This article was co-authored by Muhammad Khan, MD, MPH. Dr. Muhammad Khan is a Gastroenterologist, with over 10 years of experience. Dr. Khan specializes in Pediatric Gastroenterology, Hepatology, and Nutrition, and has a special focus in Therapeutic Endoscopy. He received his Bachelor’s, Master’s, and Doctorate of Medicine degrees from The University of Utah. Dr. Khan completed his residency training at Eastern Virginia Medical School, where he was inducted into the prestigious Alpha Omega Alpha honor society. He then completed his fellowship training at Lucile Packard Children’s Hospital at Stanford University. He is a Fellow of both the American Society of Gastrointestinal Endoscopy (ASGE) and the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition (NASPGHAN).
There are 12 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 21,844 times.
Chronic indigestion (also known as dyspepsia) refers to a medical condition that involves discomfort in the stomach lasting for more than seven days a month. Symptoms of chronic indigestion may gradually worsen, come and go, or last for quite some time. The most common symptom of chronic indigestion is burning pain or discomfort in the upper abdomen. Other possible symptoms include a generalized "upset stomach," feeling full or bloated, belching, nausea, and vomiting. Fortunately, there are some measures that can be taken to help ease the symptoms of chronic indigestion.[1]
Steps
Identifying and Treating the Cause
-
1Recognize the symptoms of indigestion. Though there are many different signs of indigestion, there are a number of key giveaways that can alert you to a problem that needs to be addressed. The most common symptoms reported by sufferers of indigestion include:[2]
- Feeling very full or bloated
- Nausea, and even vomiting
- Excessive burping and belching (beyond what is "normal" for you)
- Regurgitation of the stomach contents or food into the esophagus
- Sharp or intense pain in the stomach
-
2Understand the main causes of chronic indigestion. Indigestion is not a disease or illness itself, but a symptom of an underlying problem with the digestive system. It's important to think about some of the potential causes of your indigestion. As the name suggests, indigestion is most commonly associated with food and drink. Eating too much and too fast, excess alcohol, and consumption of foods that are difficult to digest can all cause abdominal pain.[3] Chronic indigestion, however, can be associated with several other problems, including:[4]
- Functional dyspepsia (no obvious clinical abnormality)
- Stress
- Obesity
- Smoking
- Pregnancy
- Medications (e..g. non-steroidal anti-inflammatories (NSAIDs), aspirin)
- Irritable bowel syndrome (IBS)
- Gastro-esophageal reflux disease (GERD)
- Gastroparesis (failure of the stomach to empty properly)
- Helicobacter pylori infection
- Stomach ulcers
- Cancer of the stomach
Advertisement -
3Cut back or switch medications. Sometimes, chronic indigestion is a side effect of long-term medication use, particularly with NSAIDs (non-steroidal anti-inflammatory drugs), which include aspirin, naproxen (Aleve, Anaprox, Naprelan, Naprosyn), and ibuprofen (Motrin, Advil), among others.
- NSAIDs can cause intestinal problems and discomfort. For this reason, long-term use of these medications is not recommended.
- Iron supplements are also known to be hard on the digestive system and can cause acid reflux, constipation, and an upset stomach.
- Some high blood pressure, anti-anxiety, and antibiotic medications can also cause heartburn, nausea, and indigestion, among other side effects.
- If you suspect that your indigestion is being caused by a particular drug, then consulting your doctor about changing to another medication may be the answer.
-
4Take doctor-recommended antacids to relieve indigestion throughout pregnancy. Pregnancy is often associated with indigestion, perhaps not surprisingly, because of the pressure it exerts on the digestive system due to the growing fetus.[5] Eight out of ten women typically experience indigestion during their pregnancy.[6]
- If the symptoms are mild and are not causing significant pain, you can consider making some changes to your eating and drinking habits (see Part 2). You can also take an over-the-counter antacid, which reduces the production of stomach acid, or an alginate, which helps relieve indigestion caused by acid reflux (when the acid from your stomach leaks back up into the esophagus) In general, you should take an antacid or alginate only when you experience symptoms (rather than as a general everyday medication). See Part 3 for brands.
- Although there is a lot of reluctance and fear surrounding taking medications during pregnancy nowadays, antacids or alginates are safe as long as you take only the recommended dosage. However, feel free to consult your physician if you are still unsure.
-
5Make dietary changes to alleviate chronic indigestion caused by IBS. Chronic indigestion is one of the most common symptoms of IBS (irritable bowel syndrome), a condition characterized by persistent abdominal pain, discomfort, bloating, and alteration of bowel habits. The cause of IBS is unknown and not detectable via any tests.
- The best treatment strongly depends upon the particular symptoms of discomfort experienced by the patient; however dietary changes are often effective in alleviating symptoms.
-
6Seek medical treatment for chronic indigestion cause by GERD. Gastroesophageal reflux disease (GERD) is caused by a persistent, abnormal leakage of the stomach acids back up into the esophagus.[7] The associated indigestion may be treated using medications (see Part 3), lifestyle changes (see Part 2) or even surgery, depending on the severity of the illness.
- It is important to consult your physician if you suspect you may have GERD. If left untreated, GERD can, in the long-term, increase your risk of developing permanent damage and cancer in the esophagus.
-
7Take specific medications to relieve indigestion caused by gastroparesis. Gastroparesis is a condition in which the stomach cannot empty properly as a result of nerve damage. It is sometimes associated with diabetes.
- There is no satisfactory treatment for this condition but metoclopramide, a dopamine antagonist, helps to contract the stomach thus preventing associated symptoms such as indigestion. In this case, you will need to consult a specialist recommended by your physician.
-
8Undergo treatment for your indigestion caused by stomach ulcers or cancer. Stomach ulcers and cancers can only be accurately assessed and treated by competent specialists. Adequate treatment of these problems may help any associated indigestion.
- In the meantime, symptomatic relief can be obtained by consuming antacids, alginates or H2 blockers (see Part 3).
Making Lifestyle Changes
-
1Change your portion sizes and meal times. Eating large meals requires further peristalsis or synchronized movements of the digestive tract in order to digest the food. This can further aggravate the irritation in the intestinal lining. Instead, aim to eat six small frequent meals per day: three major meals (breakfast, lunch, and dinner) and three snacks in between. In addition, make an effort to stop eating about two to three hours before you go to bed.[8]
- Try eating a half-size portion of what you would normally eat at breakfast, lunch, dinner. As a general rule (and one that holds even if you don't suffer from regular indigestion), you should feel satisfied, but not stuffed, after eating.
-
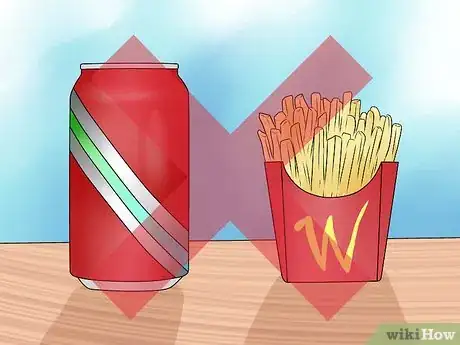
2Avoid food and drinks that can trigger indigestion.[9] A number of foods can irritate the intestines and stomach. Spicy, fatty, and acidic foods are all common culprits and should be cut back on or removed entirely from your diet if you suspect you have digestive pain.[10]
- Avoid fatty foods, like fried food, soft cheese, nuts, red meat, and avocados.[11]
- Avoid spicy food like curries and other sauces with heat to them.
- Avoid tomatoes and tomato-based sauces and citric foods like grapefruits and oranges (as well as in juice form).[12]
- Avoid carbonated drinks, which can unsettle the stomach.
- Eliminate alcohol and caffeine.
- Try cutting a few foods out at a time to see if you can narrow down the culprit. As you remove foods from your everyday diet, see if you notice a change and whether your indigestion has abated.
-
3Do not open your mouth while chewing. Chewing with your mouth open or talking while eating can lead you to swallow excessive amounts of air, which can cause further bloating.
-
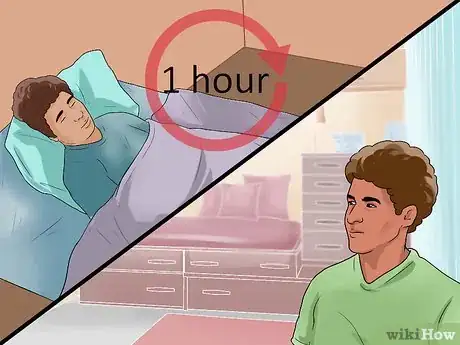
4Consider your posture. Do not lie down or bend over after meals. With the aid of gravity, bending or lying down can lead to the regurgitation of stomach contents or food into the gullet or esophagus. Similarly, avoid wearing clothing, pants or belts that put pressure on the stomach.[13]
- Wait at least one hour after eating before lying down or doing activities that require bending over. If lying down cannot be avoided, elevate the head at an angle of 30 to 45 degrees to help facilitate the digestive system to do its job, breaking down the food.
- If you have chronic indigestion, consider purchasing a wedge pillow to reduce acid reflux while lying down.[14]
-
5Stop smoking. If you smoke, consider quitting if you experience indigestion. The nicotine in cigarettes can cause a relaxing of the muscles at the lower part of the esophagus, thus aiding the stomach acid in its attempt to leak back up. In addition, nicotine is a potent vasoconstrictor. This means it can constrict the intestinal lining, which is inflamed by the irritation of the excessive stomach acid. As a result, abdominal pain can worsen when smoking.[15]
- Quitting smoking of course has numerous other benefits alongside relief from chronic indigestion, including reduced risk for lung cancer and other cancers, heart disease, and stroke.
-
6Cut back on alcohol and caffeine. Alcohol and caffeine can trigger indigestion, and particularly heartburn, because it opens the esophageal sphincter and thus permits the stomach acid to leak back up. Although you may not notice a problem with an individual drink, the effect can be compounded if for example you pair that drink with problem foods on a regular basis (e.g., if you have coffee in the morning, a glass of wine with tomato soup at dinner, and then an orange later).[16]
- Coffee, tea, and soda and other drinks that contain caffeine should also be avoided. You don't have to totally give them up, but you should cut back. Aim for 1-2 small cups (3-4 oz) of coffee a day.
-
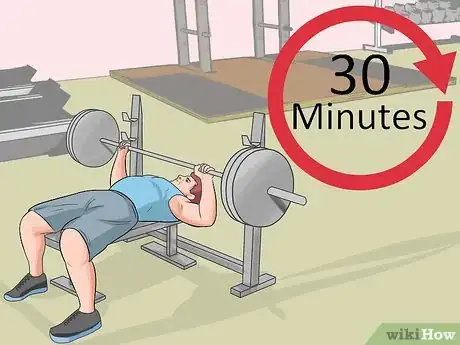
7Lose weight. If you are overweight or obese, you are more likely to suffer from indigestion because of the added pressure in your abdomen. Make a concerted ever to lose weight and see if your indigestion is alleviated.
- Try to eat healthy and regularly.[17] Incorporate more fruits and vegetables and whole grains into your diet. Make sure to limit foods with high acidic content until your symptoms are alleviated.[18]
- Get regular exercise. Try to get at least 30 minutes of moderate to intense activity at least three times a week.[19] It's also a good idea to incorporate strength training into your workouts in order to convert fat into muscle.
Taking Medication
-
1Take an antacid.[20] Easy-to-obtain antacids like Maalox, Rolaids, and Tums contain calcium, magnesium, or aluminum and can help neutralize neutralize or counteract the acid in the stomach to make it less corrosive. Antacids can be purchased over-the-counter at pharmacies and drug stores.[21]
- One of the most prescribed antacids is Maalox. Its recommended dose is one to two tablets four times a day.
- Though some people find these helpful in treating the casual occurrence of heart burn or indigestion, these may not be strong enough in cases of chronic indigestion.
-
2Take acid blockers. One of the main causes of chronic indigestion is excessive stomach acid which leaks upwards into the esophagus and causes discomfort. Acid blockers (also known as H2 blockers) work to reduce the production of stomach acid, thereby making the stomach contents less acidic so that when they do leak into the esophagus, it will be less irritating.
- The most widely recommended H2 blocker is ranitidine, or Zantac, which can be obtained OTC or with a prescription. Ranitidine can be taken orally in tablet form. In general, most H2 blockers are to be taken 30 to 60 minutes before eating (but only twice per day maximum).
- Acid blockers do not act as quickly as antacids but they last longer. In fact, acid blockers can work for several hours and are best used as a preventive measure.
-
3Take proton pump inhibitors (PPIs). Proton pump inhibitors work by blocking a chemical system called the hydrogen-potassium adenosine triphosphatase enzyme system, which produces stomach acids. If the level of stomach acid is low, then the abdominal pain in chronic indigestion can be minimized.[22]
- Physicians recommend PPIs when acid blockers don't provide lasting relief or when you have problems in the esophagus thanks to GERD.
- One PPI called Prilosec is available OTC, whereas others, including Aciphex, Nexium, Prevacid, Protonix, and stronger Prilosec, require prescription.
-
4Take an alginate. Alginates, such as the OTC brand Gaviscon, create a foam barrier that floats on top of the contents of your stomach and keeps your stomach acids from pushing back up to the esophagus. Because they create that barrier between the stomach acid and the esophagus, alginates are especially good at providing relief from acid reflux and heartburn.[23]
- Alginates work faster than H2 blockers and last longer than antacids. They come in both liquid and tablet form, so you should use whatever you prefer.
- You should take alginates when you experience symptoms and not before a meal, since the food passing through the esophagus can disrupt the barrier and make it less effective.
-
5Try Reglan. Reglan, or metoclopramide, increases digestive contractions, which helps to move food through the digestive system and into the intestines. The math is simple: speedier digestive means less heartburn.[24]
- Reglan should only be considered a short-term treatment and only as a last resort when the other medicines mentioned above do not provide sufficient relief. Do not use Reglan for more than 12 weeks.[25]
- Reglan requires a prescription and can be taken in tablet or liquid form, usually 30 minutes before meals and before bed.
-
6Use antidepressants for pain relief. NSAIDs are not given to patients with chronic indigestion to relieve abdominal pain because these drugs can irritate the intestinal lining and may aggravate the condition. Instead, antidepressants are prescribed for pain relief.
- Antidepressants aid in pain relief by reducing the ability of the nerve cells to reabsorb brain chemicals such as serotonin and noradrenaline. These chemicals accumulate outside the nerve cells if they are not reabsorbed. This results in the inhibition of pain messages to the spinal cord.
- Amitriptyline is usually prescribed for this purpose. Its therapeutic dose is 10 to 25 mg daily, which is gradually increased by an increment of 10 or 25 mg each week.[26]
- Always consult your physician about the possibilities of taking an antidepressant for pain relief.
Understanding Diagnostic Procedures
-
1Call your doctor. If you think you are suffering from chronic indigestion, you should seek treatment in order to get relief. The American Gastroenterological Association recommends that you consult your physician if you experience any or a combination of the following symptoms:
- You experience indigestion three or more times every week.
- You've suffered from regular indigestion for four or more years.
- You've used OTC antacids and other medications for a period of several months or longer.
- You have not been able to find relief in spite of various attempts (lifestyle changes, medication, etc.).
- Note that if you experience chest pain, you should call your doctor or emergency services, as this could be a sign of a heart attack that you may be mistaking for heartburn or indigestion.
-
2Get your blood tested. Your doctor will probably want to get a blood sample from you in order to help determine the underlying cause of your indigestion. Common blood tests that are ordered to help diagnoses digestive disorders include a CBC (Complete Blood Count, which measures red and white blood cells as well blood platelets and an ESR (Erythrocyte Sedimentation Rate) or CRP (C-Reactive Protein), which assess the level of inflammation in the body. Blood tests can be used to diagnose and monitor diseases such as IBS, H. pylori, Celiac disease, and Crohn's Disease, among many others.
- A blood sample is drawn from the patient’s vein through a sterile needle and syringe. The sample is put in a sterile container and will be examined in a medical laboratory.
-
3Go for an endoscopy. In some cases, particularly in those where the complaints of indigestion are persistent, your doctor may refer you to a gastroenterologist, a specialist in the area of the gastrointestinal tract and liver. The specialist may opt to conduct an endoscopy, a procedure that enables him to look inside your esophagus to see whether the underlying cause is acid reflux that is damaging the lining of your esophagus.
- In an endoscopy, a medical instrument is inserted into the colon and is guided by a small camera with a lighted tube at its end. This procedure can be performed in one of two ways: colonoscopy or upper endoscopy.
- A colonoscopy utilizes a flexible tube that is gently inserted into the opening of the anus, allowing direct visualization and examination of the colon (the large intestine) and the terminal ileum, the final section of the small intestine.[27]
- An upper endoscopy is aided by a flexible tube inserted through the mouth, down the esophagus and the stomach until it reaches the duodenum, the first part of the small intestine. Usually you will be asked to come in with an empty stomach (meaning no food or drink six or more hours before the procedure).
- During the endoscopy, your doctor may also remove a small piece of tissue to test.[28]
-
4Undergo a barium enema. Your doctor may recommend this if you've been experiencing stomach pain, bleeding from the rectum, and abnormal bowel movements (such as diarrhea or constipation). A barium enema is an X-ray test that can tell if there are any abnormalities in the colon. In this test, a liquid is injected into your rectum that contains a metallic substance called barium. Barium works to coat the lining of the colon so that the colon can be more easily seen on the X-ray.[29]
- Before the exam, you'll have to "empty" your colon because anything remaining could be seen on the X-ray as an abnormality. You will likely be required to fast after midnight and take a laxative in order to clear out your colon.[30] In some cases, your doctor may request that you stick to a special diet the day before (e.g., no solids, only clear liquids like water, broth, and black coffee). A week or two before the test, be sure to ask your doctor about any medications you may be taking and whether you should cease taking them before the exam.
- In general, the exam is uncomfortable, but there are no real side effects from a barium enema, although you may experience white stools (because of the barium) or a bit of constipation. Your doctor may suggest you take a laxative if this is the case.
Expert Q&A
-
QuestionHow can I fix my digestive problems naturally?
 Muhammad Khan, MD, MPHDr. Muhammad Khan is a Gastroenterologist, with over 10 years of experience. Dr. Khan specializes in Pediatric Gastroenterology, Hepatology, and Nutrition, and has a special focus in Therapeutic Endoscopy. He received his Bachelor’s, Master’s, and Doctorate of Medicine degrees from The University of Utah. Dr. Khan completed his residency training at Eastern Virginia Medical School, where he was inducted into the prestigious Alpha Omega Alpha honor society. He then completed his fellowship training at Lucile Packard Children’s Hospital at Stanford University. He is a Fellow of both the American Society of Gastrointestinal Endoscopy (ASGE) and the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition (NASPGHAN).
Muhammad Khan, MD, MPHDr. Muhammad Khan is a Gastroenterologist, with over 10 years of experience. Dr. Khan specializes in Pediatric Gastroenterology, Hepatology, and Nutrition, and has a special focus in Therapeutic Endoscopy. He received his Bachelor’s, Master’s, and Doctorate of Medicine degrees from The University of Utah. Dr. Khan completed his residency training at Eastern Virginia Medical School, where he was inducted into the prestigious Alpha Omega Alpha honor society. He then completed his fellowship training at Lucile Packard Children’s Hospital at Stanford University. He is a Fellow of both the American Society of Gastrointestinal Endoscopy (ASGE) and the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition (NASPGHAN).
Board Certified Gastroenterologist Basically, you have to really watch what you eat and how things are leaving your body. Focus on eating your calories from healthy sources — plants, fruits and vegetables should make up half of it — and on avoiding processed foods. Drink enough water and see a doctor if you're having any problems.
Basically, you have to really watch what you eat and how things are leaving your body. Focus on eating your calories from healthy sources — plants, fruits and vegetables should make up half of it — and on avoiding processed foods. Drink enough water and see a doctor if you're having any problems.
References
- ↑ http://patient.info/health/dyspepsia-indigestion#
- ↑ http://patient.info/health/dyspepsia-indigestion#
- ↑ Peter Gardner, MD. Board Certified Gastroenterologist. Expert Interview. 25 August 2020.
- ↑ http://patient.info/health/dyspepsia-indigestion#
- ↑ Peter Gardner, MD. Board Certified Gastroenterologist. Expert Interview. 25 August 2020.
- ↑ http://www.nhs.uk/conditions/pregnancy-and-baby/pages/indigestion-heartburn-pregnant.aspx#Treatment
- ↑ Peter Gardner, MD. Board Certified Gastroenterologist. Expert Interview. 25 August 2020.
- ↑ Peter Gardner, MD. Board Certified Gastroenterologist. Expert Interview. 25 August 2020.
- ↑ Muhammad Khan, MD, MPH. Board Certified Gastroenterologist. Expert Interview. 24 August 2021.
- ↑ Peter Gardner, MD. Board Certified Gastroenterologist. Expert Interview. 25 August 2020.
- ↑ Muhammad Khan, MD, MPH. Board Certified Gastroenterologist. Expert Interview. 24 August 2021.
- ↑ Muhammad Khan, MD, MPH. Board Certified Gastroenterologist. Expert Interview. 24 August 2021.
- ↑ http://patient.info/health/dyspepsia-indigestion#
- ↑ Peter Gardner, MD. Board Certified Gastroenterologist. Expert Interview. 25 August 2020.
- ↑ http://patient.info/health/dyspepsia-indigestion#
- ↑ http://www.webmd.com/top-10-heartburn-foods?page=2
- ↑ Muhammad Khan, MD, MPH. Board Certified Gastroenterologist. Expert Interview. 24 August 2021.
- ↑ Muhammad Khan, MD, MPH. Board Certified Gastroenterologist. Expert Interview. 24 August 2021.
- ↑ Muhammad Khan, MD, MPH. Board Certified Gastroenterologist. Expert Interview. 24 August 2021.
- ↑ Muhammad Khan, MD, MPH. Board Certified Gastroenterologist. Expert Interview. 24 August 2021.
- ↑ http://patient.info/health/antacids
- ↑ http://www.patient.info/health/proton-pump-inhibitors
- ↑ http://www.nhs.uk/conditions/pregnancy-and-baby/pages/indigestion-heartburn-pregnant.aspx#Treatment
- ↑ https://www.drugs.com/reglan.html
- ↑ http://www.webmd.com/drugs/2/drug-6177/reglan-oral/details
- ↑ http://painconcern.org.uk/amitriptyline/
- ↑ http://www.webmd.com/digestive-diseases-endoscopy
- ↑ http://www.webmd.com/digestive-diseases-endoscopy
- ↑ http://www.mayoclinic.org/tests-procedures/barium-enema/basics/definition/prc-20019174
- ↑ Muhammad Khan, MD, MPH. Board Certified Gastroenterologist. Expert Interview. 24 August 2021.














































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...