Lamellar ichthyosis
Lamellar ichthyosis, also known as ichthyosis lamellaris and nonbullous congenital ichthyosis, is a rare inherited skin disorder, affecting around 1 in 600,000 people.
| Ichthyosis lamellaris | |
|---|---|
| Other names | Ichthyosis lamellaris |
 | |
| Ichthyosis lamellaris has an autosomal recessive pattern of inheritance. | |
| Specialty | Medical genetics |
| Usual onset | Present at birth |
| Causes | Genetics |
Presentation
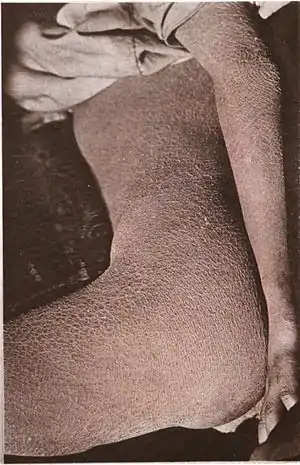
Affected babies are born in a collodion membrane, a shiny, waxy-appearing outer layer to the skin. This is shed 10–14 days after birth, revealing the main symptom of the disease, extensive scaling of the skin caused by hyperkeratosis. With increasing age, the scaling tends to be concentrated around joints in areas such as the groin, the armpits, the inside of the elbow and the neck. The scales often tile the skin and may resemble fish scales.
Collodion baby
In medicine, the term collodion baby applies to newborns who appear to have an extra layer of skin (known as a collodion membrane) that has a collodion-like quality. It is a descriptive term, not a specific diagnosis or disorder (as such, it is a syndrome).[1]
Appearance and treatment at birth
The appearance is often described as a shiny film looking like a layer of Vaseline. The eyelids and mouth may have the appearance of being forced open due to the tightness of the skin. There can be associated eversion of the eyelids (ectropion).
Collodion babies can have severe medical consequences, mainly because the baby can lose heat and fluid through the abnormal skin. This can lead to hypothermia and dehydration.[2] Strategies to prevent these problems are the use of emollients or nursing the baby in a humidified incubator.[3] There is also an increased risk of skin infection and mechanical compression, leading to problems like limb ischemia.[1][2][3] There is also a risk of intoxication by cutaneous absorption of topical products, for example salicylate intoxication (similar to aspirin overdose) due to keratolytics.[4]
The condition is not thought to be painful or in itself distressing to the child. Nursing usually takes place in a neonatal intensive care unit, and good intensive care seems to have improved the prognosis markedly.[1] The collodion membrane should peel off or "shed" 2 to 4 weeks after birth, revealing the underlying skin disorder.
The condition can resemble but is different from harlequin type ichthyosis.
Long term course
The appearance can be caused by several skin diseases, and it is most often not associated with other birth defects.[2] In most cases, the baby develops an ichthyosis or ichthyosis-like condition or other rare skin disorder.
Most cases (approximately 75%) of collodion baby will go on to develop a type of autosomal recessive congenital ichthyosis (either lamellar ichthyosis or congenital ichthyosiform erythrodema).[5]
In around 10% of cases the baby sheds this layer of skin and has normal skin for the rest of its life.[2][5] This is known as self-healing collodion baby.
The remaining 15% of cases are caused by a variety of diseases involving keratinization disorders.[5] Known causes of collodion baby include ichthyosis vulgaris and trichothiodystrophy.[3] Less well documented causes include Sjögren-Larsson syndrome, Netherton syndrome, Gaucher disease type 2, congenital hypothyroidism, Conradi syndrome, Dorfman-Chanarin syndrome, ketoadipiaciduria, koraxitrachitic syndrome, ichthyosis variegata and palmoplantar keratoderma with anogenital leukokeratosis.[3] Since many of these conditions have an autosomal recessive inheritance pattern, they are rare and can be associated with consanguinity.[3]
Tests that can be used to find the cause of collodion baby include examination of the hairs, blood tests and a skin biopsy.
Associated medical problems
Overheating: The scaling of the skin prevents normal sweating so hot weather and/or vigorous exercise can cause problems.
Eye problems: The eyelids can be pulled down by the tightness of the skin and this can make eyelids (but usually just the lower one) very red and they are prone to drying and irritation.
Constriction bands: Very rarely children with this condition can have tight bands of skin around their fingers or toes (usually at the tips) that can prevent proper blood circulation to the area.
Hair loss: Severe scaling of the skin on the scalp can lead to patchy loss of hair, but this is rarely permanent.
Genetics
This condition is an autosomal recessive genetic disorder,[6]: 561 which means the defective gene is located on an autosome, and both parents must carry one copy of the defective gene in order to have a child born with the disorder. Carriers of a recessive gene usually do not show any signs or symptoms of the disorder.
One form of ichthyosis lamellaris (LI1) is associated with a deficiency of the enzyme keratinocyte transglutaminase.
Genes involved include:
| Type | OMIM | Gene | Locus |
|---|---|---|---|
| LI1 | 242300 | TGM1 | 14 |
| LI2 | 601277 | ABCA12 | 2q34 |
| LI3 | 604777 | CYP4F22 | 19p13.12 |
| LI5 | 606545 | ? | 17p |
Treatments
As with all types of ichthyosis, there is no cure but the symptoms can be relieved.
- Moisturizers
- Prevention of overheating
- Eye drops (to prevent the eyes from becoming dried out)
- Systemic Retinoids (isotretinoin and acitretin are very effective, but careful monitoring for toxicity is required. Only severe cases may require intermittent therapy.)[7]
Psychological therapy or support may be required as well. Ophthalmology Consult ENT consult Adequate nutrition Monitor electrolytes < Collodion baby: An update with a focus on practical management. Renata Prado MD, Lixia Z Ellis MD, PhD, Ryan Gamble MD, Tracy Funk MD, Harvey Alan Arbuckle MD, Anna L Bruckner. Journal of the American Academy of Dermatology 2012;67:1362-1374>
See also
References
- Larrègue M, Ottavy N, Bressieux JM, Lorette J (1986). "[Collodion baby: 32 new case reports]". Ann Dermatol Venereol (in French). 113 (9): 773–85. PMID 3548541.
- Van Gysel D, Lijnen RL, Moekti SS, de Laat PC, Oranje AP (September 2002). "Collodion baby: a follow-up study of 17 cases". J Eur Acad Dermatol Venereol. 16 (5): 472–5. doi:10.1046/j.1468-3083.2002.00477.x. PMID 12428840. S2CID 12110995.
- Taïeb A, Labrèze C (September 2002). "Collodion baby: what's new". J Eur Acad Dermatol Venereol. 16 (5): 436–7. doi:10.1046/j.1468-3083.2002.00478.x. PMID 12428832. S2CID 35972808.
- Yamamura S, Kinoshita Y, Kitamura N, Kawai S, Kobayashi Y (2002). "Neonatal salicylate poisoning during the treatment of a collodion baby". Clin Pediatr (Phila). 41 (6): 451–2. doi:10.1177/000992280204100615. PMID 12166800. S2CID 34810587.
- Dermatology at the Millennium, By Delwyn Dyall-Smith, Robin Marks, Page 586, Published by Informa Health Care, 1999, ISBN 1-85070-005-2
- James, William; Berger, Timothy; Elston, Dirk (2005). Andrews' Diseases of the Skin: Clinical Dermatology. (10th ed.). Saunders. ISBN 0-7216-2921-0.
- Fitzpatrick clinical dermatology