Sjögren–Larsson syndrome
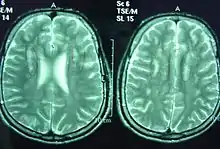
Sjögren–Larsson syndrome is a rare autosomal recessive form of ichthyosis with neurological symptoms.[1]: 485 [2]: 564 [3] It can be identified by a triad of medical disorders. The first is ichthyosis, which is a buildup of skin to form a scale-like covering that causes dry skin and other problems. The second identifier is paraplegia which is characterized by leg spasms. The final identifier is intellectual delay.
| Sjögren–Larsson syndrome | |
|---|---|
| Other names | SLS |
 | |
| Two brothers (21 and 25 years old) with generalized dryness of skin with fine scales mainly around the umbilicus and in the flexural folds, one of Sjögren–Larsson syndrome characteristics. | |
| Specialty | Medical genetics |
SLS is caused by a mutation in the fatty aldehyde dehydrogenase gene found on chromosome 17.[4] In order for a child to receive SLS both parents must be carriers of the SLS gene. If they are carriers their child has a 1⁄4 chance of getting the disease. In 1957 Sjögren and Larsson proposed that the Swedes with the disease all descended from a common ancestor 600 years ago. Today only 30–40 persons in Sweden have this disease.[5]
Signs and symptoms
- Dry and scaly skin similar to all other ichtyosiforms (types of ichthyosis).
- Neurological problems – this can often cause mild paralysis in the legs
- Mild to moderate intellectual disability.
- Often associated ocular features, which include pigmentary changes in the retina.
The usual presentation of crystalline maculopathy is from the age of 1–2 years onwards.
Causes
It is associated with a deficiency of the enzyme fatty aldehyde dehydrogenase (ALDH3A2) which is encoded on the short arm of chromosome 17 (17p11.2). At least 11 distinct mutations have been identified.[6]
Without a functioning fatty aldehyde dehydrogenase enzyme, the body is unable to break down medium- and long-chain fatty aldehydes which then build up in the membranes of the skin and brain.[4]
This condition is inherited in an autosomal recessive pattern.[7]
Diagnosis
Diagnosis is made with a blood test which sees if the activity of the fatty aldehyde dehydrogenase enzyme is normal.[4] Gene sequencing can also be used, which can additionally be used by would-be parents to see if they are carriers.[4]
Treatment
The ichthyosis is usually treated with topical ointment.[4] Anti-convulsants are used to treat seizures[4] and the spasms may be improved with surgery.[4]
Eponym
It was characterized by Torsten Sjögren and Tage Konrad Leopold Larsson (1905–1998), a Swedish medical statistician.[8][9] It should not be confused with Sjögren's syndrome, which is a distinct condition named after a different person, Henrik Sjögren.
References
- Freedberg, et al. (2003). Fitzpatrick's Dermatology in General Medicine. (6th ed.). McGraw-Hill. ISBN 0-07-138076-0.
- James, William; Berger, Timothy; Elston, Dirk (2005). Andrews' Diseases of the Skin: Clinical Dermatology. (10th ed.). Saunders. ISBN 0-7216-2921-0.
- Rapini, Ronald P.; Bolognia, Jean L.; Jorizzo, Joseph L. (2007). Dermatology: 2-Volume Set. St. Louis: Mosby. ISBN 978-1-4160-2999-1.
- "Sjogren-Larsson syndrome | Genetic and Rare Diseases Information Center (GARD) – an NCATS Program". rarediseases.info.nih.gov. Retrieved 2020-10-31.
- "Sjögren-Larssons syndrom".
- Sillén A, Anton-Lamprecht I, Braun-Quentin C, et al. (1998). "Spectrum of mutations and sequence variants in the FALDH gene in patients with Sjögren–Larsson syndrome". Hum. Mutat. 12 (6): 377–84. doi:10.1002/(SICI)1098-1004(1998)12:6<377::AID-HUMU3>3.0.CO;2-I. PMID 9829906. S2CID 37451614.
- Orphanet: Portal de enfermedades raras y medicamentos huérfanos
- synd/1678 at Who Named It?
- SJOGREN T, LARSSON T (1957). "Oligophrenia in combination with congenital ichthyosis and spastic disorders; a clinical and genetic study". Acta Psychiatr Neurol Scand Suppl. 113: 1–112. PMID 13457946.
Further reading
- Sjögren, K. G. Torsten; Larsson, Tage K. (1957). "Oligophrenia in combination with congenital ichtyosis and spastic disorders; a clinical and genetic study". Acta Psychiatrica Scandinavica. Copenhagen. 32 (supplement 113): 9–105. doi:10.1111/j.1600-0447.1956.tb04725.x. PMID 13457946. S2CID 72058188.