Saint Louis encephalitis
Saint Louis encephalitis is a disease caused by the mosquito-borne Saint Louis encephalitis virus. Saint Louis encephalitis virus is related to Japanese encephalitis virus and is a member of the family Flaviviridae. This disease mainly affects the United States, including Hawaii.[3] Occasional cases have been reported from Canada, Mexico and the Caribbean, including the Greater Antilles, Trinidad and Tobago, and Jamaica.[3]
| Saint Louis encephalitis virus | |
|---|---|
_virus_EM_PHIL_1871_lores.JPG.webp) | |
| Electron micrograph of Saint Louis encephalitis virus seen in a mosquito salivary gland | |
| Virus classification | |
| (unranked): | Virus |
| Realm: | Riboviria |
| Kingdom: | Orthornavirae |
| Phylum: | Kitrinoviricota |
| Class: | Flasuviricetes |
| Order: | Amarillovirales |
| Family: | Flaviviridae |
| Genus: | Flavivirus |
| Species: | Saint Louis encephalitis virus |
| Synonyms | |
| Saint Louis encephalitis | |
|---|---|
| Specialty | Infectious diseases |
Signs and symptoms
The majority of infections result in mild illness, including fever and headache. When infection is more severe the person may experience headache, high fever, neck stiffness, stupor, disorientation, coma, tremors, occasional convulsions and spastic paralysis. Fatality ranges from 3–30%. Elderly people are more likely to have a fatal infection.
Transmission
Mosquitoes, primarily from the genus Culex, become infected by feeding on birds infected with the Saint Louis encephalitis virus. The most common vector of this disease within the genus Culex is Culex pipiens, also known as the common house mosquito.[4] Infected mosquitoes then transmit the Saint Louis encephalitis virus to humans and animals during the feeding process. The Saint Louis encephalitis virus grows both in the infected mosquito and the infected bird, but does not make either one sick. Only infected mosquitoes can transmit Saint Louis encephalitis virus. Once a human has been infected with the virus it is not transmissible from that individual to other humans.
Genetics
Five evolutionary genetic studies of SLE virus have been published of which four[5][6][7][8] focused on phylogeny, genetic variation, and recombination dynamics by sequencing the envelope protein gene and parts of other genes.
A recent evolutionary study[9] based on 23 new full open reading frame sequences (near-complete genomes) found that the North American strains belonged to a single clade. Strains were isolated at different points in time (from 1933 to 2001) which allowed for the estimation of divergence times of SLE virus clades and the overall evolutionary rate. Furthermore, this study found an increase in the effective population size of the SLE virus around the end of the 19th century that corresponds to the split of the latest North American clade, suggesting a northwards colonization of SLE virus in the Americas, and a split from the ancestral South American strains around 1892.[10] Scans for natural selection showed that most codons of the SLE virus ORF were evolving neutrally or under negative selection. Positive selection was statistically detected only at one single codon coding for amino acids belonging to the hypothesized N-linked glycosylation site of the envelope protein. Nevertheless, the latter can be due to selection in vitro (laboratory) rather than in vivo (host). In an independent study[8] 14 out of 106 examined envelope gene sequences were found not to contain a specific codon at position 156 coding for this glycosylation site (Ser→Phe/Tyr).
Another study estimated the evolutionary rate to be 4.1 × 10−4 substitutions/site/year (95% confidence internal 2.5-5.7 × 10−4 substitutions/site/year).[11] The virus seems to have evolved in northern Mexico and then spread northwards with migrating birds.
Treatment
There are no vaccines or any other treatments specifically for Saint Louis encephalitis virus, although one study showed that early use of interferon alfa-2b may decrease the severity of complications.[12]
Epidemiology
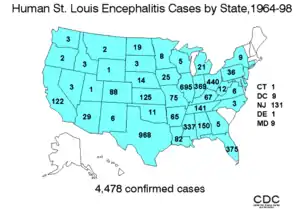
In the United States an average of 128 cases of Saint Louis encephalitis are recorded annually. In temperate areas of the United States, Saint Louis encephalitis cases occur primarily in the late summer or early fall. In the southern United States where the climate is milder Saint Louis encephalitis can occur year-round.
History
The name of the virus goes back to 1933 when within five weeks in autumn an encephalitis epidemic of explosive proportions broke out in the vicinity of St. Louis, Missouri, and the neighboring St. Louis County.[13][14] Over 1,000 cases were reported to the local health departments and the newly constituted National Institutes of Health of the United States was appealed to for epidemiological and investigative expertise.[15] The previously unknown virus that caused the epidemic was isolated by the NIH team first in monkeys and then in white mice.[16]
References
- Siddell, Stuart (April 2017). "Change the names of 43 virus species to accord with ICVCN Code, Section 3-II, Rule 3.13 regarding the use of ligatures, diacritical marks, punctuation marks (excluding hyphens), subscripts, superscripts, oblique bars and non-Latin letters in taxon names" (ZIP). International Committee on Taxonomy of Viruses (ICTV). Retrieved 29 April 2019.
- ICTV 5th Report Francki, R. I. B., Fauquet, C. M., Knudson, D. L. & Brown, F. (eds)(1991). Classification and nomenclature of viruses. Fifthreport of the International Committee on Taxonomy of Viruses. Archives of Virology Supplementum 2, p226 https://talk.ictvonline.org/ictv/proposals/ICTV%205th%20Report.pdf
- Mavian, Carla; Dulcey, Melissa; Munoz, Olga; Salemi, Marco; Vittor, Amy; Capua, Ilaria (25 December 2018). "Islands as Hotspots for Emerging Mosquito-Borne Viruses: A One-Health Perspective". Viruses. 11 (1): 11. doi:10.3390/v11010011. PMC 6356932. PMID 30585228.
- "Saint Louis Encephalitis". Centers for Disease Control and Prevention. November 20, 2009. Retrieved July 14, 2017.
- Kramer LD, Presser SB, Hardy JL, Jackson AO (1997). "Genotypic and phenotypic variation of selected Saint Louis encephalitis viral strains isolated in California". Am. J. Trop. Med. Hyg. 57 (2): 222–9. doi:10.4269/ajtmh.1997.57.222. PMID 9288820.
- Kramer LD, Chandler LJ (2001). "Phylogenetic analysis of the envelope gene of St. Louis encephalitis virus". Arch. Virol. 146 (12): 2341–55. doi:10.1007/s007050170007. PMID 11811684. S2CID 24755534.
- Twiddy SS, Holmes EC (2003). "The extent of homologous recombination in members of the genus Flavivirus". J. Gen. Virol. 84 (Pt 2): 429–40. doi:10.1099/vir.0.18660-0. PMID 12560576.
- May FJ, Li L, Zhang S, Guzman H, Beasley DW, Tesh RB, Higgs S, Raj P, Bueno R, Randle Y, Chandler L, Barrett AD (2008). "Genetic variation of St. Louis encephalitis virus". J. Gen. Virol. 89 (Pt 8): 1901–10. doi:10.1099/vir.0.2008/000190-0. PMC 2696384. PMID 18632961.
- Baillie GJ, Kolokotronis SO, Waltari E, Maffei JG, Kramer LD, Perkins SL (2008). "Phylogenetic and evolutionary analyses of St. Louis encephalitis virus genomes". Mol. Phylogenet. Evol. 47 (2): 717–28. doi:10.1016/j.ympev.2008.02.015. PMID 18374605.
- "Solving The Mystery Of St. Louis Encephalitis". American Museum of Natural History. 30 July 2008. Retrieved 28 July 2019.
- Auguste AJ, Pybus OG, Carrington CV (2009). "Evolution and dispersal of St. Louis encephalitis virus in the Americas". Infect. Genet. Evol. 9 (4): 709–15. doi:10.1016/j.meegid.2008.07.006. PMID 18708161.
- Rahal JJ, Anderson J, Rosenberg C, Reagan T, Thompson LL (2004). "Effect of interferon-alpha2b therapy on St. Louis viral meningoencephalitis: clinical and laboratory results of a pilot study". J. Infect. Dis. 190 (6): 1084–7. doi:10.1086/423325. PMID 15319857.
- "Encephalitis in St. Louis". American Journal of Public Health and the Nation's Health. 23 (10): 1058–60. October 1933. doi:10.2105/ajph.23.10.1058. PMC 1558319. PMID 18013846.
- Washington Post Magazine, October 8, 1933
- Bredeck JF (November 1933). "The Story of the Epidemic of Encephalitis in St. Louis". American Journal of Public Health and the Nation's Health. 23 (11): 1135–40. doi:10.2105/AJPH.23.11.1135. PMC 1558406. PMID 18013860.
- Edward A. Beeman: Charles Armstrong, M.D.: A Biography; 2007; p. 305; also online here (PDF).
External links
- United States Centers for Disease Control and Prevention. Saint Louis encephalitis.
- St. Louis Encephalitis at eMedicine
- The Encephalitis Society - A Global resource on Encephalitis
- "St. Louis encephalitis virus". NCBI Taxonomy Browser. 11080.