Urticaria pigmentosa
| Urticaria pigmentosa | |
|---|---|
| Other names: Generalized eruption of cutaneous mastocytosis (childhood type)[1]: 616 ) | |
.jpg.webp) | |
| Generalised eruption of multiple re-brown macule and papules in urticaria pigmentosa | |
| Specialty | Dermatology |
| Symptoms | Multiple red-brown small bumps and marks which wheal and flare when rubbed, usually on the trunk[2] |
| Usual onset | 75% occur before age 4 years[2] |
| Frequency | Rare |
Urticaria pigmentosa, also known as maculopapular cutaneous mastocytosis, is a generalised eruption of a few to hundreds of small bumps and macules which wheal and flare when rubbed, and typically occur on the trunk in young children.[2] It is the most common form of cutaneous mastocytosis.[2]
It is a rare disease caused by excessive numbers of mast cells in the skin that produce hives or lesions on the skin when irritated.
Signs and symptoms
Urticaria pigmentosa is characterized by excessive amounts of mast cells in the skin. Red or brown spots are often seen on the skin, typically around the chest, forehead, and back. These mast cells, when irritated (e.g. by rubbing the skin, heat exposure), produce too much histamine, triggering an allergic reaction that leads to hives localized to the area of irritation, sometimes referred to as Darier's sign. Severe itching usually follows, and scratching the area only serves to further symptoms. Symptoms can be mild (flushing and hives that require no treatment), moderate (diarrhea, tachycardia, nausea/vomiting, headache, and fainting), or life-threatening (vascular collapse requiring emergency treatment and hospitalization).
 The back of a child with urticaria pigmentosa
The back of a child with urticaria pigmentosa.jpg.webp) Urticaria pigmentosa
Urticaria pigmentosa.jpg.webp) Urticaria pigmentosa
Urticaria pigmentosa.jpg.webp) Urticaria pigmentosa
Urticaria pigmentosa
Cause
The majority of urticaria pigmentosa cases are caused by a point mutation at amino acid 816 of the proto-oncogene c-kit.[3] c-kit is a transmembrane protein which, when bound to Mast Cell Growth Factor (MCGF), signals the cell to divide. Mutations in position 816 of c-kit can result in a constant division signal being sent to the mast cells, resulting in abnormal proliferation. Different mutations have been linked to different onset times of the disease. For example, the Asp816Phe and Asp816Val mutations (the aspartate normally at position 816 in the c-kit protein has been replaced with phenylalanine or valine respectively) have been associated with early manifestation of the disease (mean age of onset: 1.3 and 5.9 months respectively).[4][5] The c-kit gene is encoded on the q12 locus of chromosome 4.[6]
Irritants
Several factors can worsen the symptoms of urticaria pigmentosa:
- Emotional stress
- Physical stimuli such as heat, friction, and excessive exercise
- Bacterial toxins
- Venom
- Eye drops containing dextran
- NSAIDs
- Alcohol
- Morphine
The classification of NSAIDs can be disputed. Aspirin, for example, causes the mast cells to degranulate, releasing histamines and causing symptoms to flare. However, daily intake of 81 mg aspirin may keep the mast cells degranulated. Thus, while symptoms may be worsened at first, they can get better as the mast cells are unable to recharge with histamine.
Diagnosis
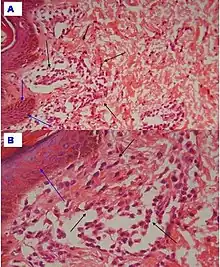
The disease is most often diagnosed as an infant, when parents take their baby in for what appears to be bug bites. The bug bites are actually the clumps of mast cells. Doctors can confirm the presence of mast cells by rubbing the baby's skin. If hives appear, it most likely signifies the presence of urticaria pigmentosa.
Treatments
There are no cures. Antihistamines are useful because they reduce the mast cell's ability to react to histamine.[8]
At least one study suggested that nifedipine, a calcium channel blocker, may reduce mast cell degranulation in people with urticaria pigmentosa. A 1984 study included a person with symptomatic urticaria pigmentosa who responded to nifedipine at dose of 10 mg po tid.[9] However, nifedipine has never been approved by the FDA for treatment of urticaria pigmentosa.
Epidemiology
Urticaria pigmentosa is a rare disease, affecting fewer than 200,000 people in the United States.
See also
References
- ↑ James, William; Berger, Timothy; Elston, Dirk (2005). Andrews' Diseases of the Skin: Clinical Dermatology. (10th ed.). Saunders. ISBN 0-7216-2921-0.
- 1 2 3 4 Johnstone, Ronald B. (2017). "40. Cutaneous Non-lymphoid infiltrates". Weedon's Skin Pathology Essentials (2nd ed.). Elsevier. p. 726. ISBN 978-0-7020-6830-0. Archived from the original on 2023-01-10. Retrieved 2021-09-24.
- ↑ Akin C (2006). "Molecular Diagnosis of Mast Cell Disorders : A Paper from the 2005 William Beaumont Hospital Symposium on Molecular Pathology". J Mol Diagn. 8 (4): 412–9. doi:10.2353/jmoldx.2006.060022. PMC 1867614. PMID 16931579. Archived from the original on 2009-09-03. Retrieved 2020-09-30.
- ↑ Yanagihori H, Oyama N, Nakamura K, Kaneko F (2005). "c-kit Mutations in Patients with Childhood-Onset Mastocytosis and Genotype-Phenotype Correlation". J Mol Diagn. 7 (2): 252–7. doi:10.1016/S1525-1578(10)60552-1. PMC 1867517. PMID 15858149. Archived from the original on 2011-12-09. Retrieved 2020-09-30.
- ↑ Sotlar K, Escribano L, Landt O, et al. (2003). "One-Step Detection of c-kit Point Mutations Using Peptide Nucleic Acid-Mediated Polymerase Chain Reaction Clamping and Hybridization Probes". Am. J. Pathol. 162 (3): 737–46. doi:10.1016/S0002-9440(10)63870-9. PMC 1868096. PMID 12598308.
{{cite journal}}: CS1 maint: url-status (link) - ↑ url=https://www.genecards.org/cgi-bin/carddisp.pl?gene=KIT&keywords=C-kit Archived 2016-03-05 at the Wayback Machine
- ↑ Tamhankar, Parag M; Suvarna, Jyoti; Deshmukh, Chandrahas T (2009). "Cutaneous mastocytosis. Getting beneath the skin of the issue: a case report". Cases Journal. 2 (1): 69. doi:10.1186/1757-1626-2-69. ISSN 1757-1626. PMC 2651115. PMID 19154597.
- ↑ "Archive copy". Archived from the original on 2012-02-29. Retrieved 2020-09-30.
{{cite web}}: CS1 maint: archived copy as title (link) - ↑ Fairley JA, Pentland AP, Voorhees JJ (1984). "Urticaria pigmentosa responsive to nifedipine". J. Am. Acad. Dermatol. 11 (4 Pt 2): 740–3. doi:10.1016/S0190-9622(84)70233-7. PMID 6491000.
Further reading
- Alto WA, Clarcq L (June 1999). "Cutaneous and systemic manifestations of mastocytosis". Am Fam Physician. 59 (11): 3047–54, 3059–60. PMID 10392589. Archived from the original on 2011-09-27. Retrieved 2020-09-30.
External links
| Classification | |
|---|---|
| External resources |