Alcoholism
| Alcoholism | |
|---|---|
| Other names: Alcohol dependence syndrome, alcohol use disorder (AUD)[1] | |
 | |
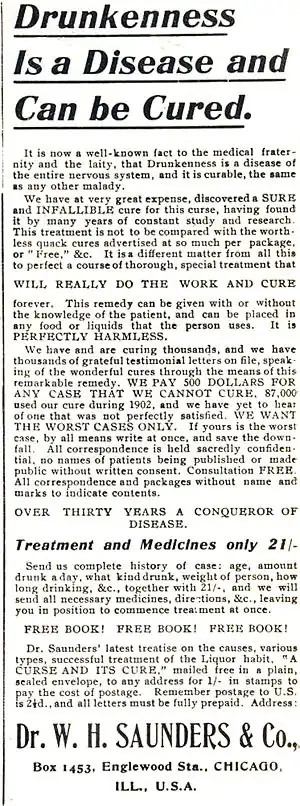
| "King Alcohol and His Prime Minister" c. 1820 | |
| Specialty | Psychiatry, toxicology, addiction medicine |
| Symptoms | Drinking large amounts of alcohol over a long period, difficulty cutting down, acquiring and drinking alcohol taking up a lot of time, usage resulting in problems, withdrawal occurring when stopping[2] |
| Complications | Mental illness, delirium, Wernicke–Korsakoff syndrome, irregular heartbeat, cirrhosis of the liver, cancer, fetal alcohol spectrum disorder, suicide[3][4][5][6] |
| Duration | Long term[2] |
| Causes | Environmental and genetic factors[4] |
| Risk factors | Stress, anxiety, inexpensive, easy access[4][7] |
| Diagnostic method | Questionnaires, blood tests[4] |
| Treatment | Alcohol detoxification typically with benzodiazepines, counselling, acamprosate, disulfiram, naltrexone[8][9][10] |
| Frequency | 208 million / 4.1% adults (2010)[11][12] |
| Deaths | 3.3 million / 5.9%[13] |
Alcoholism, also known as alcohol use disorder (AUD),[1] is, broadly, any drinking of alcohol that results in mental or physical health problems.[14][2][4] The disorder was previously divided into two types: alcohol abuse and alcohol dependence.[2][15] In a medical context, alcoholism is said to exist when two or more of the following conditions are present: a person drinks large amounts of alcohol over a long time period, has difficulty cutting down, acquiring and drinking alcohol takes up a great deal of time, alcohol is strongly desired, usage results in not fulfilling responsibilities, usage results in social problems, usage results in health problems, usage results in risky situations, withdrawal occurs when stopping, and alcohol tolerance has occurred with use.[2] Alcohol use can affect all parts of the body, but it particularly affects the brain, heart, liver, pancreas and immune system.[4][5] Alcoholism can result in mental illness, delirium tremens, Wernicke–Korsakoff syndrome, irregular heartbeat, an impaired immune response, liver cirrhosis and increased cancer risk.[4][5][16] Drinking during pregnancy can result in fetal alcohol spectrum disorders.[3] Women are generally more sensitive than men to the harmful effects of alcohol, primarily due to their smaller body weight, lower capacity to metabolize alcohol, and higher proportion of body fat.[11]
Environmental factors and genetics are two components associated with alcoholism, with about half the risk attributed to each.[4] Someone with a parent or sibling with alcoholism is three to four times more likely to become an alcoholic themselves.[4] Environmental factors include social, cultural and behavioral influences.[17] High stress levels and anxiety, as well as alcohol's inexpensive cost and easy accessibility, increase the risk.[4][7] People may continue to drink partly to prevent or improve symptoms of withdrawal.[4] After a person stops drinking alcohol, they may experience a low level of withdrawal lasting for months.[4] Medically, alcoholism is considered both a physical and mental illness.[18][19] Questionnaires and certain blood tests may detect possible alcoholism.[4][20] Further information is then collected to confirm the diagnosis.[4]
Prevention of alcoholism may be attempted by regulating and limiting the sale of alcohol, taxing alcohol to increase its cost, and providing inexpensive treatment.[21] Treatment of alcoholism may take several forms.[9] Due to medical problems that can occur during withdrawal, alcohol detoxification should be carefully controlled.[9] One common method involves the use of benzodiazepine medications, such as diazepam.[9] These can be either given while admitted to a health care institution or occasionally while a person remains in the community with close supervision.[9] Mental illness or other addictions may complicate treatment.[22] After detoxification, group therapy or support groups are used to help keep a person from returning to drinking.[8][23] One commonly used form of support is the group Alcoholics Anonymous.[24] The medications acamprosate, disulfiram or naltrexone may also be used to help prevent further drinking.[10]
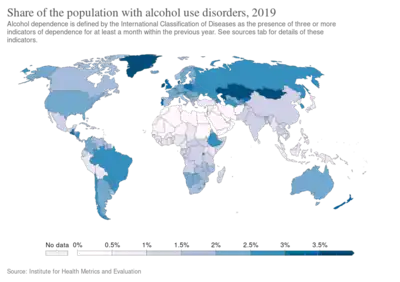
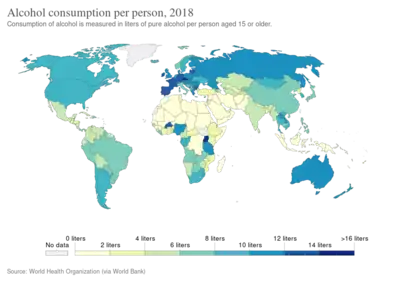
The World Health Organization has estimated that as of 2010, there were 208 million people with alcoholism worldwide (4.1% of the population over 15 years of age).[11][12] As of 2015 in the United States, about 17 million (7%) of adults and 0.7 million (2.8%) of those age 12 to 17 years of age are affected.[13] Alcoholism is most common among males and young adults, and is less common in middle and old age.[4] Geographically, it is least common in Africa (1.1% of the population) and has the highest rates in Eastern Europe (11%).[4] Alcoholism directly resulted in 139,000 deaths in 2013, up from 112,000 deaths in 1990.[25] A total of 3.3 million deaths (5.9% of all deaths) are believed to be due to alcohol.[13] Alcoholism reduces a person's life expectancy by approximately ten years.[26] Many terms, some insulting and others informal, have been used to refer to people affected by alcoholism; the expressions include tippler, drunkard, dipsomaniac and souse.[27] In 1979, the World Health Organization discouraged the use of "alcoholism" due to its inexact meaning, preferring "alcohol dependence syndrome".[28]
Signs and symptoms
The risk of alcohol dependence begins at low levels of drinking and increases directly with both the volume of alcohol consumed and a pattern of drinking larger amounts on an occasion, to the point of intoxication, which is sometimes called "binge drinking".
Long-term misuse
Alcoholism is characterised by an increased tolerance to alcohol – which means that an individual can consume more alcohol – and physical dependence on alcohol, which makes it hard for an individual to control their consumption. The physical dependency caused by alcohol can lead to an affected individual having a very strong urge to drink alcohol. These characteristics play a role in decreasing an alcoholic's ability to stop drinking.[29] Alcoholism can have adverse effects on mental health, contributing to psychiatric disorders and increasing the risk of suicide. A depressed mood is a common symptom of heavy alcohol drinkers.[30][31]
Warning signs
Warning signs of alcoholism include the consumption of increasing amounts of alcohol and frequent intoxication, preoccupation with drinking to the exclusion of other activities, promises to quit drinking and failure to keep those promises, the inability to remember what was said or done while drinking (colloquially known as "blackouts"), personality changes associated with drinking, denial or the making of excuses for drinking, the refusal to admit excessive drinking, dysfunction or other problems at work or school, the loss of interest in personal appearance or hygiene, marital and economic problems, and the complaint of poor health, with loss of appetite, respiratory infections, or increased anxiety.[32]
Physical
Short-term effects
Drinking enough to cause a blood alcohol concentration (BAC) of 0.03–0.12% typically causes an overall improvement in mood and possible euphoria (a "happy" feeling), increased self-confidence and sociability, decreased anxiety, a flushed, red appearance in the face and impaired judgment and fine muscle coordination. A BAC of 0.09% to 0.25% causes lethargy, sedation, balance problems and blurred vision. A BAC of 0.18% to 0.30% causes profound confusion, impaired speech (e.g. slurred speech), staggering, dizziness and vomiting. A BAC from 0.25% to 0.40% causes stupor, unconsciousness, anterograde amnesia, vomiting (death may occur due to inhalation of vomit (pulmonary aspiration) while unconscious) and respiratory depression (potentially life-threatening). A BAC from 0.35% to 0.80% causes a coma (unconsciousness), life-threatening respiratory depression and possibly fatal alcohol poisoning. With all alcoholic beverages, drinking while driving, operating an aircraft or heavy machinery increases the risk of an accident; many countries have penalties for drunk driving.
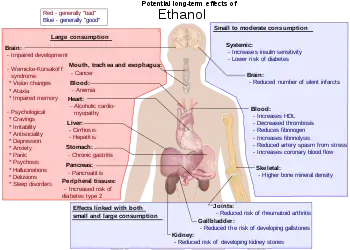
Long-term effects
Having more than one drink a day for women or two drinks for men increases the risk of heart disease, high blood pressure, atrial fibrillation, and stroke.[33] Risk is greater in younger people due to binge drinking, which may result in violence or accidents.[33] About 3.3 million deaths (5.9% of all deaths) are believed to be due to alcohol each year.[13] Alcoholism reduces a person's life expectancy by around ten years[26] and alcohol use is the third leading cause of early death in the United States.[33] No professional medical association recommends that people who are nondrinkers should start drinking.[33][34] Long-term alcohol abuse can cause a number of physical symptoms, including cirrhosis of the liver, pancreatitis, epilepsy, polyneuropathy, alcoholic dementia, heart disease, nutritional deficiencies, peptic ulcers[35] and sexual dysfunction, and can eventually be fatal. Other physical effects include an increased risk of developing cardiovascular disease, malabsorption, alcoholic liver disease, and several cancers. Damage to the central nervous system and peripheral nervous system can occur from sustained alcohol consumption.[36][37] A wide range of immunologic defects can result and there may be a generalized skeletal fragility, in addition to a recognized tendency to accidental injury, resulting a propensity to bone fractures.[38]
Women develop long-term complications of alcohol dependence more rapidly than do men. Additionally, women have a higher mortality rate from alcoholism than men.[39] Examples of long-term complications include brain, heart, and liver damage[40] and an increased risk of breast cancer. Additionally, heavy drinking over time has been found to have a negative effect on reproductive functioning in women. This results in reproductive dysfunction such as anovulation, decreased ovarian mass, problems or irregularity of the menstrual cycle, and early menopause.[39] Alcoholic ketoacidosis can occur in individuals who chronically abuse alcohol and have a recent history of binge drinking.[41][42] The amount of alcohol that can be biologically processed and its effects differ between sexes. Equal dosages of alcohol consumed by men and women generally result in women having higher blood alcohol concentrations (BACs), since women generally have a higher percentage of body fat and therefore a lower volume of distribution for alcohol than men, and because the stomachs of men tend to metabolize alcohol more quickly.[43]
Psychiatric
Long-term misuse of alcohol can cause a wide range of mental health problems. Severe cognitive problems are common; approximately 10 percent of all dementia cases are related to alcohol consumption, making it the second leading cause of dementia.[44] Excessive alcohol use causes damage to brain function, and psychological health can be increasingly affected over time.[45] Social skills are significantly impaired in people suffering from alcoholism due to the neurotoxic effects of alcohol on the brain, especially the prefrontal cortex area of the brain. The social skills that are impaired by alcohol abuse include impairments in perceiving facial emotions, prosody perception problems and theory of mind deficits; the ability to understand humour is also impaired in alcohol abusers.[46] Psychiatric disorders are common in alcoholics, with as many as 25 percent suffering severe psychiatric disturbances. The most prevalent psychiatric symptoms are anxiety and depression disorders. Psychiatric symptoms usually initially worsen during alcohol withdrawal, but typically improve or disappear with continued abstinence.[47] Psychosis, confusion, and organic brain syndrome may be caused by alcohol misuse, which can lead to a misdiagnosis such as schizophrenia.[48] Panic disorder can develop or worsen as a direct result of long-term alcohol misuse.[49][50]
The co-occurrence of major depressive disorder and alcoholism is well documented.[51][52][53] Among those with comorbid occurrences, a distinction is commonly made between depressive episodes that remit with alcohol abstinence ("substance-induced"), and depressive episodes that are primary and do not remit with abstinence ("independent" episodes).[54][55][56] Additional use of other drugs may increase the risk of depression.[57] Psychiatric disorders differ depending on gender. Women who have alcohol-use disorders often have a co-occurring psychiatric diagnosis such as major depression, anxiety, panic disorder, bulimia, post-traumatic stress disorder (PTSD), or borderline personality disorder. Men with alcohol-use disorders more often have a co-occurring diagnosis of narcissistic or antisocial personality disorder, bipolar disorder, schizophrenia, impulse disorders or attention deficit/hyperactivity disorder (ADHD).[58] Women with alcoholism are more likely to experience physical or sexual assault, abuse and domestic violence than women in the general population,[58] which can lead to higher instances of psychiatric disorders and greater dependence on alcohol.
Social effects
Serious social problems arise from alcoholism; these dilemmas are caused by the pathological changes in the brain and the intoxicating effects of alcohol.[44][59] Alcohol abuse is associated with an increased risk of committing criminal offences, including child abuse, domestic violence, rape, burglary and assault.[60] Alcoholism is associated with loss of employment,[61] which can lead to financial problems. Drinking at inappropriate times and behavior caused by reduced judgment can lead to legal consequences, such as criminal charges for drunk driving[62] or public disorder, or civil penalties for tortious behavior, and may lead to a criminal sentence. An alcoholic's behavior and mental impairment while drunk can profoundly affect those surrounding him and lead to isolation from family and friends. This isolation can lead to marital conflict and divorce, or contribute to domestic violence. Alcoholism can also lead to child neglect, with subsequent lasting damage to the emotional development of the alcoholic's children.[63] For this reason, children of alcoholic parents can develop a number of emotional problems. For example, they can become afraid of their parents, because of their unstable mood behaviors. In addition, they can develop considerable amount of shame over their inadequacy to liberate their parents from alcoholism. As a result of this failure, they develop wretched self-images, which can lead to depression.[64]
Alcohol withdrawal
As with similar substances with a sedative-hypnotic mechanism, such as barbiturates and benzodiazepines, withdrawal from alcohol dependence can be fatal if it is not properly managed.[59][65] Alcohol's primary effect is the increase in stimulation of the GABAA receptor, promoting central nervous system depression. With repeated heavy consumption of alcohol, these receptors are desensitized and reduced in number, resulting in tolerance and physical dependence. When alcohol consumption is stopped too abruptly, the person's nervous system suffers from uncontrolled synapse firing. This can result in symptoms that include anxiety, life-threatening seizures, delirium tremens, hallucinations, shakes and possible heart failure.[66][67] Other neurotransmitter systems are also involved, especially dopamine, NMDA and glutamate.[29][68]
Severe acute withdrawal symptoms such as delirium tremens and seizures rarely occur after 1-week post cessation of alcohol. The acute withdrawal phase can be defined as lasting between one and three weeks. In the period of 3–6 weeks following cessation increased anxiety, depression, as well as sleep disturbance, is common;[69] fatigue and tension can persist for up to 5 weeks as part of the post-acute withdrawal syndrome; about a quarter of alcoholics experience anxiety and depression for up to 2 years. These post-acute withdrawal symptoms have also been demonstrated in animal models of alcohol dependence and withdrawal.[70]
A kindling effect also occurs in alcoholics whereby each subsequent withdrawal syndrome is more severe than the previous withdrawal episode; this is due to neuroadaptations which occur as a result of periods of abstinence followed by re-exposure to alcohol. Individuals who have had multiple withdrawal episodes are more likely to develop seizures and experience more severe anxiety during withdrawal from alcohol than alcohol-dependent individuals without a history of past alcohol withdrawal episodes. The kindling effect leads to persistent functional changes in brain neural circuits as well as to gene expression.[71] Kindling also results in the intensification of psychological symptoms of alcohol withdrawal.[69] There are decision tools and questionnaires which help guide physicians in evaluating alcohol withdrawal. For example, the CIWA-Ar objectifies alcohol withdrawal symptoms in order to guide therapy decisions which allows for an efficient interview while at the same time retaining clinical usefulness, validity, and reliability, ensuring proper care for withdrawal patients, who can be in danger of death.[72]
Causes
A complex mixture of genetic and environmental factors influences the risk of the development of alcoholism.[73] Genes that influence the metabolism of alcohol also influence the risk of alcoholism, as can a family history of alcoholism.[74][75] One paper has found that alcohol use at an early age may influence the expression of genes which increase the risk of alcohol dependence.[76] Individuals who have a genetic disposition to alcoholism are also more likely to begin drinking at an earlier age than average.[77] Also, a younger age of onset of drinking is associated with an increased risk of the development of alcoholism,[77] and about 40 percent of alcoholics will drink excessively by their late adolescence. It is not entirely clear whether this association is causal, and some researchers have been known to disagree with this view.[78]
Severe childhood trauma is also associated with a general increase in the risk of drug dependency.[73] Lack of peer and family support is associated with an increased risk of alcoholism developing.[73] Genetics and adolescence are associated with an increased sensitivity to the neurotoxic effects of chronic alcohol abuse. Cortical degeneration due to the neurotoxic effects increases impulsive behaviour, which may contribute to the development, persistence and severity of alcohol use disorders. There is evidence that with abstinence, there is a reversal of at least some of the alcohol induced central nervous system damage.[79] The use of cannabis was associated with later problems with alcohol use.[80] Alcohol use was associated with an increased probability of later use of tobacco and illegal drugs such as cannabis.[81]
Availability
Alcohol is the most available, widely consumed, and widely abused recreational drug. Beer alone is the world's most widely consumed[82] alcoholic beverage; it is the third-most popular drink overall, after water and tea.[83] It is thought by some to be the oldest fermented beverage.[84][85][86][87]
Gender difference
Based on combined data from SAMHSA's 2004–2005 National Surveys on Drug Use & Health, the rate of past-year alcohol dependence or abuse among persons aged 12 or older varied by level of alcohol use: 44.7% of past month heavy drinkers, 18.5% binge drinkers, 3.8% past month non-binge drinkers, and 1.3% of those who did not drink alcohol in the past month met the criteria for alcohol dependence or abuse in the past year. Males had higher rates than females for all measures of drinking in the past month: any alcohol use (57.5% vs. 45%), binge drinking (30.8% vs. 15.1%), and heavy alcohol use (10.5% vs. 3.3%), and males were twice as likely as females to have met the criteria for alcohol dependence or abuse in the past year (10.5% vs. 5.1%).[88]
Genetic variation
There are genetic variations that affect the risk for alcoholism.[74][73][89][90] Some of these variations are more common in individuals with ancestry from certain areas, for example Africa, East Asia, the Middle East and Europe. The variants with strongest effect are in genes that encode the main enzymes of alcohol metabolism, ADH1B and ALDH2.[74][89][90] These genetic factors influence the rate at which alcohol and its initial metabolic product, acetaldehyde, are metabolized.[74] They are found at different frequencies in people from different parts of the world.[91][74][92] The alcohol dehydrogenase allele ADH1B*2 causes a more rapid metabolism of alcohol to acetaldehyde, and reduces risk for alcoholism;[74] it is most common in individuals from East Asia and the Middle East. The alcohol dehydrogenase allele ADH1B*3 causes a more rapid metabolism of alcohol. The allele ADH1B*3 is only found in some individuals of African descent and certain Native American tribes. African Americans and Native Americans with this allele have a reduced risk of developing alcoholism.[74][92][93] Native Americans, however, have a significantly higher rate of alcoholism than average; risk factors such as cultural environmental effects e.g. trauma have been proposed to explain the higher rates.[94][95] The aldehyde dehydrogenase allele ALDH2*2 greatly reduces the rate at which acetaldehyde, the initial product of alcohol metabolism, is removed by conversion to acetate; it greatly reduces the risk for alcoholism.[74][91]
A genome-wide association study of more than 100,000 human individuals identified variants of the gene KLB, which encodes the transmembrane protein β-Klotho, as highly associated with alcohol consumption. The protein β-Klotho is an essential element in cell surface receptors for hormones involved in modulation of appetites for simple sugars and alcohol.[96] A GWAS has found differences in the genetics of alcohol consumption and alcohol dependence, although the two are to some degree related.[89]
Diagnosis
Definition

Misuse, problem use, abuse, and heavy use of alcohol refer to improper use of alcohol, which may cause physical, social, or moral harm to the drinker.[97] The Dietary Guidelines for Americans defines "moderate use" as no more than two alcoholic beverages a day for men and no more than one alcoholic beverage a day for women.[98] Some drinkers may drink more than 600 ml of alcohol per day during a heavy drinking period.[99] The National Institute on Alcohol Abuse and Alcoholism (NIAAA) defines binge drinking as the amount of alcohol leading to a blood alcohol content (BAC) of 0.08, which, for most adults, would be reached by consuming five drinks for men or four for women over a two-hour period. According to the NIAAA, men may be at risk for alcohol-related problems if their alcohol consumption exceeds 14 standard drinks per week or 4 drinks per day, and women may be at risk if they have more than 7 standard drinks per week or 3 drinks per day. It defines a standard drink as one 12-ounce bottle of beer, one 5-ounce glass of wine, or 1.5 ounces of distilled spirits.[100] Despite this risk, a 2014 report in the National Survey on Drug Use and Health found that only 10% of either "heavy drinkers" or "binge drinkers" defined according to the above criteria also met the criteria for alcohol dependence, while only 1.3% of non-binge drinkers met the criteria. An inference drawn from this study is that evidence-based policy strategies and clinical preventive services may effectively reduce binge drinking without requiring addiction treatment in most cases.[101]
Alcoholism
The term alcoholism is commonly used amongst laypeople, but the word is poorly defined. The WHO calls alcoholism "a term of long-standing use and variable meaning", and use of the term was disfavored by a 1979 WHO expert committee. The Big Book (from Alcoholics Anonymous) states that once a person is an alcoholic, they are always an alcoholic (but others note that many do recover), but does not define what is meant by the term alcoholic in this context. In 1960, Bill W., co-founder of Alcoholics Anonymous (AA), said:
- We have never called alcoholism a disease because, technically speaking, it is not a disease entity. For example, there is no such thing as heart disease. Instead there are many separate heart ailments, or combinations of them. It is something like that with alcoholism. We did not wish to get in wrong with the medical profession by pronouncing alcoholism a disease entity. We always called it an illness, or a malady – a far safer term for us to use.[102]
In professional and research contexts, the term "alcoholism" sometimes encompasses both alcohol abuse and alcohol dependence,[103] and sometimes is considered equivalent to alcohol dependence. Talbot (1989) observes that alcoholism in the classical disease model follows a progressive course: if a person continues to drink, their condition will worsen. This will lead to harmful consequences in their life, physically, mentally, emotionally and socially.[104] Johnson (1980) explores the emotional progression of the addict's response to alcohol. He looks at this in four phases. The first two are considered "normal" drinking and the last two are viewed as "typical" alcoholic drinking.[104] Johnson's four phases consist of:
- Learning the mood swing. A person is introduced to alcohol (in some cultures this can happen at a relatively young age), and the person enjoys the happy feeling it produces. At this stage, there is no emotional cost.
- Seeking the mood swing. A person will drink to regain that feeling of euphoria experienced in phase 1; the drinking will increase as more intoxication is required to achieve the same effect. Again at this stage, there are no significant consequences.
- At the third stage there are physical and social consequences, i.e., hangovers, family problems, work problems, etc. A person will continue to drink excessively, disregarding the problems.
- The fourth stage can be detrimental, as Johnson cites it as a risk for premature death. As a person now drinks to feel normal, they block out the feelings of overwhelming guilt, remorse, anxiety, and shame they experience when sober.[104]
Milam & Ketcham's physical deterioration stages
Other theorists such as Milam & Ketcham (1983) focus on the physical deterioration that alcohol consumption causes. They describe the process in three stages:
- Adaptive stage – The person will not experience any negative symptoms, and they believe they have the capacity for drinking alcohol without problems. Physiological changes are happening with the increase in tolerance, but this will not be noticeable to the drinker or others.
- Dependent stage – At this stage, symptoms build up gradually. Hangover symptoms from excessive drinking may be confused with withdrawal symptoms. Many addicts will maintain their drinking to avoid withdrawal sickness, drinking small amounts frequently. They will try to hide their drinking problem from others and will avoid gross intoxication.
- Deterioration stage – Various organs are damaged due to long-term drinking. Medical treatment in a rehabilitation center will be required; otherwise, the pathological changes will cause death.
DSM and ICD
In psychology and psychiatry, the DSM is the most common global standard, while in medicine, the standard is ICD. The terms they recommend are similar but not identical.
| Organization | Preferred term(s) | Definition |
|---|---|---|
| APA's DSM-IV | "alcohol abuse" and "alcohol dependence" |
|
| WHO's ICD-10 | "alcohol harmful use" and "alcohol dependence syndrome" | Definitions are similar to that of the DSM-IV. The World Health Organization uses the term "alcohol dependence syndrome" rather than alcoholism.[28] The concept of "harmful use" (as opposed to "abuse") was introduced in 1992's ICD-10 to minimize underreporting of damage in the absence of dependence.[106] The term "alcoholism" was removed from ICD between ICD-8/ICDA-8 and ICD-9.[109] |
The DSM-IV diagnosis of alcohol dependence represents one approach to the definition of alcoholism. In part, this is to assist in the development of research protocols in which findings can be compared to one another. According to the DSM-IV, an alcohol dependence diagnosis is: "maladaptive alcohol use with clinically significant impairment as manifested by at least three of the following within any one-year period: tolerance; withdrawal; taken in greater amounts or over longer time course than intended; desire or unsuccessful attempts to cut down or control use; great deal of time spent obtaining, using, or recovering from use; social, occupational, or recreational activities given up or reduced; continued use despite knowledge of physical or psychological sequelae."[110] Despite the imprecision inherent in the term, there have been attempts to define how the word alcoholism should be interpreted when encountered. In 1992, it was defined by the National Council on Alcoholism and Drug Dependence (NCADD) and ASAM as "a primary, chronic disease characterized by impaired control over drinking, preoccupation with the drug alcohol, use of alcohol despite adverse consequences, and distortions in thinking."[111] MeSH has had an entry for "alcoholism" since 1999, and references the 1992 definition.[112]
AA describes alcoholism as an illness that involves a physical allergy[113]: 28 (where "allergy" has a different meaning than that used in modern medicine.[114]) and a mental obsession.[113]: 23 [115] The doctor and addiction specialist Dr. William D. Silkworth M.D. writes on behalf of AA that "Alcoholics suffer from a "(physical) craving beyond mental control".[113]: xxvi A 1960 study by E. Morton Jellinek is considered the foundation of the modern disease theory of alcoholism.[116] Jellinek's definition restricted the use of the word alcoholism to those showing a particular natural history. The modern medical definition of alcoholism has been revised numerous times since then. The American Medical Association uses the word alcoholism to refer to a particular chronic primary disease.[117]
Social barriers
Attitudes and social stereotypes can create barriers to the detection and treatment of alcohol abuse. This is more of a barrier for women than men. Fear of stigmatization may lead women to deny that they are suffering from a medical condition, to hide their drinking, and to drink alone. This pattern, in turn, leads family, physicians, and others to be less likely to suspect that a woman they know is an alcoholic.[39] In contrast, reduced fear of stigma may lead men to admit that they are suffering from a medical condition, to display their drinking publicly, and to drink in groups. This pattern, in turn, leads family, physicians, and others to be more likely to suspect that a man they know is an alcoholic.[58]
Screening
Screening is recommended among those over the age of 18.[118] Several tools may be used to detect a loss of control of alcohol use. These tools are mostly self-reports in questionnaire form. Another common theme is a score or tally that sums up the general severity of alcohol use.[119]
The CAGE questionnaire, named for its four questions, is one such example that may be used to screen patients quickly in a doctor's office.
Two "yes" responses indicate that the respondent should be investigated further.
The questionnaire asks the following questions:
- The CAGE questionnaire has demonstrated a high effectiveness in detecting alcohol-related problems; however, it has limitations in people with less severe alcohol-related problems, white women and college students.[122]
Other tests are sometimes used for the detection of alcohol dependence, such as the Alcohol Dependence Data Questionnaire, which is a more sensitive diagnostic test than the CAGE questionnaire. It helps distinguish a diagnosis of alcohol dependence from one of heavy alcohol use.[123] The Michigan Alcohol Screening Test (MAST) is a screening tool for alcoholism widely used by courts to determine the appropriate sentencing for people convicted of alcohol-related offenses,[124] driving under the influence being the most common. The Alcohol Use Disorders Identification Test (AUDIT), a screening questionnaire developed by the World Health Organization, is unique in that it has been validated in six countries and is used internationally. Like the CAGE questionnaire, it uses a simple set of questions – a high score earning a deeper investigation.[125] The Paddington Alcohol Test (PAT) was designed to screen for alcohol-related problems amongst those attending Accident and Emergency departments. It concords well with the AUDIT questionnaire but is administered in a fifth of the time.[126] Certain blood tests may also indicate possible alcoholism.[4]
Urine and blood tests
There are reliable tests for the actual use of alcohol, one common test being that of blood alcohol content (BAC).[127] These tests do not differentiate alcoholics from non-alcoholics; however, long-term heavy drinking does have a few recognizable effects on the body, including:[128]
- Macrocytosis (enlarged MCV)
- Elevated GGT
- Moderate elevation of AST and ALT and an AST: ALT ratio of 2:1
- High carbohydrate deficient transferrin (CDT)
With regard to alcoholism, BAC is useful to judge alcohol tolerance, which in turn is a sign of alcoholism.[4] Electrolyte and acid-base abnormalities including hypokalemia, hypomagnesemia, hyponatremia, hyperuricemia, metabolic acidosis, and respiratory alkalosis are common in alcoholics.[5]
However, none of these blood tests for biological markers is as sensitive as screening questionnaires.
Prevention
The World Health Organization, the European Union and other regional bodies, national governments and parliaments have formed alcohol policies in order to reduce the harm of alcoholism.[129][130] Targeting adolescents and young adults is regarded as an important step to reduce the harm of alcohol abuse. Increasing the age at which licit drugs of abuse such as alcohol can be purchased, the banning or restricting advertising of alcohol has been recommended as additional ways of reducing the harm of alcohol dependence and abuse. Credible, evidence based educational campaigns in the mass media about the consequences of alcohol abuse have been recommended. Guidelines for parents to prevent alcohol abuse amongst adolescents, and for helping young people with mental health problems have also been suggested.[131]
Management
Treatments are varied because there are multiple perspectives of alcoholism. Those who approach alcoholism as a medical condition or disease recommend differing treatments from, for instance, those who approach the condition as one of social choice. Most treatments focus on helping people discontinue their alcohol intake, followed up with life training and/or social support to help them resist a return to alcohol use. Since alcoholism involves multiple factors which encourage a person to continue drinking, they must all be addressed to successfully prevent a relapse. An example of this kind of treatment is detoxification followed by a combination of supportive therapy, attendance at self-help groups, and ongoing development of coping mechanisms. The treatment community for alcoholism typically supports an abstinence-based zero tolerance approach; however, some prefer a harm-reduction approach.[132]
Detoxification
Alcohol detoxification or 'detox' for alcoholics is an abrupt stop of alcohol drinking coupled with the substitution of drugs, such as benzodiazepines, that have similar effects to prevent alcohol withdrawal. Individuals who are only at risk of mild to moderate withdrawal symptoms can be detoxified as outpatients. Individuals at risk of a severe withdrawal syndrome as well as those who have significant or acute comorbid conditions are generally treated as inpatients. Detoxification does not actually treat alcoholism, and it is necessary to follow up detoxification with an appropriate treatment program for alcohol dependence or abuse to reduce the risk of relapse.[9] Some symptoms of alcohol withdrawal such as depressed mood and anxiety typically take weeks or months to abate while other symptoms persist longer due to persisting neuroadaptations.[69] Alcoholism has serious adverse effects on brain function; on average it takes one year of abstinence to recover from the cognitive deficits incurred by chronic alcohol abuse.[133]
Psychological

Various forms of group therapy or psychotherapy can be used to deal with underlying psychological issues that are related to alcohol addiction, as well as provide relapse prevention skills. The mutual-help group-counseling approach is one of the most common ways of helping alcoholics maintain sobriety.[8] Alcoholics Anonymous was one of the first organizations formed to provide mutual, nonprofessional counseling, and it is still the largest. Others include LifeRing Secular Recovery, SMART Recovery, Women for Sobriety, and Secular Organizations for Sobriety.[134] Alcoholics Anonymous and twelve-step programs appear more effective than cognitive behavioral therapy or abstinence.[135]
Moderate drinking
Rationing and moderation programs such as Moderation Management and DrinkWise do not mandate complete abstinence. While most alcoholics are unable to limit their drinking in this way, some return to moderate drinking. A 2002 US study by the National Institute on Alcohol Abuse and Alcoholism (NIAAA) showed that 17.7 percent of individuals diagnosed as alcohol dependent more than one year prior returned to low-risk drinking. This group, however, showed fewer initial symptoms of dependency.[136]
A follow-up study, using the same subjects that were judged to be in remission in 2001–2002, examined the rates of return to problem drinking in 2004–2005. The study found abstinence from alcohol was the most stable form of remission for recovering alcoholics.[137] There was also a 1973 study showing chronic alcoholics drinking moderately again,[138] but a 1982 follow-up showed that 95% of subjects were not able to moderately drink over the long term.[139][140] Another study was a long-term (60 year) follow-up of two groups of alcoholic men which concluded that "return to controlled drinking rarely persisted for much more than a decade without relapse or evolution into abstinence."[141] Internet based measures appear to be useful at least in the short term.[142]
Medications
In the United States there are four approved medications for alcoholism: acamprosate, two methods of using naltrexone and disulfiram.[143]
- Acamprosate may stabilise the brain chemistry that is altered due to alcohol dependence via antagonising the actions of glutamate, a neurotransmitter which is hyperactive in the post-withdrawal phase.[144] By reducing excessive NMDA activity which occurs at the onset of alcohol withdrawal, acamprosate can reduce or prevent alcohol withdrawal related neurotoxicity.[145] Acamprosate reduces the risk of relapse amongst alcohol-dependent persons.[146][147]
- Naltrexone is a competitive antagonist for opioid receptors, effectively blocking the effects of endorphins and opioids. Naltrexone is used to decrease cravings for alcohol and encourage abstinence. Alcohol causes the body to release endorphins, which in turn release dopamine and activate the reward pathways; hence in the body reduces the pleasurable effects from consuming alcohol.[148] Evidence supports a reduced risk of relapse among alcohol-dependent persons and a decrease in excessive drinking.[147] Nalmefene also appears effective and works in a similar manner.[147]
- The Sinclair method is another approach to using naltrexone or other opioid antagonists to treat alcoholism by having the person take the medication about an hour before they drink alcohol and only then.[149][150] The medication blocks the positive reinforcement effects of ethanol and hypothetically allows the person to stop drinking or drink less.[150]
- Disulfiram prevents the elimination of acetaldehyde, a chemical the body produces when breaking down ethanol. Acetaldehyde itself is the cause of many hangover symptoms from alcohol use. The overall effect is discomfort when alcohol is ingested: an extremely fast-acting and long-lasting, uncomfortable hangover.
Several other drugs are also used and many are under investigation.
- Benzodiazepines, while useful in the management of acute alcohol withdrawal, if used long-term can cause a worse outcome in alcoholism. Alcoholics on chronic benzodiazepines have a lower rate of achieving abstinence from alcohol than those not taking benzodiazepines. This class of drugs is commonly prescribed to alcoholics for insomnia or anxiety management.[151] Initiating prescriptions of benzodiazepines or sedative-hypnotics in individuals in recovery has a high rate of relapse with one author reporting more than a quarter of people relapsed after being prescribed sedative-hypnotics. Those who are long-term users of benzodiazepines should not be withdrawn rapidly, as severe anxiety and panic may develop, which are known risk factors for relapse into alcohol abuse. Taper regimes of 6–12 months have been found to be the most successful, with reduced intensity of withdrawal.[152][153]
- Calcium carbimide works in the same way as disulfiram; it has an advantage in that the occasional adverse effects of disulfiram, hepatotoxicity and drowsiness, do not occur with calcium carbimide.[154]
- Ondansetron and topiramate are supported by tentative evidence in people with certain genetics.[155][156] Evidence for ondansetron is more in those who have just begun having problems with alcohol.[155]
Evidence does not support the use of selective serotonin reuptake inhibitors (SSRIs), tricyclic antidepressants (TCAs), antipsychotics, or gabapentin.[147]
Dual addictions and dependences
Alcoholics may also require treatment for other psychotropic drug addictions and drug dependences. The most common dual dependence syndrome with alcohol dependence is benzodiazepine dependence, with studies showing 10–20 percent of alcohol-dependent individuals had problems of dependence and/or misuse problems of benzodiazepine drugs such as diazepam or clonazepam. These drugs are, like alcohol, depressants. Benzodiazepines may be used legally, if they are prescribed by doctors for anxiety problems or other mood disorders, or they may be purchased as illegal drugs. Benzodiazepine use increases cravings for alcohol and the volume of alcohol consumed by problem drinkers.[157] Benzodiazepine dependency requires careful reduction in dosage to avoid benzodiazepine withdrawal syndrome and other health consequences. Dependence on other sedative-hypnotics such as zolpidem and zopiclone as well as opiates and illegal drugs is common in alcoholics. Alcohol itself is a sedative-hypnotic and is cross-tolerant with other sedative-hypnotics such as barbiturates, benzodiazepines and nonbenzodiazepines. Dependence upon and withdrawal from sedative-hypnotics can be medically severe and, as with alcohol withdrawal, there is a risk of psychosis or seizures if not properly managed.[158]
Prognosis

Alcoholism often reduces a person's life expectancy by around ten years.[26] The most common cause of death in alcoholics is from cardiovascular complications.[159] There is a high rate of suicide in chronic alcoholics, which increases the longer a person drinks. Approximately 3–15 percent of alcoholics commit suicide,[160] and research has found that over 50 percent of all suicides are associated with alcohol or drug dependence. This is believed to be due to alcohol causing physiological distortion of brain chemistry, as well as social isolation. Suicide is also very common in adolescent alcohol abusers, with 25 percent of suicides in adolescents being related to alcohol abuse.[161] Among those with alcohol dependence after one year, some met the criteria for low-risk drinking, even though only 25.5 percent of the group received any treatment, with the breakdown as follows: 25 percent were found to be still dependent, 27.3 percent were in partial remission (some symptoms persist), 11.8 percent asymptomatic drinkers (consumption increases chances of relapse) and 35.9 percent were fully recovered – made up of 17.7 percent low-risk drinkers plus 18.2 percent abstainers.[162] In contrast, however, the results of a long-term (60-year) follow-up of two groups of alcoholic men indicated that "return to controlled drinking rarely persisted for much more than a decade without relapse or evolution into abstinence."[163] There was also "return-to-controlled drinking, as reported in short-term studies, is often a mirage."
Epidemiology
The World Health Organization estimates that as of 2010 there are 208 million people with alcoholism worldwide (4.1% of the population over 15 years of age).[11][12] Substance use disorders are a major public health problem facing many countries. "The most common substance of abuse/dependence in patients presenting for treatment is alcohol."[132] In the United Kingdom, the number of 'dependent drinkers' was calculated as over 2.8 million in 2001.[164] About 12% of American adults have had an alcohol dependence problem at some time in their life.[165] In the United States and Western Europe, 10 to 20 percent of men and 5 to 10 percent of women at some point in their lives will meet criteria for alcoholism.[166] Estonia had the highest death rate from alcohol in Europe in 2015 at 8.8 per 100,000 population.[167] In the United States, 30% of people admitted to hospital have a problem related to alcohol.[168]
Within the medical and scientific communities, there is a broad consensus regarding alcoholism as a disease state. For example, the American Medical Association considers alcohol a drug and states that "drug addiction is a chronic, relapsing brain disease characterized by compulsive drug seeking and use despite often devastating consequences. It results from a complex interplay of biological vulnerability, environmental exposure, and developmental factors (e.g., stage of brain maturity)."[117] Alcoholism has a higher prevalence among men, though, in recent decades, the proportion of female alcoholics has increased.[40] Current evidence indicates that in both men and women, alcoholism is 50–60 percent genetically determined, leaving 40–50 percent for environmental influences.[169] Most alcoholics develop alcoholism during adolescence or young adulthood.[73] 31 percent of college students show signs of alcohol abuse, while six percent are dependent on alcohol. Under the DSM's new definition of alcoholics, that means about 37 percent of college students may meet the criteria.[170]
History

Historically the name "dipsomania" was coined by German physician C.W. Hufeland in 1819 before it was superseded by "alcoholism".[171][172] That term now has a more specific meaning.[173] The term "alcoholism" was first used in 1849 by the Swedish physician Magnus Huss to describe the systematic adverse effects of alcohol.[174] Alcohol has a long history of use and misuse throughout recorded history. Biblical, Egyptian and Babylonian sources record the history of abuse and dependence on alcohol. In some ancient cultures alcohol was worshiped and in others, its abuse was condemned. Excessive alcohol misuse and drunkenness were recognized as causing social problems even thousands of years ago. However, the defining of habitual drunkenness as it was then known as and its adverse consequences were not well established medically until the 18th century. In 1647 a Greek monk named Agapios was the first to document that chronic alcohol misuse was associated with toxicity to the nervous system and body which resulted in a range of medical disorders such as seizures, paralysis, and internal bleeding. In 1920 the effects of alcohol abuse and chronic drunkenness boosted membership of the temperance movement and led to the prohibition of alcohol in the United States, a nationwide constitutional ban on the production, importation, transportation, and sale of alcoholic beverages that remained in place until 1933; this policy resulted in the decline of death rates from cirrhosis and alcoholism.[175] In 2005 alcohol dependence and abuse was estimated to cost the US economy approximately 220 billion dollars per year, more than cancer and obesity.[176]
Society and culture
The various health problems associated with long-term alcohol consumption are generally perceived as detrimental to society, for example, money due to lost labor-hours, medical costs due to injuries due to drunkenness and organ damage from long-term use, and secondary treatment costs, such as the costs of rehabilitation facilities and detoxification centers. Alcohol use is a major contributing factor for head injuries, motor vehicle injuriess (27%), interpersonal violence (18%), suicides (18%), and epilepsy (13%).[177] Beyond the financial costs that alcohol consumption imposes, there are also significant social costs to both the alcoholic and their family and friends.[59] For instance, alcohol consumption by a pregnant woman can lead to an incurable and damaging condition known as fetal alcohol syndrome, which often results in cognitive deficits, mental health problems, an inability to live independently and an increased risk of criminal behaviour, all of which can cause emotional stress for parents and caregivers.[178][179] Estimates of the economic costs of alcohol abuse, collected by the World Health Organization, vary from one to six percent of a country's GDP.[180] One Australian estimate pegged alcohol's social costs at 24% of all drug abuse costs; a similar Canadian study concluded alcohol's share was 41%.[181] One study quantified the cost to the UK of all forms of alcohol misuse in 2001 as £18.5–20 billion.[164][182] All economic costs in the United States in 2006 have been estimated at $223.5 billion.[183]
The idea of hitting rock bottom refers to an experience of stress that is blamed on alcohol misuse. There is no single definition for this idea, and people may identify their own lowest points in terms of lost jobs, lost relationships, health problems, legal problems, or other consequences of alcohol misuse.[184] The concept is promoted by 12-step recovery groups and researchers using the transtheoretical model of motivation for behavior change.[184] The first use of this slang phrase in the formal medical literature appeared in a 1965 review in the British Medical Journal,[184] which said that some men refused treatment until they "hit rock bottom", but that treatment was generally more successful for "the alcohol addict who has friends and family to support him" than for impoverished and homeless addicts.[185]
Stereotypes of alcoholics are often found in fiction and popular culture. The "town drunk" is a stock character in Western popular culture. Stereotypes of drunkenness may be based on racism or xenophobia, as in the fictional depiction of the Irish as heavy drinkers.[186] Studies by social psychologists Stivers and Greeley attempt to document the perceived prevalence of high alcohol consumption amongst the Irish in America.[187] Alcohol consumption is relatively similar between many European cultures, the United States, and Australia. In Asian countries that have a high gross domestic product, there is heightened drinking compared to other Asian countries, but it is nowhere near as high as it is in other countries like the United States. It is also inversely seen, with countries that have very low gross domestic product showing high alcohol consumption.[188] In a study done on Korean immigrants in Canada, they reported alcohol was even an integral part of their meal, and is the only time solo drinking should occur. They also believe alcohol is necessary at any social event as it helps conversations start.[189]
Caucasians have a much lower abstinence rate (11.8%) and much higher tolerance to symptoms (3.4±2.45 drinks) of alcohol than Chinese (33.4% and 2.2±1.78 drinks respectively). Also, the more acculturation there is between cultures, the more influenced the culture is to adopt Caucasians drinking practices.[190] Peyote, a psychoactive agent, has even shown promise in treating alcoholism. Alcohol had actually replaced peyote as Native Americans’ psychoactive agent of choice in rituals when peyote was outlawed.[191]
Research
Topiramate
Topiramate, a derivative of the naturally occurring sugar monosaccharide D-fructose, has been found effective in helping alcoholics quit or cut back on the amount they drink. Evidence suggests that topiramate antagonizes excitatory glutamate receptors, inhibits dopamine release, and enhances inhibitory gamma-aminobutyric acid function. A 2008 review of the effectiveness of topiramate concluded that the results of published trials are promising, however, as of 2008, data was insufficient to support using topiramate in conjunction with brief weekly compliance counseling as a first-line agent for alcohol dependence.[192] A 2010 review found that topiramate may be superior to existing alcohol pharmacotherapeutic options. Topiramate effectively reduces craving and alcohol withdrawal severity as well as improving quality-of-life-ratings.[193]
Baclofen
Baclofen, a GABAB receptor agonist, is under study for the treatment of alcoholism.[194] A 2019 systematic review concluded that there is insufficient evidence to draw any conclusions about the safety and efficacy because the evidence is of low quality and insufficient.[195] In 2018 baclofen received a Marketing Authorization for use in alcoholism treatment from the French drug agency ANSM if all other treatments are not effective.[196]
Ondansetron
Ondansetron, a 5HT3 antagonist, appears to have promise as a treatment.[197]
LSD
According to a retrospective analysis of six studies from the 1960s and 1970s LSD-assisted psychotherapy has potential as a treatment for alcoholism.[198][199] Bill Wilson, the founder of Alcoholics Anonymous, believed LSD might help alcoholics achieve sobriety.[200]
See also
- Addictive personality
- Alcohol-related traffic crashes in the United States
- Alcoholism in family systems
- Collaborative Study On The Genetics of Alcoholism
- CRAFFT Screening Test
- Disulfiram-like drug
- High-functioning alcoholic
- List of countries by alcohol consumption
References
- 1 2 "Alcoholism MeSH Descriptor Data 2020". meshb.nlm.nih.gov. Archived from the original on 23 June 2020. Retrieved 9 May 2020.
- 1 2 3 4 5 "Alcohol Use Disorder: A Comparison Between DSM–IV and DSM–5". November 2013. Archived from the original on 18 May 2015. Retrieved 9 May 2015.
- 1 2 "Fetal Alcohol Exposure". 14 September 2011. Archived from the original on 4 April 2015. Retrieved 9 May 2015.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 Association, American Psychiatric (2013). Diagnostic and statistical manual of mental disorders : DSM-5 (5 ed.). Washington, DC: American Psychiatric Association. pp. 490–97. ISBN 978-0-89042-554-1.
- 1 2 3 4 "Alcohol's Effects on the Body". 14 September 2011. Archived from the original on 3 June 2015. Retrieved 9 May 2015.
- ↑ Borges, G; Bagge, CL; Cherpitel, CJ; Conner, KR; Orozco, R; Rossow, I (April 2017). "A meta-analysis of acute use of alcohol and the risk of suicide attempt". Psychological Medicine. 47 (5): 949–957. doi:10.1017/S0033291716002841. PMC 5340592. PMID 27928972.
- 1 2 Moonat, S; Pandey, SC (2012). "Stress, epigenetics, and alcoholism". Alcohol Research : Current Reviews. 34 (4): 495–505. PMC 3860391. PMID 23584115.
- 1 2 3 Morgan-Lopez, AA; Fals-Stewart, W (May 2006). "Analytic complexities associated with group therapy in substance abuse treatment research: problems, recommendations, and future directions". Exp Clin Psychopharmacol. 14 (2): 265–73. doi:10.1037/1064-1297.14.2.265. PMC 4631029. PMID 16756430.
- 1 2 3 4 5 6 Blondell, RD (February 2005). "Ambulatory detoxification of patients with alcohol dependence". Am Fam Physician. 71 (3): 495–502. PMID 15712624.
- 1 2 Testino, G; Leone, S; Borro, P (December 2014). "Treatment of alcohol dependence: recent progress and reduction of consumption". Minerva Medica. 105 (6): 447–66. PMID 25392958.
- 1 2 3 4 Global status report on alcohol and health 2014 (PDF). World Health Organization. 2014. pp. 8, 51. ISBN 978-92-4-069276-3. Archived (PDF) from the original on 13 April 2015.
- 1 2 3 "Global Population Estimates by Age, 1950–2050". 30 January 2014. Archived from the original on 10 May 2015. Retrieved 10 May 2015.
- 1 2 3 4 "Alcohol Facts and Statistics". Archived from the original on 18 May 2015. Retrieved 9 May 2015.
- ↑ Littrell, Jill (2014). Understanding and Treating Alcoholism Volume I: An Empirically Based Clinician's Handbook for the Treatment of Alcoholism: Volume Ii: Biological, Psychological, and Social Aspects of Alcohol Consumption and Abuse. Hoboken: Taylor and Francis. p. 55. ISBN 978-1-317-78314-5. Archived from the original on 20 July 2017.
The World Health Organization defines alcoholism as any drinking which results in problems
- ↑ Hasin, Deborah (December 2003). "Classification of Alcohol Use Disorders". Alcohol Research & Health : The Journal of the National Institute on Alcohol Abuse and Alcoholism. 27 (1): 5–17. PMC 6676702. PMID 15301396. Archived from the original on 18 March 2015. Retrieved 28 February 2015.
- ↑ Romeo, Javier; Wärnberg, Julia; Nova, Esther; Díaz, Ligia E.; Gómez-Martinez, Sonia; Marcos, Ascensión (October 2007). "Moderate alcohol consumption and the immune system: a review". The British Journal of Nutrition. 98 Suppl 1: S111–115. doi:10.1017/S0007114507838049. ISSN 0007-1145. PMID 17922947.
- ↑ Agarwal-Kozlowski, K; Agarwal, DP (April 2000). "[Genetic predisposition for alcoholism]". Ther Umsch. 57 (4): 179–84. doi:10.1024/0040-5930.57.4.179. PMID 10804873.
- ↑ Mersy, DJ (1 April 2003). "Recognition of alcohol and substance abuse". American Family Physician. 67 (7): 1529–32. PMID 12722853.
- ↑ "Health and Ethics Policies of the AMA House of Delegates" (PDF). June 2008. p. 33. Archived (PDF) from the original on 20 March 2015. Retrieved 10 May 2015.
H-30.997 Dual Disease Classification of Alcoholism: The AMA reaffirms its policy endorsing the dual classification of alcoholism under both the psychiatric and medical sections of the International Classification of Diseases. (Res. 22, I-79; Reaffirmed: CLRPD Rep. B, I-89; Reaffirmed: CLRPD Rep. B, I-90; Reaffirmed by CSA Rep. 14, A-97; Reaffirmed: CSAPH Rep. 3, A-07)
- ↑ Higgins-Biddle, John C.; Babor, Thomas F. (2018). "A Review of the Alcohol Use Disorders Identification Test (AUDIT), AUDIT-C, and USAUDIT for Screening in the United States: Past Issues and Future Directions". The American Journal of Drug and Alcohol Abuse. 44 (6): 578–586. doi:10.1080/00952990.2018.1456545. ISSN 0095-2990. PMC 6217805. PMID 29723083.
- ↑ World Health Organization (January 2015). "Alcohol". Archived from the original on 23 May 2015. Retrieved 10 May 2015.
- ↑ DeVido, JJ; Weiss, RD (December 2012). "Treatment of the depressed alcoholic patient". Current Psychiatry Reports. 14 (6): 610–08. doi:10.1007/s11920-012-0314-7. PMC 3712746. PMID 22907336.
- ↑ Albanese, AP (November 2012). "Management of alcohol abuse". Clinics in Liver Disease. 16 (4): 737–62. doi:10.1016/j.cld.2012.08.006. PMID 23101980.
- ↑ Tusa, AL; Burgholzer, JA (2013). "Came to believe: spirituality as a mechanism of change in alcoholics anonymous: a review of the literature from 1992 to 2012". Journal of Addictions Nursing. 24 (4): 237–46. doi:10.1097/jan.0000000000000003. PMID 24335771.
- ↑ GBD 2013 Mortality and Causes of Death, Collaborators (17 December 2014). "Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013". Lancet. 385 (9963): 117–71. doi:10.1016/S0140-6736(14)61682-2. PMC 4340604. PMID 25530442.
- 1 2 3 Schuckit, MA (27 November 2014). "Recognition and management of withdrawal delirium (delirium tremens)". The New England Journal of Medicine. 371 (22): 2109–13. doi:10.1056/NEJMra1407298. PMID 25427113. Archived from the original on 13 February 2020. Retrieved 26 June 2020.
- ↑ Chambers English Thesaurus. Allied Publishers. p. 175. ISBN 978-81-86062-04-3. Archived from the original on 25 July 2020. Retrieved 26 June 2020.
- 1 2 WHO. "Lexicon of alcohol and drug terms published by the World Health Organization". World Health Organization. Archived from the original on 5 February 2013.
- 1 2 Hoffman, PL; Tabakoff, B (July 1996). "Alcohol dependence: a commentary on mechanisms". Alcohol and Alcoholism. 31 (4): 333–40. doi:10.1093/oxfordjournals.alcalc.a008159. PMID 8879279.
- ↑ Dunn, N; Cook, CC (March 1999). "Psychiatric aspects of alcohol misuse". Hospital Medicine. 60 (3): 169–72. doi:10.12968/hosp.1999.60.3.1060. ISSN 1462-3935. PMID 10476237.
- ↑ Wilson, Richard; Kolander, Cheryl A. (2003). Drug abuse prevention: a school and community partnership. Sudbury, MA: Jones and Bartlett. pp. 40–45. ISBN 978-0-7637-1461-1. Archived from the original on 19 March 2022. Retrieved 15 August 2022.
- ↑ "Biology". The Volume Library. Vol. 1. Nashville, TN: The Southwestern Company. 2009. p. 29. ISBN 978-0-87197-208-8.
{{cite book}}: CS1 maint: url-status (link) - 1 2 3 4 O'Keefe, JH; Bhatti, SK; Bajwa, A; DiNicolantonio, JJ; Lavie, CJ (March 2014). "Alcohol and cardiovascular health: the dose makes the poison ... or the remedy". Mayo Clinic Proceedings. 89 (3): 382–93. doi:10.1016/j.mayocp.2013.11.005. PMID 24582196.
- ↑ Alcohol and Heart Health Archived 19 January 2016 at the Wayback Machine American Heart Association
- ↑ American Medical Association (2003). Leiken, Jerrold B. MD; Lipsky, Martin S. MD (eds.). Complete Medical Encyclopedia (First ed.). New York: Random House Reference. p. 485. ISBN 978-0-8129-9100-0. Archived from the original on 9 May 2022. Retrieved 15 August 2022.
- ↑ Müller, D; Koch, RD; von Specht, H; Völker, W; Münch, EM (March 1985). "[Neurophysiologic findings in chronic alcohol abuse]". Psychiatr Neurol Med Psychol (Leipz) (in German). 37 (3): 129–32. PMID 2988001.
{{cite journal}}: CS1 maint: unrecognized language (link) - ↑ Testino, G. (2008). "Alcoholic Diseases in Hepato-Gastroenterology: a point of view". Hepatogastroenterology. 55 (82–83): 371–77. PMID 18613369.
- ↑ 10th Special Report to the U.S. Congress on Alcohol and Health Archived 13 September 2012 at the Wayback Machine, 2000, U.S. Department of Health and Human Services, Public Health Service National Institutes of Health, National Institute on Alcohol Abuse and Alcoholism.
- 1 2 3 Blum, Laura N.; Nielsen, Nancy H.; Riggs, Joseph A.; Council on Scientific Affairs, American Medical Association (September 1998). "Alcoholism and alcohol abuse among women: report of the council on scientific affairs". Journal of Women's Health. 7 (7): 861–70. doi:10.1089/jwh.1998.7.861. PMID 9785312.
{{cite journal}}: Cite has empty unknown parameter:|1=(help) - 1 2 Walter, H; Gutierrez, K; Ramskogler, K; Hertling, I; Dvorak, A; Lesch, OM (November 2003). "Gender-specific differences in alcoholism: implications for treatment". Archives of Women's Mental Health. 6 (4): 253–58. doi:10.1007/s00737-003-0014-8. PMID 14628177.
- ↑ Mihai, B; Lăcătuşu, C; Graur, M (April–June 2008). "[Alcoholic ketoacidosis]". Rev Med Chir Soc Med Nat Iasi. 112 (2): 321–26. PMID 19294998.
- ↑ Sibaï, K; Eggimann, P (September 2005). "[Alcoholic ketoacidosis: not rare cause of metabolic acidosis]". Rev Med Suisse. 1 (32): 2106, 2108–10, 2112–15. PMID 16238232.
- ↑ Cederbaum, AI (2012). "Alcohol metabolism". Clin Liver Dis. 16 (4): 667–85. doi:10.1016/j.cld.2012.08.002. PMC 3484320. PMID 23101976.
- 1 2 Bakalkin, Georgy (8 July 2008). "Alcoholism-associated molecular adaptations in brain neurocognitive circuits". Eurekalert.org. Archived from the original on 30 November 2011. Retrieved 11 January 2012.
- ↑ Oscar-Berman, M; Marinkovic, K (2003). "Alcoholism and the brain: an overview". Alcohol Res Health. 27 (2): 125–33. PMC 6668884. PMID 15303622.
- ↑ Uekermann, J; Daum, I (May 2008). "Social cognition in alcoholism: a link to prefrontal cortex dysfunction?". Addiction. 103 (5): 726–35. doi:10.1111/j.1360-0443.2008.02157.x. PMID 18412750.
- ↑ Wetterling, T; Junghanns, K (September 2000). "Psychopathology of alcoholics during withdrawal and early abstinence". Eur Psychiatry. 15 (8): 483–88. doi:10.1016/S0924-9338(00)00519-8. ISSN 0924-9338. PMID 11175926.
- ↑ Schuckit, MA (November 1983). "Alcoholism and other psychiatric disorders". Hosp Community Psychiatry. 34 (11): 1022–27. doi:10.1176/ps.34.11.1022. ISSN 0022-1597. PMID 6642446.
- ↑ Cowley, DS (24 January 1992). "Alcohol abuse, substance abuse, and panic disorder". Am J Med. 92 (1A): 41S–48S. doi:10.1016/0002-9343(92)90136-Y. ISSN 0002-9343. PMID 1346485.
- ↑ Cosci, F; Schruers, KR; Abrams, K; Griez, EJ (June 2007). "Alcohol use disorders and panic disorder: a review of the evidence of a direct relationship". J Clin Psychiatry. 68 (6): 874–80. doi:10.4088/JCP.v68n0608. ISSN 0160-6689. PMID 17592911.
- ↑ Grant, BF; Harford, TC (October 1995). "Comorbidity between DSM-IV alcohol use disorders and major depression: results of a national survey". Drug Alcohol Depend. 39 (3): 197–206. doi:10.1016/0376-8716(95)01160-4. ISSN 0376-8716. PMID 8556968. Archived from the original on 28 November 2020. Retrieved 26 June 2020.
- ↑ Kandel, DB; Huang, FY; Davies, M (October 2001). "Comorbidity between patterns of substance use dependence and psychiatric syndromes". Drug Alcohol Depend. 64 (2): 233–41. doi:10.1016/S0376-8716(01)00126-0. ISSN 0376-8716. PMID 11543993.
- ↑ Cornelius, JR; Bukstein, O; Salloum, I; Clark, D (2003). Alcohol and psychiatric comorbidity. Recent Dev Alcohol. Recent Developments in Alcoholism. Vol. 16. pp. 361–74. doi:10.1007/0-306-47939-7_24. ISBN 978-0-306-47258-9. ISSN 0738-422X. PMID 12638646.
- ↑ Schuckit, MA; Tipp, JE; Bergman, M; Reich, W; Hesselbrock, VM; Smith, TL (July 1997). "Comparison of induced and independent major depressive disorders in 2,945 alcoholics". Am J Psychiatry. 154 (7): 948–57. doi:10.1176/ajp.154.7.948. ISSN 0002-953X. PMID 9210745.
- ↑ Schuckit, MA; Tipp, JE; Bucholz, KK; Nurnberger, JI; Hesselbrock, VM; Crowe, RR; Kramer, J (October 1997). "The life-time rates of three major mood disorders and four major anxiety disorders in alcoholics and controls". Addiction. 92 (10): 1289–304. doi:10.1111/j.1360-0443.1997.tb02848.x. ISSN 0965-2140. PMID 9489046. S2CID 14958283.
- ↑ Schuckit, MA; Smith, TL; Danko, GP; Pierson, J; Trim, R; Nurnberger, JI; Kramer, J; Kuperman, S; Bierut, LJ; Hesselbrock, V (November 2007). "A comparison of factors associated with substance-induced versus independent depressions". J Stud Alcohol Drugs. 68 (6): 805–12. doi:10.15288/jsad.2007.68.805. ISSN 1937-1888. PMID 17960298. S2CID 17528609.
- ↑ Schuckit, M (June 1983). "Alcoholic patients with secondary depression". Am J Psychiatry. 140 (6): 711–14. doi:10.1176/ajp.140.6.711. ISSN 0002-953X. PMID 6846629.
- 1 2 3 Karrol, Brad R. (2002). "Women and alcohol use disorders: a review of important knowledge and its implications for social work practitioners". Journal of Social Work. 2 (3): 337–56. doi:10.1177/146801730200200305.
- 1 2 3 McCully, Chris (2004). Goodbye Mr. Wonderful. Alcohol, Addition and Early Recovery. London: Jessica Kingsley Publishers. ISBN 978-1-84310-265-6. Archived from the original on 21 November 2009.
- ↑ Isralowitz, Richard (2004). Drug use: a reference handbook. Santa Barbara, CA: ABC-CLIO. pp. 122–23. ISBN 978-1-57607-708-5. Archived from the original on 22 December 2021. Retrieved 26 June 2020.
- ↑ Langdana, Farrokh K. (2009). Macroeconomic Policy: Demystifying Monetary and Fiscal Policy (2nd ed.). Springer. p. 81. ISBN 978-0-387-77665-1. Archived from the original on 19 March 2022. Retrieved 15 August 2022.
- ↑ Gifford, Maria (2009). Alcoholism (Biographies of Disease). Greenwood Press. pp. 89–91. ISBN 978-0-313-35908-8. Archived from the original on 19 March 2022. Retrieved 15 August 2022.
- ↑ Schadé, Johannes Petrus (2006). The Complete Encyclopedia of Medicine and Health. Foreign Media Books. pp. 132–33. ISBN 978-1-60136-001-4. Archived from the original on 17 August 2022. Retrieved 26 June 2020.
- ↑ Gold, Mark. "Children of Alcoholics". Psych Central. Archived from the original on 16 November 2011. Retrieved 27 November 2011.
- ↑ Galanter, Marc; Kleber, Herbert D. (2008). The American Psychiatric Publishing Textbook of Substance Abuse Treatment (4th ed.). American Psychiatric Publishing Inc. p. 58. ISBN 978-1-58562-276-4.
- ↑ Dart, Richard C. (2003). Medical Toxicology (3rd ed.). Lippincott Williams & Wilkins. pp. 139–40. ISBN 978-0-7817-2845-4. Archived from the original on 19 March 2022. Retrieved 15 August 2022.
- ↑ Idemudia, SO; Bhadra, S; Lal, H (June 1989). "The pentylenetetrazol-like interoceptive stimulus produced by ethanol withdrawal is potentiated by bicuculline and picrotoxinin". Neuropsychopharmacology. 2 (2): 115–22. doi:10.1016/0893-133X(89)90014-6. ISSN 0893-133X. PMID 2742726.
- ↑ Chastain, G (October 2006). "Alcohol, neurotransmitter systems, and behavior". The Journal of General Psychology. 133 (4): 329–35. doi:10.3200/GENP.133.4.329-335. ISSN 0022-1309. PMID 17128954.
- 1 2 3 Heilig, M; Egli, M; Crabbe, JC; Becker, HC (April 2010). "Acute withdrawal, protracted abstinence and negative affect in alcoholism: are they linked?". Addict Biol. 15 (2): 169–84. doi:10.1111/j.1369-1600.2009.00194.x. PMC 3268458. PMID 20148778.
- ↑ Johnson, Bankole A. (2011). Addiction medicine : science and practice. New York: Springer. pp. 301–03. ISBN 978-1-4419-0337-2. Archived from the original on 1 December 2015.
- ↑ Breese, GR; Sinha, R; Heilig, M (February 2011). "Chronic alcohol neuroadaptation and stress contribute to susceptibility for alcohol craving and relapse". Pharmacol Ther. 129 (2): 149–71. doi:10.1016/j.pharmthera.2010.09.007. PMC 3026093. PMID 20951730.
- ↑ Sullivan, JT; Sykora, K; Schneiderman, J; Naranjo, CA; Sellers, EM (November 1989). "Assessment of alcohol withdrawal: the revised clinical institute withdrawal assessment for alcohol scale (CIWA-Ar)" (PDF). Br J Addict. 84 (11): 1353–57. CiteSeerX 10.1.1.489.341. doi:10.1111/j.1360-0443.1989.tb00737.x. PMID 2597811. Archived from the original (PDF) on 10 August 2013. Retrieved 25 October 2017.
- 1 2 3 4 5 Enoch, MA (December 2006). "Genetic and environmental influences on the development of alcoholism: resilience vs. risk". Annals of the New York Academy of Sciences. 1094 (1): 193–201. Bibcode:2006NYASA1094..193E. doi:10.1196/annals.1376.019. PMID 17347351. Archived from the original on 25 July 2020. Retrieved 26 June 2020.
- 1 2 3 4 5 6 7 8 Edenberg, Howard J.; McClintick, Jeanette N. (11 November 2018). "Alcohol Dehydrogenases, Aldehyde Dehydrogenases, and Alcohol Use Disorders: A Critical Review". Alcoholism: Clinical and Experimental Research. 42 (12): 2281–2297. doi:10.1111/acer.13904. ISSN 0145-6008. PMC 6286250. PMID 30320893.
- ↑ Bierut, LJ; Schuckit, MA; Hesselbrock, V; Reich, T (2000). "Co-occurring risk factors for alcohol dependence and habitual smoking". Alcohol Res Health. 24 (4): 233–41. PMC 6709743. PMID 15986718.
- ↑ Agrawal, A; Sartor, CE; Lynskey, MT; Grant, JD; Pergadia, ML; Grucza, R; Bucholz, KK; Nelson, EC; Madden, PA; Martin, NG; Heath, AC (2009). "Evidence for an Interaction Between Age at 1st Drink and Genetic Influences on DSM-IV Alcohol Dependence Symptoms". Alcoholism: Clinical and Experimental Research. 33 (12): 2047–56. doi:10.1111/j.1530-0277.2009.01044.x. PMC 2883563. PMID 19764935.
- 1 2 "Early Age At First Drink May Modify Tween/Teen Risk For Alcohol Dependence". Medical News Today. 21 September 2009. Archived from the original on 13 February 2010.
- ↑ Schwandt, ML; Lindell, SG; Chen, S; Higley, JD; Suomi, SJ; Heilig, M; Barr, CS (February 2010). "Alcohol Response and Consumption in Adolescent Rhesus Macaques: Life History and Genetic Influences". Alcohol. 44 (1): 67–80. doi:10.1016/j.alcohol.2009.09.034. PMC 2818103. PMID 20113875.
- ↑ Crews, FT; Boettiger, CA (September 2009). "Impulsivity, Frontal Lobes and Risk for Addiction". Pharmacol Biochem Behav. 93 (3): 237–47. doi:10.1016/j.pbb.2009.04.018. PMC 2730661. PMID 19410598.
- ↑ Weinberger, A.H.; Platt, J; Goodwin, R.D. (2016). "Is cannabis use associated with an increased risk of onset and persistence of alcohol use disorders? A three-year prospective study among adults in the United States". Drug and Alcohol Dependence. 161: 363–67. doi:10.1016/j.drugalcdep.2016.01.014. PMC 5028105. PMID 26875671.
- ↑ Kirby, T; Barry, A.E. (2012). "Alcohol as a gateway drug: A study of US 12th graders" (PDF). Journal of School Health. 82 (8): 371–79. doi:10.1111/j.1746-1561.2012.00712.x. PMID 22712674. Archived (PDF) from the original on 4 June 2016.
- ↑ "Volume of World Beer Production". European Beer Guide. Archived from the original on 28 October 2006. Retrieved 17 October 2006.
- ↑ Nelson, Max (2005). The Barbarian's Beverage: A History of Beer in Ancient Europe. Abingdon, Oxon: Routledge. p. 1. ISBN 978-0-415-31121-2. Archived from the original on 25 July 2020. Retrieved 21 September 2010.
- ↑ Rudgley, Richard (1993). The Alchemy of Culture: Intoxicants in Society. London: British Museum Press. p. 411. ISBN 978-0-7141-1736-2. Archived from the original on 25 July 2020. Retrieved 13 January 2012.
- ↑ Arnold, John P (2005). Origin and History of Beer and Brewing: From Prehistoric Times to the Beginning of Brewing Science and Technology. Cleveland, OH. p. 411. ISBN 978-0-9662084-1-2. Archived from the original on 25 July 2020. Retrieved 13 January 2012.
- ↑ Joshua J. Mark (2011). Beer Archived 3 July 2014 at the Wayback Machine. Ancient History Encyclopedia.
- ↑ McFarland, Ben (2009). World's Best Beers: One Thousand. Sterling Publishing Company, Inc. ISBN 978-1-4027-6694-7. Archived from the original on 25 July 2020. Retrieved 26 June 2020.
- ↑ "Gender differences in alcohol use and alcohol dependence or abuse: 2004 or 2005." The NSDUH Report. Accessed 22 June 2012.
- 1 2 3 Walters, Raymond K.; Polimanti, Renato; Johnson, Emma C.; McClintick, Jeanette N.; Adams, Mark J.; Adkins, Amy E.; Aliev, Fazil; Bacanu, Silviu-Alin; Batzler, Anthony; Bertelsen, Sarah; Biernacka, Joanna M. (2018). "Trans-ancestral GWAS of alcohol dependence reveals common genetic underpinnings with psychiatric disorders". Nature Neuroscience. 21 (12): 1656–1669. doi:10.1038/s41593-018-0275-1. ISSN 1097-6256. PMC 6430207. PMID 30482948.
- 1 2 Kranzler, Henry R.; Zhou, Hang; Kember, Rachel L.; Vickers Smith, Rachel; Justice, Amy C.; Damrauer, Scott; Tsao, Philip S.; Klarin, Derek; Baras, Aris; Reid, Jeffrey; Overton, John (2 April 2019). "Genome-wide association study of alcohol consumption and use disorder in 274,424 individuals from multiple populations". Nature Communications. 10 (1): 1499. Bibcode:2019NatCo..10.1499K. doi:10.1038/s41467-019-09480-8. ISSN 2041-1723. PMC 6445072. PMID 30940813.
- 1 2 Eng, MY; Luczak, SE; Wall, TL (2007). "ALDH2, ADH1B, and ADH1C genotypes in Asians: a literature review". Alcohol Res Health. 30 (1): 22–27. PMC 3860439. PMID 17718397.
- 1 2 Ehlers, CL (2007). "Variations in ADH and ALDH in Southwest California Indians". Alcohol Res Health. 30 (1): 14–17. PMC 3860438. PMID 17718395.
- ↑ Scott, DM; Taylor, RE (2007). "Health-related effects of genetic variations of alcohol-metabolizing enzymes in African Americans". Alcohol Res Health. 30 (1): 18–21. PMC 3860436. PMID 17718396.
- ↑ Szlemko, WJ; Wood, JW; Thurman, PJ (October 2006). "Native Americans and alcohol: past, present, and future". J Gen Psychol. 133 (4): 435–51. doi:10.3200/GENP.133.4.435-451. PMID 17128961.
- ↑ Spillane, NS; Smith, GT (May 2007). "A theory of reservation-dwelling American Indian alcohol use risk". Psychol Bull. 133 (3): 395–418. doi:10.1037/0033-2909.133.3.395. PMID 17469984.
- ↑ Schumann, G; et al. (2016). "KLB is associated with alcohol drinking, and its gene product β-Klotho is necessary for FGF21 regulation of alcohol preference". PNAS USA. 113 (50): 14372–77. doi:10.1073/pnas.1611243113. PMC 5167198. PMID 27911795. S2CID 4060021.
- ↑ American Heritage Dictionaries (2006). The American Heritage dictionary of the English language (4 ed.). Boston: Houghton Mifflin. ISBN 978-0-618-70172-8. Archived from the original on 7 September 2021. Retrieved 15 August 2022.
To use wrongly or improperly; misuse: abuse alcohol
- ↑ "Dietary Guidelines for Americans 2005". health.gov. 2005. Archived from the original on 1 July 2007. Retrieved 28 November 2009. Dietary Guidelines
- ↑ See question 16 of the Severity of Alcohol Dependence Questionnaire.
- ↑ "Young Adult Drinking". Alcohol Alert (68). April 2006. Archived from the original on 13 February 2013. Retrieved 18 February 2013.
- ↑ Esser, Marissa B.; Hedden, Sarra L.; Kanny, Dafna; Brewer, Robert D.; Gfroerer, Joseph C.; Naimi, Timothy S. (20 November 2014). "Prevalence of Alcohol Dependence Among US Adult Drinkers, 2009–2011". Preventing Chronic Disease. 11: E206. doi:10.5888/pcd11.140329. PMC 4241371. PMID 25412029.
- ↑ McGovern, Thomas F.; White, William L. (2003). Alcohol Problems in the United States: Twenty Years of Treatment Perspective. Routledge. pp. 7–. ISBN 978-0-7890-2049-9. Archived from the original on 8 April 2014. Retrieved 17 April 2010.
- ↑ "alcoholism" at Dorland's Medical Dictionary
- 1 2 3 Thombs, Dennis L (1999). Introduction To Addictive Behaviors 2ed. London: The Guildford Press. pp. 64–65.
{{cite book}}: CS1 maint: url-status (link) - 1 2 VandenBos, Gary R. (2006). APA dictionary of psychology. Washington, DC: American Psychological Association. ISBN 978-1-59147-380-0. Archived from the original on 7 September 2021. Retrieved 15 August 2022.
- 1 2 "Diagnostic Criteria for Alcohol Abuse and Dependence – Alcohol Alert No. 30-1995". Archived from the original on 27 March 2010. Retrieved 17 April 2010.
- ↑ Martin, CS; Chung, T; Langenbucher, JW (August 2008). "How Should We Revise Diagnostic Criteria for Substance Use Disorders in the DSM–V?". J Abnorm Psychol. 117 (3): 561–75. doi:10.1037/0021-843X.117.3.561. PMC 2701140. PMID 18729609.
- ↑ "Proposed Revision | APA DSM-5". Archived from the original on 25 March 2010. Retrieved 17 April 2010.
- ↑ "A System to Convert ICD Diagnostic Codes for Alcohol Research". Archived from the original on 24 April 2009. Retrieved 17 April 2010.
- ↑ Diagnostic and statistical manual of mental disorders: DSM-IV. Washington, DC: American Psychiatric Association. 1994. ISBN 978-0-89042-025-6. Archived from the original on 25 July 2020. Retrieved 26 June 2020.
- ↑ Morse, RM; Flavin, DK (August 1992). "The definition of alcoholism. The Joint Committee of the National Council on Alcoholism and Drug Dependence and the American Society of Addiction Medicine to Study the Definition and Criteria for the Diagnosis of Alcoholism". JAMA: The Journal of the American Medical Association. 268 (8): 1012–14. doi:10.1001/jama.1992.03490080086030. ISSN 0098-7484. PMID 1501306.
- ↑ Alcoholism at the US National Library of Medicine Medical Subject Headings (MeSH)
- 1 2 3 The first 100 members of AA (2001) [1939]. Alcoholics Anonymous: the story of how many thousands of men and women have recovered from alcoholism. New York: Alcoholics Anonymous World Services. pp. xxxii, 575. ISBN 978-1-893007-16-1. Archived from the original on 30 April 2017.
{{cite book}}: Unknown parameter|nopp=ignored (help) - ↑ Kay, AB (2000). "Overview of 'allergy and allergic diseases: with a view to the future'". Br. Med. Bull. 56 (4): 843–64. doi:10.1258/0007142001903481. ISSN 0007-1420. PMID 11359624.
- ↑ "The Big Book Self Test". intoaction.us. Archived from the original on 23 November 2007. Retrieved 19 February 2008.
- ↑ "October 22 Deaths". todayinsci.com. Archived from the original on 7 February 2008. Retrieved 18 February 2008.
- 1 2 Volkow, Nora. "Science of Addiction" (PDF). American Medical Association. Archived (PDF) from the original on 29 June 2011.
- ↑ US Preventive Services Task, Force.; Curry, SJ; Krist, AH; Owens, DK; Barry, MJ; Caughey, AB; Davidson, KW; Doubeni, CA; Epling JW, Jr; Kemper, AR; Kubik, M; Landefeld, CS; Mangione, CM; Silverstein, M; Simon, MA; Tseng, CW; Wong, JB (13 November 2018). "Screening and Behavioral Counseling Interventions to Reduce Unhealthy Alcohol Use in Adolescents and Adults: US Preventive Services Task Force Recommendation Statement". JAMA. 320 (18): 1899–1909. doi:10.1001/jama.2018.16789. PMID 30422199.
- ↑ Kahan, M (April 1996). "Identifying and managing problem drinkers". Can Fam Physician. 42: 661–71. PMC 2146411. PMID 8653034.
- ↑ Ewing, JA (October 1984). "Detecting alcoholism. The CAGE questionnaire". JAMA: The Journal of the American Medical Association. 252 (14): 1905–07. doi:10.1001/jama.1984.03350140051025. ISSN 0098-7484. PMID 6471323.
- ↑ "CAGE questionnaire – screen for alcohol misuse" (PDF). Archived from the original (PDF) on 28 July 2011.
- ↑ Dhalla, S; Kopec, JA (2007). "The CAGE questionnaire for alcohol misuse: a review of reliability and validity studies". Clin Invest Med. 30 (1): 33–41. doi:10.25011/cim.v30i1.447. PMID 17716538.
- ↑ Raistrick, D.; Dunbar, G.; Davidson, R. (1983). "Alcohol Dependence Data Questionnaire (SADD)". European Monitoring Centre for Drugs and Drug Addiction. Archived from the original on 21 July 2016.
- ↑ "Michigan Alcohol Screening Test". The National Council on Alcoholism and Drug Dependence. Archived from the original on 6 September 2006.
- ↑ Babor, Thomas F.; Higgins-Biddle, John C.; Saunders, John B.; Monteiro, Maristela G. (2001). "The Alcohol Use Disorders Identification Test; Guidelines for Use in Primary Care" (PDF). World Health Organization. Archived from the original (PDF) on 2 May 2006.
- ↑ Smith, SG; Touquet, R; Wright, S; Das Gupta, N (September 1996). "Detection of alcohol misusing patients in accident and emergency departments: the Paddington alcohol test (PAT)". Journal of Accident and Emergency Medicine. 13 (5): 308–12. doi:10.1136/emj.13.5.308. ISSN 1351-0622. PMC 1342761. PMID 8894853.
- ↑ Jones, AW (2006). "Urine as a biological specimen for forensic analysis of alcohol and variability in the urine-to-blood relationship". Toxicol Rev. 25 (1): 15–35. doi:10.2165/00139709-200625010-00002. PMID 16856767.
- ↑ Das, SK; Dhanya, L; Vasudevan, DM (2008). "Biomarkers of alcoholism: an updated review". Scand J Clin Lab Invest. 68 (2): 81–92. doi:10.1080/00365510701532662. PMID 17852805.
- ↑ World Health Organization (2010). "Alcohol". Archived from the original on 26 February 2010.
- ↑ "Alcohol policy in the WHO European Region: current status and the way forward" (PDF). World Health Organization. 12 September 2005. Archived from the original (PDF) on 23 January 2010.
- ↑ Crews, F; He, J; Hodge, C (February 2007). "Adolescent cortical development: a critical period of vulnerability for addiction". Pharmacol Biochem Behav. 86 (2): 189–99. doi:10.1016/j.pbb.2006.12.001. PMID 17222895.
- 1 2 Gabbard, Glen O. (2001). Treatments of psychiatric disorders (3 ed.). Washington, DC: American Psychiatric Press. ISBN 978-0-88048-910-2. Archived from the original on 25 April 2022. Retrieved 15 August 2022.
- ↑ Stavro, K; Pelletier, J; Potvin, S (January 2012). "Widespread and sustained cognitive deficits in alcoholism: a meta-analysis". Addict Biol. 18 (2): 203–13. doi:10.1111/j.1369-1600.2011.00418.x. PMID 22264351.
- ↑ Smith, M.A., Melinda; Saisan, M.S.W., Joanna (2016). "Self-Help Groups for Alcohol Addiction". Archived from the original on 21 May 2015.
- ↑ Kelly JF, Humphreys K, Ferri M (2020). "Alcoholics Anonymous and other 12‐step programs for alcohol use disorder". Cochrane Database of Systematic Reviews (Systematic review). 3: CD012880. doi:10.1002/14651858.CD012880.pub2. PMC 7065341. PMID 32159228.
- ↑ Dawson, DA; Grant, BF; Stinson, FS; Chou, PS; Huang, B; Ruan, WJ (2005). "Recovery from DSM-IV alcohol dependence: United States, 2001–2002". Addiction. 100 (3): 281–92. doi:10.1111/j.1360-0443.2004.00964.x. PMID 15733237. Archived from the original on 19 July 2011.
- ↑ Dawson, DA; Goldstein, RB; Grant, BF (2007). "Rates and correlates of relapse among individuals in remission from DSM-IV alcohol dependence: a 3-year follow-up". Alcoholism: Clinical and Experimental Research. 31 (12): 2036–45. doi:10.1111/j.1530-0277.2007.00536.x. PMID 18034696. Archived from the original on 25 July 2020. Retrieved 26 June 2020.
- ↑ Sobell, Mark B.; Sobell, Linda C. (1973). "Individualized behavior therapy for alcoholics". Behavior Therapy. 4: 49–72. doi:10.1016/S0005-7894(73)80074-7.
- ↑ Pendery, M.; Maltzman, I.; West, L. (1982). "Controlled drinking by alcoholics? New findings and a reevaluation of a major affirmative study". Science. 217 (4555): 169–175. Bibcode:1982Sci...217..169P. doi:10.1126/science.7089552. PMID 7089552.
- ↑ "Alcoholism Study Under New Attack". The New York Times. 28 June 1982. Archived from the original on 24 June 2020. Retrieved 26 June 2020.
The new article will say that, 10 years later, four of the 20 had died from alcohol-related causes. Eight others were still drinking excessively, six were abstinent but in most cases after multiple hospitalizations, and one was drinking moderately. The alcohol dependence of that last case was also questioned. Another subject, who could not be found, was reported gravely disabled.
- ↑ Vaillant, GE (2003). "A 60-year follow-up of alcoholic men". Addiction. 98 (8): 1043–51. doi:10.1046/j.1360-0443.2003.00422.x. PMID 12873238. S2CID 12835128.
- ↑ Riper, H; Hoogendoorn, A; Cuijpers, P; Karyotaki, E; Boumparis, N; Mira, A; Andersson, G; Berman, AH; Bertholet, N; Bischof, G; Blankers, M; Boon, B; Boß, L; Brendryen, H; Cunningham, J; Ebert, D; Hansen, A; Hester, R; Khadjesari, Z; Kramer, J; Murray, E; Postel, M; Schulz, D; Sinadinovic, K; Suffoletto, B; Sundström, C; de Vries, H; Wallace, P; Wiers, RW; Smit, JH (December 2018). "Effectiveness and treatment moderators of internet interventions for adult problem drinking: An individual patient data meta-analysis of 19 randomised controlled trials". PLOS Medicine. 15 (12): e1002714. doi:10.1371/journal.pmed.1002714. PMC 6298657. PMID 30562347.
- ↑ "Alcohol and Other Drugs". Alcohol Alert. National Institute on Alcohol Abuse and Alcoholism (76). July 2008. Archived from the original on 28 July 2013. Retrieved 11 July 2013.
- ↑ Mason, BJ; Heyser, CJ (January 2010). "The neurobiology, clinical efficacy and safety of acamprosate in the treatment of alcohol dependence". Expert Opin Drug Saf. 9 (1): 177–88. doi:10.1517/14740330903512943. PMID 20021295.
- ↑ Mason, BJ; Heyser, CJ (March 2010). "Acamprosate: A prototypic neuromodulator in the treatment of alcohol dependence". CNS Neurol Disord Drug Targets. 9 (1): 23–32. doi:10.2174/187152710790966641. PMC 2853976. PMID 20201812.
- ↑ Rösner, S; Hackl-Herrwerth, A; Leucht, S; Lehert, P; Vecchi, S; Soyka, M (2010). Rösner, Susanne (ed.). "Acamprosate for alcohol dependence". Cochrane Database of Systematic Reviews (Submitted manuscript). 128 (9): 379. doi:10.1002/14651858.CD004332.pub2. PMID 20824837. Archived from the original on 8 July 2020. Retrieved 26 June 2020.
- 1 2 3 4 Jonas, DE; Amick, HR; Feltner, C; Bobashev, G; Thomas, K; Wines, R; Kim, MM; Shanahan, E; Gass, CE; Rowe, CJ; Garbutt, JC (14 May 2014). "Pharmacotherapy for Adults With Alcohol Use Disorders in Outpatient Settings". JAMA. 311 (18): 1889–900. doi:10.1001/jama.2014.3628. PMID 24825644.
- ↑ Soyka, M; Rösner, S (November 2008). "Opioid antagonists for pharmacological treatment of alcohol dependence – a critical review". Curr Drug Abuse Rev. 1 (3): 280–91. doi:10.2174/1874473710801030280. PMID 19630726.
- ↑ Anderson, Kenneth (28 July 2013). "Drink Your Way Sober with Naltrexone". Psychology Today. Archived from the original on 20 June 2014. Retrieved 18 July 2016.
- 1 2 Sinclair, JD (2001). "Evidence about the use of naltrexone and for different ways of using it in the treatment of alcoholism". Alcohol and Alcoholism. 36 (1): 2–10. doi:10.1093/alcalc/36.1.2. PMID 11139409.
- ↑ Lindsay, S.J.E.; Powell, Graham E., eds. (28 July 1998). The Handbook of Clinical Adult Psychology (2nd ed.). Routledge. p. 402. ISBN 978-0-415-07215-1.
- ↑ Gitlow, Stuart (2006). Substance Use Disorders: A Practical Guide (2nd ed.). Lippincott Williams & Wilkins. pp. 52, 103–21. ISBN 978-0-7817-6998-3. Archived from the original on 25 July 2020. Retrieved 26 June 2020.
- ↑ Kushner, MG; Abrams, K; Borchardt, C (March 2000). "The relationship between anxiety disorders and alcohol use disorders: a review of major perspectives and findings". Clin Psychol Rev. 20 (2): 149–71. doi:10.1016/S0272-7358(99)00027-6. PMID 10721495.
- ↑ Ogborne, AC (June 2000). "Identifying and treating patients with alcohol-related problems". CMAJ. 162 (12): 1705–08. PMC 1232509. PMID 10870503.
- 1 2 Soyka, M; Müller, CA (August 2017). "Pharmacotherapy of alcoholism – an update on approved and off-label medications". Expert Opinion on Pharmacotherapy. 18 (12): 1187–99. doi:10.1080/14656566.2017.1349098. PMID 28658981.
- ↑ Cservenka, A; Yardley, MM; Ray, LA (August 2017). "Review: Pharmacogenetics of alcoholism treatment: Implications of ethnic diversity". The American Journal on Addictions. 26 (5): 516–25. doi:10.1111/ajad.12463. PMC 5484746. PMID 28134463.
- ↑ Poulos, CX; Zack, M (November 2004). "Low-dose diazepam primes motivation for alcohol and alcohol-related semantic networks in problem drinkers". Behav Pharmacol. 15 (7): 503–12. doi:10.1097/00008877-200411000-00006. ISSN 0955-8810. PMID 15472572.
- ↑ Johansson, BA; Berglund, M; Hanson, M; Pöhlén, C; Persson, I (November 2003). "Dependence on legal psychotropic drugs among alcoholics" (PDF). Alcohol and Alcoholism. 38 (6): 613–18. doi:10.1093/alcalc/agg123. ISSN 0735-0414. PMID 14633651. Archived from the original on 20 February 2009.
- ↑ Zuskin, E; Jukić, V; Lipozencić, J; Matosić, A; Mustajbegović, J; Turcić, N; Poplasen-Orlovac, D; Bubas, M; Prohić, A (December 2006). "[Alcoholism – how it affects health and working capacity]". Arh Hig Rada Toksikol. 57 (4): 413–26. PMID 17265681.
- ↑ American Psychiatric Association practice guidelines for the treatment of psychiatric disorders. Arlington, VA: American Psychiatric Association. 2006. p. 1346. ISBN 978-0-89042-385-1. Archived from the original on 29 May 2016.
- ↑ O'Connor, Rory; Sheehy, Noel (29 January 2000). Understanding suicidal behaviour. Leicester: BPS Books. pp. 33–37. ISBN 978-1-85433-290-5. Archived from the original on 22 December 2021. Retrieved 26 June 2020.
- ↑ The National Institute on Alcohol Abuse and Alcoholism; U.S. Department of Health and Human Services, NIH News (18 January 2005). "2001–2002 Survey Finds That Many Recover From Alcoholism". National Institutes of Health. Archived from the original on 18 August 2006.
- ↑ Vaillant, GE (August 2003). "A 60-year follow-up of alcoholic men". Addiction. 98 (8): 1043–51. doi:10.1046/j.1360-0443.2003.00422.x. ISSN 0965-2140. PMID 12873238. S2CID 12835128.
- 1 2 "Alcohol misuse: How much does it cost?" (PDF). Cabinet Office Strategy Unit. September 2003. Archived from the original (PDF) on 15 May 2011.
- ↑ Hasin, DS; Stinson, FS; Ogburn, E; Grant, BF (2007). "Prevalence, Correlates, Disability, and Comorbidity of DSM-IV Alcohol Abuse and Dependence in the United States". Archives of General Psychiatry. 64 (7): 830–42. doi:10.1001/archpsyc.64.7.830. PMID 17606817.
- ↑ "alcoholism". Encyclopædia Britannica. 2010. Archived from the original on 2 December 2010.
- ↑ Ballas, Dimitris; Dorling, Danny; Hennig, Benjamin (2017). The Human Atlas of Europe. Bristol: Policy Press. p. 73. ISBN 978-1-4473-1354-0.
{{cite book}}: CS1 maint: url-status (link) - ↑ Vonghia, Luisa; Leggio, Lorenzo; Ferrulli, Anna; Bertini, Marco; Gasbarrini, Giovanni; Addolorato, Giovanni; Alcoholism Treatment Study Group (December 2008). "Acute alcohol intoxication". European Journal of Internal Medicine. 19 (8): 561–67. doi:10.1016/j.ejim.2007.06.033. ISSN 1879-0828. PMID 19046719.
- ↑ Dick, DM; Bierut, LJ (April 2006). "The genetics of alcohol dependence". Current Psychiatry Reports. 8 (2): 151–57. doi:10.1007/s11920-006-0015-1. ISSN 1523-3812. PMID 16539893.
- ↑ "About 37 percent of college students could now be considered alcoholics". Emerald Media. Archived from the original on 17 October 2013.
- ↑ Peters, Uwe Henrik (2007). Lexikon Psychiatrie, Psychotherapie, Medizinische Psychologie. Urban Fischer bei Elsev. ISBN 978-3-437-15061-6. Archived from the original on 7 September 2021. Retrieved 15 August 2022.
- ↑ Valverde, Mariana (1998). Diseases of the Will. Cambridge: Cambridge University Press. p. 48. ISBN 978-0-521-64469-3. Archived from the original on 2 May 2022. Retrieved 15 August 2022.
- ↑ Tracy, Sarah J. (2005). Alcoholism in America: from reconstruction to prohibition. Baltimore: Johns Hopkins University Press. pp. 31–52. ISBN 978-0-8018-8119-0. Archived from the original on 7 April 2022. Retrieved 15 August 2022.
- ↑ Alcoholismus chronicus, eller Chronisk alkoholssjukdom. Stockholm und Leipzig. 1852. Archived from the original on 25 July 2020. Retrieved 19 February 2008.
- ↑ Blocker, Jack S. (February 2006). "Did Prohibition Really Work? Alcohol Prohibition as a Public Health Innovation". American Journal of Public Health. 96 (2): 233–43. doi:10.2105/AJPH.2005.065409. PMC 1470475. PMID 16380559.
Nevertheless, once Prohibition became the law of the land, many citizens decided to obey it. Referendum results in the immediate post-Volstead period showed widespread support, and the Supreme Court quickly fended off challenges to the new law. Death rates from cirrhosis and alcoholism, alcoholic psychosis hospital admissions, and drunkenness arrests all declined steeply during the latter years of the 1910s, when both the cultural and the legal climate were increasingly inhospitable to drink, and in the early years after National Prohibition went into effect.
- ↑ Potter, James V. (2008). Substances of Abuse. Vol. 2. AFS Publishing Co. pp. 1–13. ISBN 978-1-930327-46-7. Archived from the original on 25 July 2020. Retrieved 26 June 2020.
- ↑ "Alcohol and health" (PDF). WHO. Archived (PDF) from the original on 25 July 2020. Retrieved 3 May 2020.
- ↑ Streissguth, Ann Pytkowicz (2018). Fetal alcohol syndrome: a guide for families and communities. Baltimore: Paul H Brookes Pub. ISBN 978-1-55766-283-5. Archived from the original on 7 September 2021. Retrieved 15 August 2022.
- ↑ Gerberding, Julie Louise; Cordero, José; Floyd, R. Louise (May 2005). "Fetal Alcohol Syndrome: Guidelines for Referral and Diagnosis" (PDF). US Centers for Disease Control and Prevention. Archived (PDF) from the original on 11 June 2014.
- ↑ "Global Status Report on Alcohol 2004" (PDF). World Health Organization. Archived (PDF) from the original on 30 December 2006. Retrieved 3 January 2007.
- ↑ "Economic cost of alcohol consumption". World Health Organization Global Alcohol Database. Archived from the original on 18 January 2008. Retrieved 3 January 2007.
- ↑ "Q&A: The costs of alcohol". BBC. 19 September 2003. Archived from the original on 19 October 2006.
- ↑ Bouchery, EE; Harwood, HJ; Sacks, JJ; Simon, CJ; Brewer, RD (2011). "Economic Costs of Excessive Alcohol Consumption in the U.S., 2006" (PDF). American Journal of Preventive Medicine. 41 (5): 516–24. CiteSeerX 10.1.1.460.5582. doi:10.1016/j.amepre.2011.06.045. PMID 22011424. Archived from the original (PDF) on 21 July 2018. Retrieved 12 December 2017.
- 1 2 3 Kirouac, Megan; Witkiewitz, Katie (15 October 2017). "Identifying "Hitting Bottom" among Individuals with Alcohol Problems: Development and Evaluation of the Noteworthy Aspects of Drinking Important to Recovery (NADIR)". Substance Use & Misuse. 52 (12): 1602–1615. doi:10.1080/10826084.2017.1293104. ISSN 1082-6084. PMC 6107067. PMID 28557550.
- ↑ "Treatment of Alcohol Addiction". British Medical Journal. 2 (5455): 184–185. 24 July 1965. doi:10.1136/bmj.2.5455.184. ISSN 0007-1447. PMC 1846501. PMID 20790596.
- ↑ "World/Global Alcohol/Drink Consumption". Finfacts Ireland. 2009. Archived from the original on 12 May 2015.
- ↑ Stivers, Richard (2000). Hair of the dog: Irish drinking and its American stereotype. New York: Continuum. ISBN 978-0-8264-1218-8. Archived from the original on 7 April 2022. Retrieved 15 August 2022.
- ↑ Chen, CC; Yin, SJ (2008). "Alcohol abuse and related factors in Asia". International Review of Psychiatry. 20 (5): 425–33. doi:10.1080/09540260802344075. PMID 19012127.
- ↑ Wooksoo, K (2009). "Drinking Culture of Elderly Korean Immigrants in Canada: A Focus Group Study". Journal of Cross-Cultural Gerontology. 24 (4): 339–53. doi:10.1007/s10823-009-9104-z. PMID 19823926.
- ↑ Li, H Z; Rosenblood, L (1994). "Exploring factors influencing alcohol consumption patterns among Chinese and Caucasians". Journal of Studies on Alcohol. 55 (4): 427–33. doi:10.15288/jsa.1994.55.427. PMID 7934050.
- ↑ French, L (2008). "Psychoactive agents and Native American spirituality: Past and present". Contemporary Justice Review. 11 (2): 155–63. doi:10.1080/10282580802058270.
- ↑ Olmsted, CL; Kockler, DR (October 2008). "Topiramate for alcohol dependence". Ann Pharmacother. 42 (10): 1475–80. doi:10.1345/aph.1L157. ISSN 1060-0280. PMID 18698008. S2CID 27071889.
- ↑ Kenna, GA; Lomastro, TL; Schiesl, A; Leggio, L; Swift, RM (May 2009). "Review of topiramate: an antiepileptic for the treatment of alcohol dependence". Curr Drug Abuse Rev. 2 (2): 135–42. doi:10.2174/1874473710902020135. PMID 19630744.
- ↑ Leggio, L; Garbutt, JC; Addolorato, G (March 2010). "Effectiveness and safety of baclofen in the treatment of alcohol dependent patients". CNS & Neurological Disorders Drug Targets. 9 (1): 33–44. doi:10.2174/187152710790966614. PMID 20201813.
- ↑ Liu, Jia; Wang, Lu-Ning (6 November 2019). "Baclofen for alcohol withdrawal". The Cochrane Database of Systematic Reviews. 2019 (11). doi:10.1002/14651858.CD008502.pub6. ISSN 1469-493X. PMC 6831488. PMID 31689723.
- ↑ "Autorisation du baclofène : des conditions d'utilisation trop restrictives ? - A la une". Destination Santé (in français). 25 October 2018. Archived from the original on 8 July 2020. Retrieved 26 June 2020.
- ↑ Kenna, GA (2010). "Medications acting on the serotonergic system for the treatment of alcohol dependent patients". Current Pharmaceutical Design. 16 (19): 2126–35. doi:10.2174/138161210791516396. PMID 20482508.
- ↑ Frood, Arran (9 March 2012). "LSD helps to treat alcoholism". Nature. doi:10.1038/nature.2012.10200. ISSN 1744-7933. Archived from the original on 17 December 2019. Retrieved 26 June 2020.
- ↑ Garcia-Romeu, Albert; Davis, Alan K; Erowid, Fire; Erowid, Earth; Griffiths, Roland R; Johnson, Matthew W (14 May 2019). "Cessation and reduction in alcohol consumption and misuse after psychedelic use". Journal of Psychopharmacology. 33 (9): 1088–1101. doi:10.1177/0269881119845793. ISSN 0269-8811. PMID 31084460.
- ↑ Hill, Amelia (23 August 2012). "LSD could help alcoholics stop drinking, AA founder believed". The Guardian. Archived from the original on 25 July 2020. Retrieved 26 June 2020.
External links
| Classification | |
|---|---|
| External resources |
- Alcohol at Curlie