Subacute sclerosing panencephalitis
| Subacute sclerosing panencephalitis | |
|---|---|
| Other names: Dawson disease | |
 | |
| Subacute sclerosing panencephalitis. | |
| Symptoms | Initial memory loss and irritability; followed by involuntary jerking movements[1] |
| Complications | Seizures, blindness[1] |
| Usual onset | 7-10 yrs after infection with measles[2] |
| Causes | Measles virus[3] |
| Diagnostic method | Based on symptoms, CSF analysis, EEG, medical imaging, brain biopsy[3] |
| Differential diagnosis | Viral encephalitis, autoimmune encephalitis, multiple sclerosis, Creutzfeldt-Jakob disease[3] |
| Prevention | Measles vaccine[1] |
| Treatment | Supportive care[3] |
| Medication | Antivirals, antiseizure medication, antispasmodics[1] |
| Prognosis | Usually fatal within 3 yrs[1] |
| Frequency | About 1 in 10,000 people infected by measles[2] |
Subacute sclerosing panencephalitis (SSPE) is progressive brain inflammation due to persistent measles infection.[3] Onset is generally 7 to 10 years after the initial infection.[2] Initial symptoms include memory loss and irritability which is followed by involuntary jerking movements.[1] Complications may include seizures and blindness.[1]
It is caused by wild-type measles virus, not by vaccine strains.[3] Diagnosis may be based on a combination of symptoms, CSF analysis, EEG findings, medical imaging, and brain biopsy.[3] It differs from the other forms of encephalitis due to measles: primary measles encephalitis, acute post-measles encephalitis, and measles inclusion body encephalitis.[4]
Prevention is by measles vaccination.[1] There is no cure.[1] Treatment may involve the use of antiviral medication such as ribavirin, antiseizure medication, and antispasmodics.[1] Most individuals die within 3 years of the diagnosis.[1]
SSPE affects about 1 in 10,000 people who get measles; though it is more common in those who had measles before the age of 5.[2][5] Rates decreased more than 90% with widespread vaccination against measles.[1] The condition primarily affects children and young adults.[1] Males are more commonly affected than females.[1] The condition was first described in 1933 by Dawson.[6]
Signs and symptoms
SSPE is characterized by a history of a measles infection, followed by an asymptomatic period that lasts 7 years on average but can range from 1 month to 27 years. After the asymptomatic period, progressive neurological deterioration occurs, characterized by behavior change, intellectual problems, myoclonic seizures, blindness, ataxia, and eventually death.[7][8]
Progression
Symptoms progress through the following 4 stages:[9]
- Stage 1: There may be personality changes, mood swings, or depression. Fever and headache may also be present. This stage may last up to 6 months.
- Stage 2: This stage may involve jerking, muscle spasms, seizures, loss of vision, and dementia.
- Stage 3: Jerking movements are replaced by writhing (twisting) movements and rigidity. At this stage complications may result in death.
- Stage 4: The final stage, in which breathing, heart rate, and blood pressure are affected, leading to coma and death.
Pathogenesis
A large number of nucleocapsids are produced in the neurons and the glial cells. In these cells the viral genes that encode envelope proteins have restricted expression.[10] As a result, infectious particles like the M protein are not produced, and the virus is able to survive persistently without evoking an immune response. Eventually the infection will lead to SSPE.[11]
Diagnosis
_(cropped).png.webp)
According to the Merck Manual:[8]
"SSPE is suspected in young patients with dementia and neuromuscular irritability. EEG, CT or MRI, CSF examination, and measles serologic testing are done. EEG shows periodic complexes with high-voltage diphasic waves occurring synchronously throughout the recording. CT or MRI may show cortical atrophy or white matter lesions. CSF examination usually reveals normal pressure, cell count, and total protein content; however, CSF globulin is almost always elevated, constituting up to 20 to 60% of CSF protein. Serum and CSF contain elevated levels of measles virus antibodies. Anti-measles IgG appears to increase as the disease progresses. If test results are inconclusive, brain biopsy may be needed."
Treatment
If the diagnosis is made during stage 1 it may be possible to treat the disease with oral isoprinosine and intraventricular interferon alfa, but the response to these drugs varies from patient to patient,[12] and the only accepted treatments are supportive measures such as anticonvulsants.[8]
Prognosis
In the classic presentation of the disease death occurs in 1 to 3 years,[13] but faster and slower progressions can occur. Faster deterioration in cases of acute fulminant SSPE leads to death within 3 months of diagnosis.[14][15]Although the prognosis is bleak for SSPE past stage 1, there is a 5% spontaneous remission rate—this may be either a full remission that may last many years or an improvement in condition giving a longer progression period or at least a longer period with the less severe symptoms.[15][16]
Epidemiology
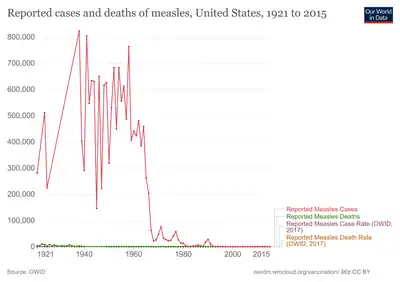
SSPE is a rare condition, although there is still relatively high rates in Asia and the Middle East. However, the number of reported cases is declining since the introduction of the measles vaccine—eradication of the measles virus prevents the SSPE mutation and therefore the progression of the disease or even the initial infection itself.
References
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 "Subacute Sclerosing Panencephalitis Information Page | National Institute of Neurological Disorders and Stroke". www.ninds.nih.gov. Archived from the original on 9 April 2021. Retrieved 16 May 2021.
- 1 2 3 4 "Measles - Vaccine Preventable Diseases Surveillance Manual | CDC". www.cdc.gov. 13 May 2019. Archived from the original on 4 August 2020. Retrieved 16 May 2021.
- 1 2 3 4 5 6 7 Rocke, Z; Belyayeva, M (January 2021). "Subacute Sclerosing Panencephalitis". PMID 32809508.
{{cite journal}}: Cite journal requires|journal=(help) - ↑ Fisher DL, Defres S, Solomon T (2015). "Measles-induced encephalitis". QJM. 108 (3): 177–182. doi:10.1093/qjmed/hcu113. PMID 24865261.
{{cite journal}}: CS1 maint: uses authors parameter (link) - ↑ Mekki, M; Eley, B; Hardie, D; Wilmshurst, JM (October 2019). "Subacute sclerosing panencephalitis: clinical phenotype, epidemiology, and preventive interventions". Developmental medicine and child neurology. 61 (10): 1139–1144. doi:10.1111/dmcn.14166. PMID 30680706.
- ↑ Morris, Huw (2005). Neurology Update: Reviews for Continuing Professional Development. Radcliffe Publishing. p. 77. ISBN 978-1-85775-722-4. Archived from the original on 2021-08-29. Retrieved 2021-05-16.
- ↑ "CDC pinkbook". 2019-03-29. Archived from the original on 2015-02-07. Retrieved 2018-11-04.
- 1 2 3 "merckmanuals.com". Archived from the original on 2018-11-05. Retrieved 2018-11-04.
- ↑ "medline.gov". Archived from the original on 2018-11-04. Retrieved 2018-11-04.
- ↑ Jawetz. Melnick & Adelberg's Medical Microbiology. Lange. 2010. p. 586. ISBN 978-0-07-174271-9.
- ↑ Carter, M. J.; Willcocks, M. M.; Ter Meulen, V. (1983). "Defective translation of measles virus matrix protein in a subacute sclerosing panencephalitis cell line". Nature. 305 (5930): 153–5. Bibcode:1983Natur.305..153C. doi:10.1038/305153a0. PMC 7094927. PMID 6888557.
- ↑
- Gascon G, Yamanis S, Crowell J, et al. Combined oralisoprinosine-intraventricular alpha-interferon therapy for subacute sclerosing panencephalitis. Brain Dev. 1993; 15:346–55.
- Anlar B, Yalaz K, Oktem F; et al. (1997). "Long-term follow-up of patients with subacute sclerosing panencephalitis treated with intraventricular alpha-interferon". Neurology. 48 (2): 526–8. doi:10.1212/wnl.48.2.526. PMID 9040751. S2CID 20412574.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Cianchetti C, Marrosu MG, Muntoni F; et al. (1998). "Intraventricularalpha-interferon in subacute sclerosing panencephalitis". Neurology. 50 (1): 315–16. doi:10.1212/wnl.50.1.315. PMID 9443512. S2CID 33700234.
{{cite journal}}: CS1 maint: multiple names: authors list (link)
- ↑ "SSPE information page www.ninds.nih.gov". Archived from the original on 2021-04-09. Retrieved 2018-11-04.
- ↑ Risk WS, Haddad FS (1979). "The variable natural history of subacute sclerosing panencephalitis: a study of 118 cases from the Middle East". Arch Neurol. 56 (10): 610–14. doi:10.1001/archneur.1979.00500460044004. PMID 485888.
- 1 2 Garg, R K (1 February 2002). "Subacute sclerosing panencephalitis". Postgraduate Medical Journal. 78 (916): 63–70. doi:10.1136/pmj.78.916.63. PMC 1742261. PMID 11807185.
- ↑
- Grunewald T, Lampe J, Weissbrich B; et al. (1998). "A 35-year old bricklayer with hemimyoclonic jerks". Lancet. 351 (9120): 1926. doi:10.1016/s0140-6736(98)04091-4. PMID 9654261. S2CID 206010725.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Santoshkumar B, Radhakrishnan K (1998). "Substantial spontaneous long-term remission in subacute sclerosing panencephalitis (SSPE)". J Neurol Sci. 154 (1): 83–8. doi:10.1016/s0022-510x(97)00303-1. PMID 9543327. S2CID 10635605.
- Grunewald T, Lampe J, Weissbrich B; et al. (1998). "A 35-year old bricklayer with hemimyoclonic jerks". Lancet. 351 (9120): 1926. doi:10.1016/s0140-6736(98)04091-4. PMID 9654261. S2CID 206010725.
External links
- 23-273l. at Merck Manual of Diagnosis and Therapy Home Edition
- NINDS Archived 2021-04-09 at the Wayback Machine
- PubMed Health: Subacute sclerosing panencephalitis Archived 2014-08-08 at the Wayback Machine
- synd/1889 at Who Named It?
| Classification | |
|---|---|
| External resources |
|