This article was co-authored by Peter Gardner, MD. Peter W. Gardner, MD is a board certified physician who has practiced Gastroenterology and Hepatology for over 30 years. He specializes in diseases of the digestive system and liver. Dr. Gardner earned his Bachelor’s degree from the University of North Carolina and attended Georgetown Medical School. He completed his residency in Internal Medicine and then his fellowship in Gastroenterology at the University of Connecticut. He is a previous Chief of Gastroenterology at Stamford Hospital and remains on the staff. He is also on the staff of Greenwich Hospital and New York (Columbia) Presbyterian Hospital. Dr. Gardner is an Approved Consultant in Internal Medicine and Gastroenterology with the American Board of Internal Medicine.
There are 10 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 11,818 times.
In most cases, the little pouches that form in your large intestine, known as diverticula, are not a big deal. If one or more of those pouches becomes infected and inflamed, though, you develop a condition called diverticulitis. Diverticulitis is most readily recognized by the sharp, painful sensations it creates in the lower abdomen. However, since diverticulitis shares so many symptoms with other conditions, you’ll need your doctor to positively diagnose it.[1]
Steps
Identifying Diverticulitis by Yourself
-
1Check for pain in your lower abdomen. The most prominent symptom of diverticulitis is usually sharp, consistent pain in the lower abdomen. This pain may be felt on either side, but tends to occur more on the left.[2] The pain may be persistent for several days, or it may come and go.[3]
- Abdominal pain is usually accompanied by abdominal tenderness. This may be noticeable when someone or something touches your abdomen, when you sneeze, or when you stretch.
-
2Watch for changes in your bowel habits. Both constipation and diarrhea can be signs of diverticulitis. Diverticulitis causes constipation because food cannot pass easily through your bowels, and the bowel walls become constricted. Diarrhea is usually a result of overflow from the resulting constipation. Constipation is more common, but if you experience either of these symptoms in conjunction with lower abdominal pain, you should make an appointment with your health care provider.[4]
- Diverticulitis can also impact how frequently you have a bowel movement, as well as how big the movement is. If you notice substantial changes in your bowel frequency or volume, this could be another symptom of diverticulitis.
Advertisement -
3Monitor your stool for blood. In some cases, diverticulitis may result in blood in your stool. If you have other symptoms of diverticulitis, check for blood before you flush. If you have black or tarry-looking stools or notice blood in your stool, contact a medical professional right away.[5]
- Bleeding from diverticulitis typically occurs high up in the bowel, causing your stools to look tarry or black. Black stools are a more common sign of bleeding in diverticulitis than fresh blood in the toilet.
- Blood in your stool could be indicative of a number of serious medical problems, including diverticulitis. If you see blood when you go, seek medical help as soon as possible to rule out more serious issues such as colon cancer.
-
4Look out for nausea and vomiting. Vomiting is a common symptom of diverticulitis. If you are experiencing unexplained nausea and vomiting, especially in conjunction with severe and persistent abdominal cramps or pain, get medical attention right away.[6]
-
5Take your temperature to check for a fever. In some cases, diverticulitis may cause a fever along with other symptoms.[7] Fevers associated with diverticulitis may also come with nausea, vomiting, or other flu-like symptoms. If you have both abdominal pain or tenderness and a fever, make an appointment with your doctor to screen for diverticulitis.[8]
- A fever is a relatively uncommon symptom of diverticulitis. Abdominal pain, cramping, and vomiting are the most typical symptoms.
- Any temperature over 98.6 °F (37.0 °C) is considered a fever, but fevers generally aren’t considered severe unless they are over 100.4 °F (38.0 °C).
- If you have a high fever, seek treatment at an immediate care or urgent care center right away.
Getting a Medical Diagnosis
-
1Make an appointment for a physical with your health care provider. Screening for diverticulitis generally starts with a standard physical unless you’re experiencing extreme symptoms. Your doctor will check your overall health profile, along with examining your abdomen for tenderness or signs of pain.[9]
- If you are experiencing serious symptoms or severe pain, seek emergency medical treatment right away.
- If you experience sharp pain that is localized to 1 part of your abdomen, this is a sign of a medical emergency. You may experience this type of localized pain with either diverticulitis or appendicitis, and it will be extremely severe (a 10 on the numeric pain scale).
-
2Get a blood and urine test. A basic blood and urine test will help your doctor screen for signs of infection, inflammation, and anemia.[10] You may be able to complete your tests in your doctor’s office, or you may have to go to an affiliated hospital or clinic, depending on your health care provider’s in-house setup.[11]
-
3Have a CT scan done on your GI tract. During a CT scan, an x-ray technician will use a combination of x-rays and computer imaging to create a comprehensive image of your gastrointestinal (GI) tract. This procedure is painless, and requires you to lie on a table that slides into a tunnel to capture the x-rays. The images are then used to check for both diverticulosis and diverticulitis.[12]
- Prior to your scan, your technician may give you a solution to drink and an injection of a dye called a contrast medium. This medium makes it easier to see inside your body during the procedure.
-
4Ask about a colonoscopy. In a colonoscopy, your doctor will use a long, thin, flexible tube with a tiny light and camera attached to it to look inside your colon. This can help them directly identify diverticulosis and diverticulitis, as well as other conditions that may potentially be causing your abdominal pain.[13]
- This is an outpatient procedure, but you will generally be given a sedative or anesthesia to help manage any associated discomfort.
-
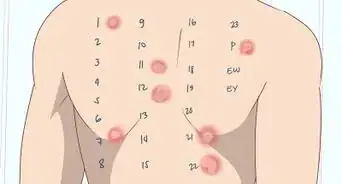
5See if you need a lower GI series. This procedure uses a chalky liquid called barium to make your large intestine more visible on x-rays. During this process, you will lie flat on a table, and your radiologist will use a thin, flexible tube to fill your large intestine with barium. They will then take x-ray images to check for the pouches that cause diverticulitis.[14]
- This procedure may cause some discomfort. Generally, though, the discomfort is not so great that you will need anesthesia.
- The night before your procedure, your doctor may provide you with a set of instructions to help you empty your bowel as much as possible. If they do, follow them closely. The cleaner your bowel, the easier it will be for the scan to detect any issues.
Ruling Out Other Complications
-
1Assess your personal risk level for diverticulitis. Diverticulitis is more likely for some people than it is for others. Take a look at your personal health risk profile to see if you have an increased risk of diverticulitis. If you are low on the diverticulitis risk spectrum but still have abdominal pain, you may have a different condition. Diverticulitis risk factors include:[15]
- Aging. Those over the age of 40 are more likely to develop diverticulitis.
- Obesity and a sedentary lifestyle. Regular exercise lowers the risk of diverticulitis.
- Smoking.
- A diet rich in animal fats.
- Taking certain medications including steroids, opiates, ibuprofen, and naproxen.
-
2Request a liver function test. Liver function tests are blood tests that can help rule out other causes of abdominal pain, such as liver disease or gallstones. Check with your health care provider to see if a liver function test is necessary. If it is, it can often be ordered and completed at the same time as your other blood tests.[16]
-
3Ask about a pelvic exam. Symptoms of diverticulitis can be similar to those associated with pelvic injuries or diseases, such as pelvic inflammatory disease. Talk to your doctor about screening for pelvic disease with a standard pelvic exam.[17]
References
- ↑ Peter Gardner, MD. Board Certified Gastroenterologist. Expert Interview. 25 August 2020.
- ↑ Peter Gardner, MD. Board Certified Gastroenterologist. Expert Interview. 25 August 2020.
- ↑ https://my.clevelandclinic.org/health/diseases/10352-diverticular-disease
- ↑ https://my.clevelandclinic.org/health/diseases/10352-diverticular-disease
- ↑ https://www.nhs.uk/conditions/diverticular-disease-and-diverticulitis/
- ↑ https://www.niddk.nih.gov/health-information/digestive-diseases/diverticulosis-diverticulitis/symptoms-causes
- ↑ Peter Gardner, MD. Board Certified Gastroenterologist. Expert Interview. 25 August 2020.
- ↑ https://www.niddk.nih.gov/health-information/digestive-diseases/diverticulosis-diverticulitis/symptoms-causes
- ↑ https://my.clevelandclinic.org/health/diseases/10352-diverticular-disease
- ↑ https://www.radiologyinfo.org/en/info/diverticulitis
- ↑ https://www.niddk.nih.gov/health-information/digestive-diseases/diverticulosis-diverticulitis/diagnosis
- ↑ https://www.niddk.nih.gov/health-information/digestive-diseases/diverticulosis-diverticulitis/diagnosis
- ↑ https://www.radiologyinfo.org/en/info/diverticulitis
- ↑ https://www.niddk.nih.gov/health-information/diagnostic-tests/lower-gi-series
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6502189/
- ↑ https://medlineplus.gov/lab-tests/liver-function-tests/
- ↑ https://www.aafp.org/afp/2005/1001/p1229.html
About This Article
To diagnose diverticulitis, monitor yourself for common symptoms, like pain in the lower abdomen, constipation or diarrhea, bloody stool, nausea, vomiting, and fever. If you think you have diverticulitis, make an appointment with your doctor so they can do a blood and urine test. They might also recommend a CT scan of your gastrointestinal tract or x-rays of your large intestine. For more advice from our Medical co-author, like how to rule out other possible complications, scroll down!



































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...