine began soon after B. pertussis was cultured that year. In the 1920s, Louis W. Sauer developed a weak vaccine for whooping cough at Evanston Hospital (Evanston, IL). In 1925 Danish physician Thorvald Madsen was the first to test a whole-cell vaccine on a wide scale.[76] Madsen used the vaccine to control outbreaks in the Faroe Islands in the North Sea.
Vaccine
In 1932 an outbreak of whooping cough hit Atlanta, Georgia, prompting pediatrician Leila Denmark to begin her study of the disease. Over the next six years her work was published in the Journal of the American Medical Association, and in partnership with Emory University and Eli Lilly & Company, she developed the first pertussis vaccine.[77] In 1942 American scientists Grace Eldering, Loney Gordon, and Pearl Kendrick combined the whole-cell pertussis vaccine with diphtheria and tetanus toxoids to generate the first DTP combination vaccine.[78] To minimize the frequent side effects caused by the pertussis component, Japanese scientist Yuji Sato developed an acellular vaccine consisting of purified haemagglutinins (HAs: filamentous strep throat and leukocytosis-promoting-factor HA), which are secreted by B. pertussis. Sato's acellular pertussis vaccine was used in Japan starting in 1981.[79] Later versions of the acellular vaccine in other countries consisted of additional defined components of B. pertussis and were often part of the DTaP combination vaccine.
References
- "Pertussis (Whooping Cough) Signs & Symptoms". 22 May 2014. Archived from the original on 7 February 2015. Retrieved 12 February 2015.
- "Pertussis (Whooping Cough) Complications". cdc.gov. 28 August 2013. Archived from the original on 9 February 2015. Retrieved 12 February 2015.
- "Pertussis (Whooping Cough) Fast Facts". cdc.gov. 13 February 2014. Archived from the original on 7 February 2015. Retrieved 12 February 2015.
- "Pertussis (Whooping Cough) Causes & Transmission". cdc.gov. 4 September 2014. Archived from the original on 14 February 2015. Retrieved 12 February 2015.
- "Pertussis (Whooping Cough) Specimen Collection". cdc.gov. 28 August 2013. Archived from the original on 8 February 2015. Retrieved 13 February 2015.
- Heininger U (February 2010). "Update on pertussis in children". Expert Review of Anti-Infective Therapy. 8 (2): 163–73. doi:10.1586/eri.09.124. PMID 20109046. S2CID 207217558.
- "Pertussis (Whooping Cough) Treatment". cdc.gov. 28 August 2013. Archived from the original on 11 February 2015. Retrieved 13 February 2015.
- Vos, Theo; Allen, Christine; Arora, Megha; Barber, Ryan M.; Bhutta, Zulfiqar A.; Brown, Alexandria; Carter, Austin; Casey, Daniel C.; Charlson, Fiona J.; Chen, Alan Z.; Coggeshall, Megan; Cornaby, Leslie; Dandona, Lalit; Dicker, Daniel J.; Dilegge, Tina; Erskine, Holly E.; Ferrari, Alize J.; Fitzmaurice, Christina; Fleming, Tom; Forouzanfar, Mohammad H.; Fullman, Nancy; Gething, Peter W.; Goldberg, Ellen M.; Graetz, Nicholas; Haagsma, Juanita A.; Hay, Simon I.; Johnson, Catherine O.; Kassebaum, Nicholas J.; Kawashima, Toana; et al. (October 2016). "Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1545–1602. doi:10.1016/S0140-6736(16)31678-6. PMC 5055577. PMID 27733282.
- Wang, Haidong; Naghavi, Mohsen; Allen, Christine; Barber, Ryan M.; Bhutta, Zulfiqar A.; Carter, Austin; Casey, Daniel C.; Charlson, Fiona J.; Chen, Alan Zian; Coates, Matthew M.; Coggeshall, Megan; Dandona, Lalit; Dicker, Daniel J.; Erskine, Holly E.; Ferrari, Alize J.; Fitzmaurice, Christina; Foreman, Kyle; Forouzanfar, Mohammad H.; Fraser, Maya S.; Fullman, Nancy; Gething, Peter W.; Goldberg, Ellen M.; Graetz, Nicholas; Haagsma, Juanita A.; Hay, Simon I.; Huynh, Chantal; Johnson, Catherine O.; Kassebaum, Nicholas J.; Kinfu, Yohannes; et al. (October 2016). "Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1459–1544. doi:10.1016/s0140-6736(16)31012-1. PMC 5388903. PMID 27733281.
- Carbonetti NH (June 2007). "Immunomodulation in the pathogenesis of Bordetella pertussis infection and disease". Current Opinion in Pharmacology. 7 (3): 272–8. doi:10.1016/j.coph.2006.12.004. PMID 17418639.
- Atkinson W (May 2012). Pertussis Epidemiology and Prevention of Vaccine-Preventable Diseases (12th ed.). Public Health Foundation. pp. 215–230. ISBN 9780983263135. Archived from the original on 29 July 2017.
- "Pertussis". WHO. Archived from the original on 5 June 2015. Retrieved 23 March 2016.
- "Revised guidance on the choice of pertussis vaccines: July 2014" (PDF). Relevé Épidémiologique Hebdomadaire. 89 (30): 337–40. July 2014. PMID 25072068. Archived (PDF) from the original on 13 February 2015.
- "Pertussis vaccines: WHO position paper". Relevé Épidémiologique Hebdomadaire. 85 (40): 385–400. October 2010. PMID 20939150.
- Vygen-Bonnet S, Hellenbrand W, Garbe E, von Kries R, Bogdan C, Heininger U, Röbl-Mathieu M, Harder T (February 2020). "Safety and effectiveness of acellular pertussis vaccination during pregnancy: a systematic review". BMC Infect Dis. 20 (1): 136. doi:10.1186/s12879-020-4824-3. PMC 7020352. PMID 32054444.
- "Pertussis (Whooping Cough) Prevention". cdc.gov. 10 October 2014. Archived from the original on 8 February 2015. Retrieved 13 February 2015.
- Wang K, Bettiol S, Thompson MJ, Roberts NW, Perera R, Heneghan CJ, Harnden A (September 2014). "Symptomatic treatment of the cough in whooping cough". The Cochrane Database of Systematic Reviews. 9 (9): CD003257. doi:10.1002/14651858.CD003257.pub5. PMC 7154224. PMID 25243777.
- GBD 2013 Mortality Causes of Death Collaborators (January 2015). "Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013". Lancet. 385 (9963): 117–71. doi:10.1016/S0140-6736(14)61682-2. PMC 4340604. PMID 25530442.
- Cornia PB, Hersh AL, Lipsky BA, Newman TB, Gonzales R (August 2010). "Does this coughing adolescent or adult patient have pertussis?". JAMA. 304 (8): 890–6. doi:10.1001/jama.2010.1181. PMID 20736473. S2CID 14430946.
- "Pink book | Pertussis | Epidemiology of Vaccine-Preventable Diseases | CDC". 2 March 2019.
- Nguyen, Van Tuong Ngoc; Simon, Lauren (1 September 2018). "Pertussis: The Whooping Cough". Primary Care: Clinics in Office Practice. Infectious Disease. 45 (3): 423–431. doi:10.1016/j.pop.2018.05.003. ISSN 0095-4543. PMID 30115332.
- Heymann, David L. (ed): Pertussis; in Control of Communicable Diseases Manual. p. 457. American Public Health Association, Washington DC, 2008, ISBN 978-0-87553-189-2
- "Pertussis (whooping cough)". New York State Department of Health. Archived from the original on 22 July 2013. Retrieved 8 June 2013.
- Inaba I (1912). "Über den Bordet-Gengouschen Keuchhustenbacillus Übertragungsversuches des Keuchenhustens auf Tiere". Z Kinderheilkd. 4: 252–264. doi:10.1007/bf02088879. S2CID 42345587.
- Bachamn W, Burghard E (1925). "Der Nachweis der Bordet-Gengouschen Bacillen und ihre aetiologische Bedeutung für den Keuchenhusten". Z Kinderheilkd. 39: 465–483. doi:10.1007/BF02225286. S2CID 30221200.
- Shibley GS, Hoelscher H (September 1934). "Studies on whooping cough. I. Type-specific (S) and dissociation (R) forms of haemophilus pertussis". The Journal of Experimental Medicine. 60 (4): 403–18. doi:10.1084/jem.60.4.403. PMC 2132401. PMID 19870311.
- Gustavsson OE, Röken BO, Serrander R (1990). "An epizootic of whooping cough among chimpanzees in a zoo". Folia Primatologica; International Journal of Primatology. 55 (1): 45–50. doi:10.1159/000156498. PMID 2394416.
- Warfel JM, Merkel TJ (October 2014). "The baboon model of pertussis: effective use and lessons for pertussis vaccines". Expert Review of Vaccines. 13 (10): 1241–52. doi:10.1586/14760584.2014.946016. PMID 25182980. S2CID 24133254.
- Butynski TM et al. (eds.): Mammals of Africa vol. II: Primates, p. 51. Bloomsbury Publishing, London, 2013. ISBN 978-1-4081-2252-5
- Loomis MR (1985). "Immunoprofylaxis in infant great apes". In Graham CE, Bowen JA (eds.). Clinical Management of Infant Great Apes. Monographs in Primatology. Vol. 5. New York: Liss. pp. 107–112.
- Top KA, Halperin SA (2017). "Pertussis and other Bordetella infections". In Kasper DL, Fauci AS (eds.). Harrison's Infectious Diseases (3 ed.). New York: McGraw-Hill Education. pp. 502–506. ISBN 9781259835971.
- Kilgore PE, Salim AM, Zervos MJ, Schmitt HJ (July 2016). "Pertussis: Microbiology, Disease, Treatment, and Prevention". Clinical Microbiology Reviews. 29 (3): 449–86. doi:10.1128/CMR.00083-15. PMC 4861987. PMID 27029594.
- Hewlett EL, Burns DL, Cotter PA, Harvill ET, Merkel TJ, Quinn CP, Stibitz ES (April 2014). "Pertussis pathogenesis—what we know and what we don't know". The Journal of Infectious Diseases. 209 (7): 982–5. doi:10.1093/infdis/jit639. PMC 3952676. PMID 24626533.
- Melvin JA, Scheller EV, Miller JF, Cotter PA (April 2014). "Bordetella pertussis pathogenesis: current and future challenges". Nature Reviews. Microbiology. 12 (4): 274–88. doi:10.1038/nrmicro3235. PMC 4205565. PMID 24608338.
- Cherry JD (2013). "Pertussis: challenges today and for the future". PLOS Pathogens. 9 (7): e1003418. doi:10.1371/journal.ppat.1003418. PMC 3723573. PMID 23935481.
- Ebell MH, Marchello C, Callahan M (2017). "Clinical Diagnosis of Bordetella Pertussis Infection: A Systematic Review". Journal of the American Board of Family Medicine. 30 (3): 308–319. doi:10.3122/jabfm.2017.03.160330. PMID 28484063.
- Moore A, Harnden A, Grant CC, Patel S, Irwin RS (January 2019). "Clinically Diagnosing Pertussis-associated Cough in Adults and Children: CHEST Guideline and Expert Panel Report". Chest. 155 (1): 147–154. doi:10.1016/j.chest.2018.09.027. PMC 6859243. PMID 30321509.
- Pedro-Pons, Agustín (1968). Patología y Clínica Médicas (in Spanish). Vol. 6 (3rd ed.). Barcelona: Salvat. p. 615. ISBN 84-345-1106-1.
- "Pertussis". Euro Diagnostica. Euro Diagnostica AB. Archived from the original on 4 March 2016. Retrieved 29 February 2016.
- Finger H, von Koenig CH (1996). "Bordetella". In Baron S, et al. (eds.). Bordetella–Clinical Manifestations. In: Barron's Medical Microbiology (4th ed.). Univ of Texas Medical Branch. ISBN 0-9631172-1-1. Archived from the original on 14 October 2007.
- "Pertussis | Whooping Cough | Vaccination | CDC". www.cdc.gov. Archived from the original on 26 May 2017. Retrieved 27 May 2017.
- Altunaiji S, Kukuruzovic R, Curtis N, Massie J (July 2007). "Antibiotics for whooping cough (pertussis)". The Cochrane Database of Systematic Reviews (3): CD004404. doi:10.1002/14651858.CD004404.pub3. PMID 17636756.
- Zhang L, Prietsch SO, Axelsson I, Halperin SA (September 2014). "Acellular vaccines for preventing whooping cough in children". The Cochrane Database of Systematic Reviews. 9 (9): CD001478. doi:10.1002/14651858.CD001478.pub6. PMID 25228233.
- "Annex 6 whole cell pertussis" (PDF). World Health Organization. Archived (PDF) from the original on 24 March 2012. Retrieved 5 June 2011.
- "Pertussis: Summary of Vaccine Recommendations". Centers for Disease Control and Prevention. Archived from the original on 29 June 2011. Retrieved 5 June 2011.
- Mooi FR, Van Der Maas NA, De Melker HE (April 2014). "Pertussis resurgence: waning immunity and pathogen adaptation – two sides of the same coin". Epidemiology and Infection. Oxford University Press. 142 (4): 685–94. doi:10.1017/S0950268813000071. PMID 23406868. S2CID 206283573.
- van der Ark AA, Hozbor DF, Boog CJ, Metz B, van den Dobbelsteen GP, van Els CA (September 2012). "Resurgence of pertussis calls for re-evaluation of pertussis animal models". Expert Review of Vaccines. 11 (9): 1121–37. doi:10.1586/erv.12.83. PMID 23151168. S2CID 10457474.
- Versteegh FG, Schellekens JF, Fleer A, Roord JJ (2005). "Pertussis: a concise historical review including diagnosis, incidence, clinical manifestations and the role of treatment and vaccination in management". Rev Med Microbiol. 16 (3): 79–89. doi:10.1097/01.revmedmi.0000175933.85861.4e. S2CID 71775827.
- Mattoo S, Cherry JD (April 2005). "Molecular pathogenesis, epidemiology, and clinical manifestations of respiratory infections due to Bordetella pertussis and other Bordetella subspecies". Clinical Microbiology Reviews. 18 (2): 326–82. doi:10.1128/CMR.18.2.326-382.2005. PMC 1082800. PMID 15831828.
- Brenzel L, Wolfson LJ, Fox-Rushby J, et al. (2006). "Vaccine-Preventable Diseases". In Jamison DT, Breman JG, Measham AR, et al. (eds.). Disease Control Priorities in Developing Countries (2nd ed.). Washington DC: International Bank for Reconstruction and Development, World Bank. Table 20.1 Selected Vaccine-preventable Diseases and Vaccines. ISBN 9780821361795. PMID 21250343.
- Wendelboe AM, Van Rie A, Salmaso S, Englund JA (May 2005). "Duration of immunity against pertussis after natural infection or vaccination". The Pediatric Infectious Disease Journal. 24 (5 Suppl): S58-61. doi:10.1097/01.inf.0000160914.59160.41. PMID 15876927. S2CID 45434262.
- Yang YT, Debold V (February 2014). "A longitudinal analysis of the effect of nonmedical exemption law and vaccine uptake on vaccine-targeted disease rates". American Journal of Public Health. 104 (2): 371–7. doi:10.2105/AJPH.2013.301538. PMC 3935668. PMID 24328666.
- Srugo I, Benilevi D, Madeb R, Shapiro S, Shohat T, Somekh E, et al. (October 2000). "Pertussis infection in fully vaccinated children in day-care centers, Israel". Emerging Infectious Diseases. 6 (5): 526–9. doi:10.3201/eid0605.000512. PMC 2627963. PMID 10998384.
- "Pertussis Vaccines:WHO Position Paper" (PDF). August 2015. Archived (PDF) from the original on 4 March 2016.
It is plausible that in humans, as in nonhuman primates, asymptomatic or mildly symptomatic infections in DTaP-immunized persons may result in transmission of B. pertussis to others and may drive pertussis outbreaks.
- "Pertussis | Whooping Cough | Causes and Transmission | CDC". www.cdc.gov. 1 February 2019. Retrieved 24 April 2020.
- Wang K, Bettiol S, Thompson MJ, Roberts NW, Perera R, Heneghan CJ, Harnden A (September 2014). "Symptomatic treatment of the cough in whooping cough". The Cochrane Database of Systematic Reviews. 9 (9): CD003257. doi:10.1002/14651858.CD003257.pub5. PMC 7154224. PMID 25243777.
- "Pertussis: Complications". Centers for Disease Control and Prevention. Archived from the original on 14 August 2012. Retrieved 24 August 2012.
- Carbonetti NH (March 2010). "Pertussis toxin and adenylate cyclase toxin: key virulence factors of Bordetella pertussis and cell biology tools". Future Microbiology. 5 (3): 455–69. doi:10.2217/fmb.09.133. PMC 2851156. PMID 20210554.
- "Pertussis | Whooping Cough | Cases in Other Countries | CDC". www.cdc.gov. Archived from the original on 1 March 2016. Retrieved 1 March 2016.
- "Pertussis in Other Countries". Centers for Disease Control and Prevention (CDC). Archived from the original on 12 May 2013. Retrieved 27 May 2013.
- "Pertussis | Whooping Cough | Surveillance | Cases by Year | CDC". www.cdc.gov. Archived from the original on 10 April 2017. Retrieved 10 April 2017.
- Gregory DS (August 2006). "Pertussis: a disease affecting all ages". American Family Physician. 74 (3): 420–6. PMID 16913160. Archived from the original on 16 May 2008.
- Whooping Cough – Causes, Symptoms, Treatment, Diagnosis – – C-Health Archived 7 July 2012 at archive.today
- Lavelle P (20 January 2009). "A bad year for whooping cough". Australian Broadcasting Corporation. Archived from the original on 26 October 2009.
- Kate Murphy (22 February 2005). "Enduring and Painful, Pertussis Leaps Back". The New York Times. Archived from the original on 24 May 2013.
- Esposito S, Stefanelli P, Fry NK, Fedele G, He Q, Paterson P, et al. (3 July 2019). "Pertussis Prevention: Reasons for Resurgence, and Differences in the Current Acellular Pertussis Vaccines". Frontiers in Immunology. 10: 1344. doi:10.3389/fimmu.2019.01344. PMC 6616129. PMID 31333640.
- Falco M (20 October 2010). "Ten infants dead in California whooping cough outbreak". CNN. Archived from the original on 21 October 2010. Retrieved 21 October 2010.
Whooping cough, also known as pertussis, has claimed the 10th victim in California, in what health officials are calling the worst outbreak in 60 years.
- "Pertussis (Whooping Cough) Outbreaks". Centers for Disease Control and Prevention. 11 January 2011. Archived from the original on 19 July 2017.
- Lin II R (7 September 2010). "Diagnoses lagged in baby deaths". Los Angeles Times. Archived from the original on 10 September 2010. Retrieved 8 September 2010.
- Shute N (30 September 2013). "Vaccine Refusals Fueled California's Whooping Cough Epidemic". NPR. Archived from the original on 5 October 2013. Retrieved 6 October 2013.
- Atwell JE, Van Otterloo J, Zipprich J, Winter K, Harriman K, Salmon DA, et al. (October 2013). "Nonmedical vaccine exemptions and pertussis in California, 2010". Pediatrics. 132 (4): 624–30. doi:10.1542/peds.2013-0878. PMID 24082000.
- Donna Gordon Blankinship (10 May 2012). "Whooping cough epidemic declared in Washington". Associated Press, Seattle Times. Archived from the original on 13 May 2012. Retrieved 14 May 2012.
- Washington State Department of Health (April 2012). "Whooping cough cases reach epidemic levels in much of Washington" (PDF). Washington State Department of Health. Archived from the original (PDF) on 20 January 2015. Retrieved 14 May 2012.
- Herzog K (17 August 2012). "Wisconsin has highest rate of whooping cough". the Journal Sentinel. Archived from the original on 19 August 2012. Retrieved 17 August 2012.
- Johnson T (13 December 2012). "Whooping cough epidemic declared in Vermont". Burlington Free Press. Retrieved 14 December 2012.
- Baker JP, Katz SL (February 2004). "Childhood vaccine development: an overview". Pediatric Research. 55 (2): 347–56. doi:10.1203/01.PDR.0000106317.36875.6A. PMID 14630981.
- "Changing the Face of Medicine | Dr. Leila Alice Daughtry Denmark". www.nlm.nih.gov. Archived from the original on 21 March 2015. Retrieved 3 February 2016.
- Bannink J. "Finding aid for the Michigan women and the whooping cough vaccine collection[s]" (PDF). Archived (PDF) from the original on 5 February 2015.
- Sato Y, Kimura M, Fukumi H (January 1984). "Development of a pertussis component vaccine in Japan". Lancet. 1 (8369): 122–6. doi:10.1016/S0140-6736(84)90061-8. PMID 6140441. S2CID 23621152.
External links
- Pertussis at Todar's Online Textbook of Bacteriology
- PBS NOVA – Vaccines: Calling The Shots
- "Whooping Cough". MedlinePlus. U.S. National Library of Medicine.